Abstract
Background
The use of prophylactic anti-seizure medications (ASMs) in the management of patients with spontaneous intracerebral hemorrhage (sICH) and aneurysmal subarachnoid hemorrhage (aSAH) is controversial.
Objective
The purpose of this survey was to better characterize the current state of prophylactic ASM use in sICH and aSAH in North America.
Methods
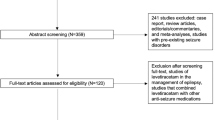
US and Canadian neurosurgeons, neurologists, and interventional neuroradiologists with an interest in or expertise in the management of neurovascular disease were surveyed using an electronic survey tool.
Results
Seven hundred ninety-four survey requests were sent; responses were received from 103 (13%). The majority of respondents were neurosurgeons (84%). Thirty-eight percent of respondents self-identified as vascular neurosurgeons and 10% self-identified as neurocritical care specialists. Seventy-two percent were in academic practice. When asked their preference for ASM prophylaxis (aSAH, sICH, or both), the most common response was to use prophylaxis in both aSAH and sICH (43, 45%). Twenty-one (22%) did not use routine prophylaxis, while 22 (23%) used prophylaxis only in aSAH and 9 (9%) only in sICH. The majority of practitioners (35, 67%) who answered that they used ASM prophylaxis in sICH, used ASMs selectively. For aSAH, the vast majority (53, 82%) used prophylaxis for all patients. Respondents felt that they were more likely to use ASMs for sICH patients if the sICH was in a cortical location, supratentorial location, or was related to a structural abnormality (e.g., tumor, arteriovenous malformation) Levetiracetam (Keppra) was the most commonly used ASM (73, 99%). When asked whether the statement “Current AHA/ASA Guidelines recommend against the use of prophylactic anticonvulsants in spontaneous ICH” was true or false, 78 (83%) responded correctly that the recommendation is true. Only 24 respondents answered the question as to whether they would be willing to randomize sICH and/or aSAH patients to management with or without ASM prophylaxis. Of these, 13 (54%) said they would be willing to randomize sICH patients, while only 6 (25%) were willing to randomize aSAH patients. There were no statistically significant differences in responses to survey questions when analyzed by practice type (academic versus non-academic) or physician specialty (critical care versus non-critical care, or vascular neurology/neurosurgery versus other).
Conclusion
The use of ASMs for seizure prophylaxis after sICH and aSAH remains widespread despite the lack of any specific evidence-based guideline to support the practice. A large-scale randomized controlled trial is needed to add clarity to the practice of prophylactic ASM use in patients with spontaneous intracranial hemorrhage.


Similar content being viewed by others
References
Hemphill III JC, Greenberg SM, Anderson CS, et al. and on behalf of the American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, and Council on Clinical Cardiology (2015) Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 46:2032–2060
Connolly ES Jr, Rabinstein AA, Carhuaporna JR et al (2012) Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 43:1711–1737
Mackey J, Blatsioris AD, Moser EAS et al (2017) Prophylactic anticonvulsants in intracerebral hemorrhage. Neurocrit Care 27(2):220–228. https://doi.org/10.1007/s12028-017-0385-8
Christie C, Daggubati L, Patel N, Matthews N, Lehman E, Cockroft KM (2020) The role of newer generation anticonvulsant prophylaxis on seizures post intracerebral hemorrhage. World Neurosurg 141:e461–e465
Zandieh A, Messé SR, Cucchiara B, Mullen MT, Kasner SE on behalf of the VISTA-ICH Collaborators (2016) Prophylactic use of anti-epileptic drugs in patients with spontaneous intracerebral hemorrhage. J Stroke Cerebrovasc Dis 25(9):2159–2166. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.05.026
Srinivasan S, Shinb H, Chou SHY, Page B, Pennell PB, Dworetzky BA, Lee JW (2013) Seizures and antiepileptic drugs in patients with spontaneous intracerebral hemorrhages. Seizure 22(7):512–516
Spoelhof B, Sanchez-Bautista J, Zorrilla-Vaca A et al (2019) Impact of antiepileptic drugs for seizure prophylaxis on short and long-term functional outcomes in patients with acute intracerebral hemorrhage: a meta-analysis and systematic review. Eur J Epilepsy 69:140–146. https://doi.org/10.1016/j.seizure.2019.04.017
Cotton BA, Kao LS, Kozar R, Holcomb JB (2011) Cost-utility analysis of levetiracetam and phenytoin for posttraumatic seizure prophylaxis. J Trauma Injury Infect Crit Care 71(2):375–379
Martens J, de Jong G, Rovers M, Westert G, Bartels R (2018) Importance and presence of high-quality evidence for clinical decisions in neurosurgery: international survey of neurosurgeons. Interact J Med Res 7(2):e16. https://doi.org/10.2196/ijmr.9617
Staartjes VE, Stumpo V, Kernbach JM et al (2020) Machine learning in neurosurgery: a global survey. Acta Neurochir 162:3081–3091
Benzil DL, Muraszko KM, Soni P, Air EL, Orrico KO, Rutka JT (2020) Toward an understanding of sexual harassment in neurosurgery. J Neurosurg. https://doi.org/10.3171/2020.6.JNS201649
Khalafallah AM, Shravika L, Gami A, Dornbos DL 3rd, Sivakumar W, Johnson JN, Mukherjee D (2020) Burnout and career satisfaction among attending neurosurgeons during the COVID-19 pandemic. Clin Neurol Neurosurg 198:106193
Attenello FJ, Buchanan IA, Wen T et al (2018) Factors associated with burnout among US neurosurgery residents: a nationwide survey. J Neurosurg 129(5):1349–1363. https://doi.org/10.3171/2017.9.JNS17996
Acknowledgements
The authors wish to thank Sara Langan for her assistance in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
Our institution’s Human Subjects Protection Office determined that this project did not require formal institutional review board (IRB) review because the study met the criteria for exempt research according to the policies of our institution and the provisions of applicable federal regulations (IRB 00,014,015).
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gigliotti, M.J., Srikanth, S. & Cockroft, K.M. Patterns of prophylactic anticonvulsant use in spontaneous intracerebral and subarachnoid hemorrhage: results of a practitioner survey. Neurol Sci 43, 1873–1877 (2022). https://doi.org/10.1007/s10072-021-05588-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05588-2