Abstract
Background
The hypothalamus plays a central role in the pathophysiology of migraine and is considered to be the “migraine generator.” It participates in initiating a migraine attack through its connectivity to regions of the brain involved in processing and modulating pain. However, the underlying mechanisms of hypothalamic effective functional connectivity that bring about migraines remain unclear. This study investigated the hypothalamus-based directional effective connectivity in migraine without aura patients and assessed associations among the clinical characteristics.
Methods
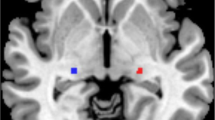
Seven patients with migraine without aura during the attack (MWoA-DA) (four with photophobia (MWoA-DAWP) and three without photophobia (MWoA-DAWoP)), twenty-seven patients with migraine without aura during the interictal period (MWoA-DI), and twenty-nine healthy controls (HC) were included in this study. Granger causality analysis (GCA) was used to investigate the directional effective connectivity between the hypothalamus and other brain regions.
Results
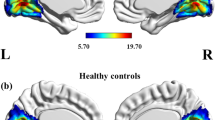
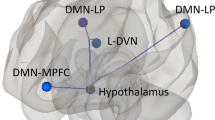
MWoA-DA patients exhibited decreased outflow from the bilateral hypothalamus to the visual cortex compared with the MWoA-DI patients and HCs. The MWoA-DAWP group primarily contributed to this result. The MWoA-DA patients showed decreased outflow from the bilateral hypothalamus to the right inferior parietal gyrus compared with the HCs. The visual analogue scale (VAS) was negatively correlated with abnormal effective functional connectivity from the right hypothalamus to the right inferior parietal gyrus in the MWoA-DA group.
Conclusions
These data provide evidence that the hypothalamus might serve as a central component of a multisystem network implicated in migraine and ictal photophobia, which includes hypothalamus and the visual and trigeminovascular systems.


Similar content being viewed by others
Abbreviations
- MWoA-DA:
-
Migraine without aura during the attack
- MWoA-DI:
-
Migraine without aura during the interictal period
- MWoA-DAWP:
-
Migraine without aura patients during attack with photophobia
- MWoA-DAWoP:
-
Migraine without aura patients during attack without photophobia
- HC:
-
Healthy controls
- GCA:
-
Granger causality analysis
- FC:
-
Functional connectivity
- VAS:
-
Visual analogue scale
- MIDAS:
-
Migraine Disability Assessment Scale
- HIT-6:
-
Headache Impact Test
- SF-MPQ-2:
-
Short-form McGill Pain Questionnaire-2 scores
- CSD:
-
Cortical spreading depression
- HP:
-
Hypothalamus
- IPG:
-
Inferior parietal gyrus
References
Headache Classification Committee of the International Headache S (2013) The International Classification of Headache Disorders, 3rd edition (beta version). 33(9):629–808
Global Burden of Disease Study C (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386(9995):743–800
Charles ACSM (2013) Baca, Cortical spreading depression and migraine. Nat Rev Neurol 9(11):637–644
Edvinsson L, Haanes KA, Warfvinge K (2019) Does inflammation have a role in migraine? Nat Rev Neurol 15(8):483–490
Akerman S, Holland R, Goadsby J (2011) Diencephalic and brainstem mechanisms in migraine. Nat Rev Neurosci 12(10):570–584
Maniyar FH et al (2014) Brain activations in the premonitory phase of nitroglycerin-triggered migraine attacks. Brain 137(Pt 1):232–241
Schulte LHA (2016) May, The migraine generator revisited: continuous scanning of the migraine cycle over 30 days and three spontaneous attacks. Brain 139(Pt 7):1987–1993
Schulte LH, Mehnert J, May A (2020) Longitudinal neuroimaging over 30 days: temporal characteristics of migraine. Ann Neurol 87(4):646–651
Denuelle M et al (2007) Hypothalamic activation in spontaneous migraine attacks. Headache 47(10):1418–1426
Meylakh N et al (2020) Altered regional cerebral blood flow and hypothalamic connectivity immediately prior to a migraine headache. Cephalalgia 40(5):448–460
Lerebours F et al (2019) Functional connectivity of hypothalamus in chronic migraine with medication overuse. Cephalalgia 39(7):892–899
