Abstract
Objectives
We aimed to (i) analyse the clinical characteristics, treatment outcome and long-term prognosis of anti-NMDAR encephalitis and (ii) study the differences between paediatric and adult patients.
Methods
This was a chart review of all patients with anti-NMDAR encephalitis.
Results
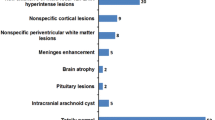
There were 28 patients with 18 patients belonging to the paediatric (<18 years) age group. There was female (94%) preponderance in the paediatric age group, while in adult patients, there was no gender predilection (p=0.006). There was no significant difference in clinical feature, outcome or number of relapses between paediatric and adult population groups. MRI brain was abnormal in 53% of patients. Among the 15 patients with MRI abnormalities at the onset, 53% had poor functional outcome at 1 year, while in 12 patients with normal initial MRI brain, only 8% had poor functional outcome at 1 year (p =0.01). Nearly 53% of patients with abnormal MRI at presentation had at least one clinical relapse within 2 years while in patients with normal MRI at presentation, 15% had a clinical relapse (p=0.037). EEG abnormalities were noticed in 71% of patients; among them, 40 and 15% had poor functional outcome at 1 and 2 years respectively. In comparison, those with normal first EEG at onset, 12% had poor functional outcome at 2 years (p=0.57).
Conclusions
Both paediatric and adult patients presented with similar clinical features but the paediatric population had female preponderance. The functional outcome and number of relapse were comparable in both the paediatric and adult groups. Patients with parenchymal changes on MRI and abnormal EEG showed poorer response compared to those with normal MRI and/or EEG at the onset. Patients have lesser severity of symptoms at relapse than in the first episode. An early diagnosis and treatment are essential for better long-term functional outcome.



Similar content being viewed by others
References
Vitaliani R, Mason W, Ances B, Zwerdling T, Jiang Z, Dalmau J (2005) Paraneoplastic encephalitis, psychiatric symptoms, and hypoventilation in ovarian teratoma. Ann Neurol 58(4):594–604
Dalmau J, Tüzün E, Wu HY, Masjuan J, Rossi JE, Voloschin A, Baehring JM, Shimazaki H, Koide R, King D, Mason W, Sansing LH, Dichter MA, Rosenfeld MR, Lynch DR (2007) Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol 61(1):25–36. https://doi.org/10.1002/ana.21050
Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, Dessain SK, Rosenfeld MR, Balice-Gordon R, Lynch DR (2008) Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 7(12):1091–1098. https://doi.org/10.1016/S1474-4422(08)70224-2
Ryan-florance N, Davis RL, Lam C et al (2009) Key elements for making product value offerings comprehendible in value-based selling. Ann Neurol 66(1):11–18. https://doi.org/10.1002/ana.21756
Granerod J, Ambrose HE, Davies NWS, Clewley JP, Walsh AL, Morgan D, Cunningham R, Zuckerman M, Mutton KJ, Solomon T, Ward KN, Lunn MP, Irani SR, Vincent A, Brown DW, Crowcroft NS, UK Health Protection Agency (HPA) Aetiology of Encephalitis Study Group (2010) Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis 10(12):835–844. https://doi.org/10.1016/S1473-3099(10)70222-X
Kamble N, Netravathi M, Saini J, Mahadevan A, Yadav R, Nalini A, Pal PK, Satishchandra P (2015) Clinical and imaging characteristics of 16 patients with autoimmune neuronal synaptic encephalitis. Neurol India 63(5):687–696. https://doi.org/10.4103/0028-3886.166532
Irani SR, Bera K, Waters P, Zuliani L, Maxwell S, Zandi MS, Friese MA, Galea I, Kullmann DM, Beeson D, Lang B, Bien CG, Vincent A (2010) N-methyl-d-aspartate antibody encephalitis: temporal progression of clinical and paraclinical observations in a predominantly non-paraneoplastic disorder of both sexes. Brain. 133(6):1655–1667. https://doi.org/10.1093/brain/awq113
Titulaer MJ, McCracken L, Gabilondo I, Armangué T, Glaser C, Iizuka T, Honig LS, Benseler SM, Kawachi I, Martinez-Hernandez E, Aguilar E, Gresa-Arribas N, Ryan-Florance N, Torrents A, Saiz A, Rosenfeld MR, Balice-Gordon R, Graus F, Dalmau J (2013) Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol 12(2):157–165. https://doi.org/10.1016/S1474-4422(12)70310-1
