Abstract
Purpose
To summarize the clinical characteristics of patients with sporadic Creutzfeldt-Jakob disease (sCJD), analyze its sleep disorder characteristics using polysomnography (PSG), and compare sleep disturbances with those of fatal familial insomnia (FFI).
Patients and methods
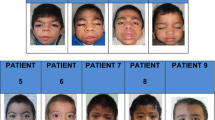
We retrospectively reviewed the sleep disturbances; cerebrospinal fluid (CSF) protein 14-3-3 (CSF-14-3-3 protein); prion protein gene, PRNP; magnetic resonance imaging; and electroencephalogram (EEG) of nine sCJD patients
Results
Of the nine sCJD patients, six were positive for CSF-14-3-3 protein. In the eight patients who completed diffusion-weighted imaging, seven showed cortical “ribbons sign” and two showed high signal in the basal ganglia. All nine patients had an EEG, which showed an increase in background slow waves; moreover, four showed typical periodic sharp wave complexes. The codon diversity at position 129, 219 of nine patients were MM, EE. Almost all nine patients had sleep disturbances such as insomnia, hypersomnia, and periodic limb movement disorder (PLMD). Five patients completed PSG, which demonstrated severe sleep structure disorder, prolonged total waking time, significantly reduced sleep efficiency, and absent rapid eye movement in some severe patients.
Conclusion
Sleep disturbances are common in sCJD patients, manifested as insomnia, lethargy, and PLMD. The sCJD patients often demonstrate severe sleep structure disorder through PSG, which is similar to patients with FFI.




Similar content being viewed by others
Abbreviations
- AD:
-
Alzheimer’s disease
- AHI:
-
apnea hypopnea index
- CJD:
-
Creutzfeldt-Jakob disease
- CSF:
-
cerebrospinal fluid
- CSF-14-3-3 protein:
-
protein 14-3-3
- DWI:
-
using diffusion-weighted imaging
- ECG:
-
electrocardiogram
- EEG:
-
electroencephalogram
- EMG:
-
electromyography
- FFI:
-
fatal familial insomnia
- FLAIR:
-
fluid-attenuated inversion recovery
- MRI:
-
magnetic resonance imaging
- NREM:
-
non-REM
- PD:
-
Parkinson’s disease
- PLMS:
-
periodic leg movement
- PSG:
-
polysomnography
- REM:
-
rapid eye movement
- RPD:
-
rapidly progressive dementias
- RT-QulC:
-
real-time quaking-induced conversion
- sCJD:
-
sporadic Creutzfeldt-Jakob disease
- SL:
-
sleep latency
- SPT:
-
time of sleep period
- T1WI:
-
T1-weighted imaging
- T2WI:
-
T2-weighted imaging
- TST:
-
total sleep time
- WASO:
-
waking time during sleep
References
Takada LT, Geschwind MD (2013) Prion diseases. Semin Neurol 33:348–356. https://doi.org/10.1055/s-0033-1359314
Geschwind MD (2015) Prion diseases. Continuum (Minneap Minn) 21:1612–1638. https://doi.org/10.1212/CON.0000000000000251
Coulthart MB et al (2015) Creutzfeldt-Jakob disease mortality in Canada, 1998 to 2013. Can Commun Dis Rep 41:182–191. https://doi.org/10.14745/ccdr.v41i08a01
Iwasaki Y, Mimuro M, Yoshida M, Sobue G, Hashizume Y (2009) Clinical diagnosis of Creutzfeldt-Jakob disease: accuracy based on analysis of autopsy-confirmed cases. J Neurol Sci 277:119–123. https://doi.org/10.1016/j.jns.2008.10.026
Zerr I et al (2009) Updated clinical diagnostic criteria for sporadic Creutzfeldt-Jakob disease. Brain 132:2659–2668. https://doi.org/10.1093/brain/awp191
Wu L et al (2017) Clinical features and sleep analysis of Chinese patients with fatal familial insomnia. Sci Rep 7:3625. https://doi.org/10.1038/s41598-017-03817-3
Morabito FC et al (2017) Deep learning representation from electroencephalography of early-stage Creutzfeldt-Jakob disease and features for differentiation from rapidly progressive dementia. Int J Neural Syst 27:1650039. https://doi.org/10.1142/S0129065716500398
Geschwind MD, Murray K (2018) Differential diagnosis with other rapid progressive dementias in human prion diseases. Handb Clin Neurol 153:371–397. https://doi.org/10.1016/B978-0-444-63945-5.00020-9
王晶, 周., 肖康, 王园, 董小平, 石琦. 2017年中国克-雅病监测网络病例特征分析. 疾病监测, 226-231. https://doi.org/10.3784/j.issn.1003-9961.2019.03.010 (2019).
