Abstract
Background
Although abnormal movements and postures are the hallmark of dystonia, non-motor symptoms (NMS) are common and negatively affect quality of life.
Objectives
The aim of this study was to screen dystonia patients for NMS and analyze their association with clinical parameters, including motor disability.
Methods
Adult patients with idiopathic isolated dystonia were interviewed and examined. Dystonia severity was evaluated with the Fahn-Marsden Dystonia Rating Scale and the presence of NMS was assessed using a list of 29 complaints.
Results
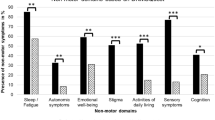
A hundred and two patients (63.7% female) were enrolled. Dystonia began after 20 years of age in 61.8% and was focal or segmental in 82.8% of patients. Only eight patients (7.8%) had no NMS and 59.8% reported more than five. The most prevalent NMS were pain (72.5%) and anxiety (63.7%), followed by difficulty recalling information (44.1%), sadness/anhedonia (41.2%), and difficulty falling asleep (38.2%). No correlation was found between the total number of NMS and dystonia severity (p = 0.18) or regular botulinum toxin use (p = 0.66). The majority of NMS domains correlated with each other.
Conclusions
Our results confirm a high prevalence of NMS among dystonia patients, even in those with mild motor disability. The pathophysiology of NMS in dystonia remains to be completely understood.
Similar content being viewed by others
References
Albanese A, Bathia K, Bressman SB, DeLong MR, Fahn S, Fung VSC et al (2013) Phenomenology and classification of dystonia: a consensus update. Mov Disord 28:863–873. https://doi.org/10.1002/mds.25475
Torres JAKL, Rosales RL (2017) Nonmotor symptoms in dystonia. Int Rev Neurobiol 134:1335–1371. https://doi.org/10.1016/bs.irn.2017.05.003
Han V, Skorvanek M, Smit M, Koprusakova MT, Hoekstra T, van Dijk JP et al (2020) Prevalence of non-motor symptoms and their association with quality of life in cervical dystonia. Acta Neurol Scand 142:613–622. https://doi.org/10.1111/ane.13304
Eggink H, Coenen MA, de Jong R, Toonen RF, Eissens MH, Veenstra WS et al (2019) Motor and non-motor determinants of health-related quality of life in young dystonia patients. Parkinsonism Relat Disord 58:50–55. https://doi.org/10.1016/j.parkreldis.2018.08.008
Novaretti N, Cunha AL, Bezerra TC, Pereira MA, Oliveira DS, Brito MM (2019) The prevalence and correlation of non-motor symptoms in adult patients with idiopathic focal or segmental dystonia. Tremor Other Hiperkinet Mov (NY) 9:596. https://doi.org/10.7916/fhnv-v355
Chaudhuri KR, Prieto-Jurcynska C, Naidu Y, Mitra T, Frades-Payo B, Tluk S et al (2010) The nondeclaration of nonmotor symptoms of Parkinson’s disease to health care professionals: an international study using the nonmotor symptoms questionnaire. Mov Disord 25:704–709. https://doi.org/10.1002/mds.22868
Klingelhoefer L, Chaudhuri KR, Kamm C, Martinez-Martin P, Bathia K, Sauerbier A et al (2019) Validation of a self-completed Dystonia Non-Motor Symptoms Questionnaire. Ann Clin Transl Neurol 6:2054–2065. https://doi.org/10.1002/acn3.50900
Li S, Wang L, Yang Y, Qiao L, Zhang D, Wan X (2020) Non-motor symptoms in Chinese patients with isolated generalized dystonia. Front Neurol 11:209. https://doi.org/10.3389/fneur.2020.00209
Ferrazzano G, Berardelli I, Conte A, Baione V, Concolato C, Belvisi D et al (2019) Motor and non-motor symptoms in blepharospasm: clinical and pathophysiological implications. J Neurol 266:2780–2785. https://doi.org/10.1007/s00415-019-09484-w
Yang J, Shao N, Song W, Wei Q, Ou R, Wu Y et al (2016) Nonmotor symptoms in primary adult-onset cervical dystonia and blepharospasm. Brain Behav 7:e00592. https://doi.org/10.1002/brb3.592
Burke RE, Fahn S, Marsden CD, Bressman SB, Moskowitz C, Friedman J (1985) Validity and reliability of a rating scale for the primary torsion dystonias. Neurology 35:73–77. https://doi.org/10.1212/wnl.35.1.73