Schulte LH, Allers A, May A (2017) Hypothalamus as a mediator of chronic migraine: Evidence from high-resolution fMRI. Neurology 88(21):2011–2016
Buchel CK (2000) Friston, Assessing interactions among neuronal systems using functional neuroimaging. Neural Netw 13(8–9):871–882
Moulton EA et al (2014) Altered hypothalamic functional connectivity with autonomic circuits and the locus coeruleus in migraine. PLoS ONE 9(4):e95508
Schulte LH et al (2020) The migraineur’s brain networks: continuous resting state fMRI over 30 days. Cephalalgia 40(14):1614–1621
Roebroeck A, Formisano E, Goebel R (2005) Mapping directed influence over the brain using Granger causality and fMRI. Neuroimage 25(1):230–242
Deshpande GX (2012) Hu, Investigating effective brain connectivity from fMRI data: past findings and current issues with reference to Granger causality analysis. Brain Connect 2(5):235–245
Huang X et al (2021) Altered amygdala effective connectivity in migraine without aura: evidence from resting-state fMRI with Granger causality analysis. J Headache Pain 22(1):25
Wang T et al (2016) Altered resting-state ascending/descending pathways associated with the posterior thalamus in migraine without aura. NeuroReport 27(4):257–263
Zhu Y et al (2021) Alterations in Effective Connectivity of the Hippocampus in Migraine without Aura. J Pain Res 14:3333–3343
Yan CG et al (2016) DPABI: Data Processing & Analysis for (Resting-State) Brain Imaging. Neuroinformatics 14(3):339–351
Cao Z et al (2022) Decreased gray matter volume in the frontal cortex of migraine patients with associated functional connectivity alterations: a VBM and rs-FC study. Pain Res Manag 2022:2115956
Messina R et al (2021) Clinical correlates of hypothalamic functional changes in migraine patients. Cephalalgia :3331024211046618
Zang ZX et al (2012) Granger causality analysis implementation on MATLAB: a graphic user interface toolkit for fMRI data processing. J Neurosci Methods 203(2):418–426
M A, S D et al (2017) Exploring connectivity with large-scale Granger causality on resting-state functional MRI. J Neurosci Methods 287:68–79
Puledda F et al (2019) Imaging the visual network in the migraine spectrum. Front Neurol 10:1325
Jin C et al (2013) Structural and functional abnormalities in migraine patients without aura. NMR Biomed 26(1):58–64
Wang JJ et al (2016) Amplitude of low-frequency fluctuation (ALFF) and fractional ALFF in migraine patients: a resting-state functional MRI study. Clin Radiol 71(6):558–564
Wei HL et al (2021) Functional connectivity of the visual cortex differentiates anxiety comorbidity from episodic migraineurs without aura. J Headache Pain 22(1):40
Zhang L et al (2021) Altered metabolites in the occipital lobe in migraine without aura during the attack and the interictal period. Front Neurol 12:656349
Thiebaut de Schotten M et al (2014) Subdivision of the occipital lobes: an anatomical and functional MRI connectivity study. Cortex 56:121–37
May AR (2019) Burstein, Hypothalamic regulation of headache and migraine. Cephalalgia 39(13):1710–1719
Zielman R et al (2017) Cortical glutamate in migraine. Brain 140(7):1859–1871
Kamali A et al (2020) A direct visuosensory cortical connectivity of the human limbic system. Dissecting the trajectory of the parieto-occipito-hypothalamic tract in the human brain using diffusion weighted tractography. Neurosci Lett 728:134955
Coppola G et al (2020) Increased neural connectivity between the hypothalamus and cortical resting-state functional networks in chronic migraine. J Neurol 267(1):185–191
Wei HL et al (2019) Impaired intrinsic functional connectivity between the thalamus and visual cortex in migraine without aura. J Headache Pain 20(1):116
Messina R et al (2018) Gray matter volume modifications in migraine: a cross-sectional and longitudinal study. Neurology 91(3):e280–e292
Boulloche N et al (2010) Photophobia in migraine: an interictal PET study of cortical hyperexcitability and its modulation by pain. J Neurol Neurosurg Psychiatry 81(9):978–984
Denuelle M et al (2011) A PET study of photophobia during spontaneous migraine attacks. Neurology 76(3):213–218
Rossi HL, Recober A (2015) Photophobia in primary headaches. Headache 55(4):600–604