Iizuka T, Kaneko J, Tominaga N, Someko H, Nakamura M, Ishima D, Kitamura E, Masuda R, Oguni E, Yanagisawa T, Kanazawa N, Dalmau J, Nishiyama K (2016) Association of progressive cerebellar atrophy with long-term outcome in patients with anti-N-methyl-D-aspartate receptor encephalitis. JAMA Neurol 73(6):706–713. https://doi.org/10.1001/JAMANeurol.2016.0232
Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, Cortese I, Dale RC, Gelfand JM, Geschwind M, Glaser CA, Honnorat J, Höftberger R, Iizuka T, Irani SR, Lancaster E, Leypoldt F, Prüss H, Rae-Grant A, Reindl M, Rosenfeld MR, Rostásy K, Saiz A, Venkatesan A, Vincent A, Wandinger KP, Waters P, Dalmau J (2016) A clinical approach to the diagnosis of autoimmune encephalitis. Lancet Neurol 15(4):391–404. https://doi.org/10.1016/S1474-4422(15)00401-9
DeSena A, Graves D, Warnack W, Greenberg BM (2014) Herpes simplex encephalitis as a potential cause of anti-N-methyl-D-aspartate receptor antibody encephalitis: Report of 2 cases. JAMA Neurol 71(3):344–346. https://doi.org/10.1001/JAMANeurol.2013.4580
Neo S, Yeo T, Chen Z, Ngiam NHW, Lim ETX, Tan K, Lim TCC (2020) Journal of the Neurological Sciences Acute radiological features facilitate diagnosis and prognosis of anti-N-methyl-D-aspartate receptor (NMDAR) and anti-voltage-gated potassium channel (VGKC) encephalitis in adults Acute radiological features facilitate. J Neurol Sci 419(October):117216. https://doi.org/10.1016/j.jns.2020.117216
Wu S, Li H, Lian Y, Chen Y, Zheng Y, Wang C, Zhang Q, Huang Z, Mao Z, Pang K (2020) Anti-N-methyl-D-aspartate receptor encephalitis: a prospective study focused on cerebrospinal fluid and clinical symptoms. Neurol Sci 41(11):3255–3263. https://doi.org/10.1007/s10072-020-04451-0
Shaik R, Netravathi M, Nitish L, Mani RS, Shah P, Damodar T, Anita M, Pal PK (2018) A rare case of Japanese encephalitis-induced anti-N-methyl-d-aspartate receptor encephalitis. Neurol India 66(5):1495–1496. https://doi.org/10.4103/0028-3886.241335
Dabner M, McCluggage WG, Bundell C et al (2012) Ovarian teratoma associated with anti-n-methyl D-aspartate receptor encephalitis: a report of 5 cases documenting prominent intratumoral lymphoid infiltrates. Int J Gynecol Pathol 31(5):429–437. https://doi.org/10.1097/PGP.0b013e31824a1de2
Tüzün E, Zhou L, Baehring JM, Bannykh S, Rosenfeld MR, Dalmau J (2009) Evidence for antibody-mediated pathogenesis in anti-NMDAR encephalitis associated with ovarian teratoma. Acta Neuropathol 118(6):737–743. https://doi.org/10.1007/s00401-009-0582-4
Pruetarat N, Netbaramee W, Pattharathitikul S, Veeravigrom M (2019) Clinical manifestations, treatment outcomes, and prognostic factors of pediatric anti-NMDAR encephalitis in tertiary care hospitals: A multicenter retrospective/prospective cohort study. Brain and Development 41(5):436–442. https://doi.org/10.1016/j.braindev.2018.12.009
Kümpfel T, Havla J, Schuh E et al (2011) Long-term follow-up of patients with neuromyelitis optica treated with rituximab. Neurology. 18(4):293 http://n.neurology.org/content/76/15/1310.short
I G. Analysis of relapses in anti-NMDAR encephalitis_Supplemental info. Neurology. Published online 2011:2-14
Lancaster E, Dalmau J (2012) Neuronal autoantigens-pathogenesis, associated disorders and antibody testing. Nat Rev Neurol 8(7):380–390. https://doi.org/10.1038/nrneurol.2012.99
Vause HE, Chapman MR (2011) Anti-NMDA Receptor Encephalitis: Diagnosis, Psychiatric Presentation, and Treatment. Am J Psychiatry 168(3):245–251
Data and materials availability
The anonymised data of each patient are available with unique alphanumeric code that will be shared if required by the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
None.
Conflict of interest
The authors declare no any financial disclosure or conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Raja, P., Shamick, B., Nitish, L.K. et al. Clinical characteristics, treatment and long-term prognosis in patients with anti-NMDAR encephalitis. Neurol Sci 42, 4683–4696 (2021). https://doi.org/10.1007/s10072-021-05174-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05174-6