Chaudhuri KR, Martinez-Martin P, Schapira AH, Stocchi F, Sethi K, Odin P et al (2006) International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson’disease: the NMSQuest study. Mov Disord 21:916–923. https://doi.org/10.1002/mds.20844
Chaudhuri KR, Sauerbier A, Rojo JM, Sethi K, Schapira AHV, Brown RG et al (2015) The burden of non-motor symptoms in Parkinson’s disease using a self-completed non-motor questionnaire: a simple grading system. Parkinsonism Relat Disord 21:287–291. https://doi.org/10.1016/j.parkreldis.2014.12.031
Kuyper DJ, Parra V, Aerts S, Okun MS, Kluger BM (2011) Nonmotor manifestations of dystonia: a systematic review. Mov Disord 26:1206–1217. https://doi.org/10.1002/mds.23709
Tinazzi M, Squintani GM, Bhatia KP, Segatti A, Donato F, Valeriani M et al (2019) Pain in cervical dystonia: evidence of abnormal inhibitory control. Parkinsonism Relat Disord 65:252–255. https://doi.org/10.1016/j.parkreldis.2019.06.009
Stamelou M, Edwards MJ, Hallett M, Bhatia KP (2012) The non-motor syndrome of primary dystonia: clinical and pathophysiological implications. Brain 135:1668–1681. https://doi.org/10.1093/brain/awr224
Zurowski M, McDonald WM, Fox S, Marsh L (2013) Psychiatric comorbidities in dystonia: emerging concepts. Mov Disord 28:914–920. https://doi.org/10.1002/mds.25501
Conte A, Berardelli I, Ferrazzano G, Pasquini M, Berardelli A, Fabbrini G (2016) Non-motor symptoms in patients with adult-onset focal dystonia: sensory and psychiatric disturbances. Parkinsonism Relat Disord 22:S111-114. https://doi.org/10.1016/j.parkreldis.2015.09.001
Niccolai L, Aita SL, Walker WC, Martin RC, Clay OJ, Crowe M et al (2020) An examination of the neurocognitive profile and base rate of performance impairment in primary dystonia. J Clin Neurosci 74:1–5. https://doi.org/10.1016/j.jocn.2019.12.050
Shukla AW, Brown R, Heese K, Jones J, Rodriguez RL, Malaty IM et al (2016) High rates of fatigue and sleep disturbances in dystonia. Int J Neurosci 126:928–935. https://doi.org/10.3109/00207454.2015.1085035
Hertenstein E, Tang NKY, Bernstein CJ, Nissen C, Underwood MR, Sandhu HK (2016) Sleep in patients with primary dystonia: a systematic review on the state of research and perspectives. Sleep Med Rev 26:95–107. https://doi.org/10.1016/j.smrv.2015.04.004
Marek M, Grobe-Einsler N, Bedarf JR, Wabbels B, Paus S (2018) Sexual dysfunction in cervical dystonia and blepharospasm. Neuropsychiatr Dis Treat 14:2847–2852. https://doi.org/10.2147/NDT.S175193
Hentschel F, Dressler D, Abele M, Paus S (2016) Impaired heart rate variability in cervical dystonia is associated to depression. J Neural Transm 124:245–251. https://doi.org/10.1007/s00702-016-1639-x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Research Ethics Committee of each participating institution and informed written consent was obtained from all patients.
Conflict of interest
Francisco Pereira da Silva-Júnior - employment: Hospital Israelita Albert Einstein, São Paulo-SP, Brazil.
Camila Oliveira dos Santos Alves - none.
Sônia Maria Cesar Azevedo Silva - none.
Vanderci Borges - none.
Henrique Ballalai Ferraz - none.
Maria Sheila Guimarães Rocha - none.
João Carlos Papaterra Limongi - none.
Egberto Reis Barbosa - none.
Patrícia de Carvalho Aguiar - employment: Hospital Israelita Albert Einstein, São Paulo-SP, Brazil and grants: FAPESP 2017/24022-4.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
da Silva-Júnior, F.P., dos Santos Alves, C.O., Silva, S.M.C.A. et al. High prevalence of self-reported non-motor symptoms and lack of correlation with motor severity in adult patients with idiopathic isolated dystonia. Neurol Sci 43, 1061–1065 (2022). https://doi.org/10.1007/s10072-021-05452-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05452-3