Munjal S et al (2020) Most bothersome symptom in persons with migraine: results from the migraine in America Symptoms and Treatment (MAST) study. Headache 60(2):416–429
Schulte LHK (2019) Peng, Current understanding of premonitory networks in migraine: A window to attack generation. Cephalalgia 39(13):1720–1727
Wilkins AJ et al (2021) Photophobia in migraine: a symptom cluster? Cephalalgia 41(11–12):1240–1248
Mulleners WM et al (2001) Visual cortex excitability in migraine with and without aura. Headache 41(6):565–572
Brighina F et al (2015) Visual cortex hyperexcitability in migraine in response to sound-induced flash illusions. Neurology 84(20):2057–2061
Noseda R et al (2017) Neural mechanism for hypothalamic-mediated autonomic responses to light during migraine. Proc Natl Acad Sci U S A 114(28):E5683–E5692
Artemenko AR et al (2022) Migraine and light: a narrative review. Headache 62(1):4–10
Noseda R, Copenhagen D, Burstein R (2019) Current understanding of photophobia, visual networks and headaches. Cephalalgia 39(13):1623–1634
Hayne DR (2019) Martin, Relating photophobia, visual aura, and visual triggers of headache and migraine. Headache 59(3):430–442
Vincent MBN (2007) Hadjikhani, Migraine aura and related phenomena: beyond scotomata and scintillations. Cephalalgia 27(12):1368–1377
Vincent MB (2015) Vision and migraine. Headache 55(4):595–599
Hadjikhani NM (2019) Vincent, Neuroimaging clues of migraine aura. J Headache Pain 20(1):32
Corno S et al (2018) The brain effect of the migraine attack: an ASL MRI study of the cerebral perfusion during a migraine attack. Neurol Sci 39(Suppl 1):73–74
Qin ZX et al (2020) Altered resting-state functional connectivity between subregions in the thalamus and cortex in migraine without aura. Eur J Neurol 27(11):2233–2241
Wei HL et al (2020) Impaired functional connectivity of limbic system in migraine without aura. Brain Imaging Behav 14(5):1805–1814
Tian Z et al (2021) Acupuncture modulation effect on pain processing patterns in patients with migraine without aura. Front Neurosci 15:729218
Yu ZB et al (2016) Different mean thickness implicates involvement of the cortex in migraine. Medicine (Baltimore) 95(37):e4824
Coppola G et al (2015) Evidence for brain morphometric changes during the migraine cycle: a magnetic resonance-based morphometry study. Cephalalgia 35(9):783–791
Liu J et al (2012) Hierarchical alteration of brain structural and functional networks in female migraine sufferers. PLoS ONE 7(12):e51250
Chen N et al (2015) Functional alterations of pain processing pathway in migraine patients with cutaneous allodynia. Pain Med 16(6):1211–1220
Hu B et al (2019) Multi-modal MRI reveals the neurovascular coupling dysfunction in chronic migraine. Neuroscience 419:72–82
Schwedt TJCD (2014) Chong, Correlations between brain cortical thickness and cutaneous pain thresholds are atypical in adults with migraine. PLoS ONE 9(6):e99791
Acknowledgements
We would like to thank the volunteers for their involvement in the study.
Funding
This study was supported by Science and Technology Planning Project of Traditional Chinese Medicine of Zhejiang Province (grant number 2021ZB101) and Medical and Health Research Project of Zhejiang Province (grant number 2020KY665).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Statement of ethics
The study was carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) and was approved by the Ethics Committee of the first Affiliated Hospital of Zhejiang Chinese Medical University.
Conflict of interest
The authors declare no competing interests.
Ethical approval and Informed consent
The study was carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) and was approved by the Ethics Committee of the first Affiliated Hospital of Zhejiang Chinese Medical University (2018-KL-081-02).
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, L., Yu, W., Xu, M. et al. The hypothalamus may mediate migraine and ictal photophobia: evidence from Granger causality analysis. Neurol Sci 43, 6021–6030 (2022). https://doi.org/10.1007/s10072-022-06245-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06245-y