Kobayashi A et al (2015) The influence of PRNP polymorphisms on human prion disease susceptibility: an update. Acta Neuropathol 130:159–170. https://doi.org/10.1007/s00401-015-1447-7
Xie D, Shen Q, Zhou J, Xu Y (2021) Non-motor symptoms are associated with REM sleep behavior disorder in Parkinson’s disease: a systematic review and meta-analysis. Neurol Sci 42:47–60. https://doi.org/10.1007/s10072-020-04769-9
Scaglione C et al (2005) REM sleep behaviour disorder in Parkinson’s disease: a questionnaire-based study. Neurol Sci 25:316–321. https://doi.org/10.1007/s10072-004-0364-7
Sharma DK, Boggild M, van Heuven AW, White RP (2017) Creutzfeldt-Jakob disease presenting as stroke: a case report and systematic literature review. Neurologist 22:48–53. https://doi.org/10.1097/NRL.0000000000000107
Matta G, Velakoulis D, Gaillard F, McLean CA, Yerra R (2017) Creutzfeldt-Jakob disease, cerebral amyloid angiopathy and Abeta-related angiitis with neuropsychiatric manifestations. Aust N Z J Psychiatry 51:740–741. https://doi.org/10.1177/0004867416686695
Wall CA, Rummans TA, Aksamit AJ, Krahn LE, Pankratz VS (2005) Psychiatric manifestations of Creutzfeldt-Jakob disease: a 25-year analysis. J Neuropsychiatr Clin Neurosci 17:489–495. https://doi.org/10.1176/jnp.17.4.489
Satishchandra P, Sharma P, Chatterji S, Shankar SK (1996) Psychiatric manifestations of Creutzfeldt Jakob disease: probable neuropathological correlates. Neurol India 44:43–46
Marciani MG et al (1996) Rapidly progressive form of Creutzfeldt-Jakob disease without dementia: a case report. Int J Neurosci 84:115–120. https://doi.org/10.3109/00207459608987256
Kretzschmar HA, Ironside JW, DeArmond SJ, Tateishi J (1996) Diagnostic criteria for sporadic Creutzfeldt-Jakob disease. Arch Neurol 53:913–920. https://doi.org/10.1001/archneur.1996.00550090125018
Bizzi A, Peoc’h K (2018) Amended diagnostic protocol increases the early diagnosis of sporadic Creutzfeldt-Jakob disease. Neurology 91:155–156. https://doi.org/10.1212/WNL.0000000000005871
Casimiro C et al (2012) Bilateral hyperintensity of the pulvinar and dorsomedial nucleus of the thalamus in sporadic Creutzfeldt-Jakob disease. Acta Medica Port 25(Suppl 1):41–44
Satoh K et al (2011) Early detection of sporadic CJD by diffusion-weighted MRI before the onset of symptoms. J Neurol Neurosurg Psychiatry 82:942–943. https://doi.org/10.1136/jnnp.2008.155242
Atarashi R et al (2011) Ultrasensitive human prion detection in cerebrospinal fluid by real-time quaking-induced conversion. Nat Med 17:175–178. https://doi.org/10.1038/nm.2294
Godal D, Simon S, Cheng K, Knox JD (2015) A new diagnostic test for Creutzfeldt-Jakob disease: real-time quaking-induced conversion (RT-QulC). Can Commun Dis Rep 41:192–195. https://doi.org/10.14745/ccdr.v41i08a02
Naismith SL et al (2010) Sleep well, think well: sleep-wake disturbance in mild cognitive impairment. J Geriatr Psychiatry Neurol 23:123–130. https://doi.org/10.1177/0891988710363710
Landolt HP et al (2006) Sleep-wake disturbances in sporadic Creutzfeldt-Jakob disease. Neurology 66:1418–1424. https://doi.org/10.1212/01.wnl.0000210445.16135.56
Terzano MG et al (1995) Precocious loss of physiological sleep in a case of Creutzfeldt Jakob disease: a serial polygraphic study. Sleep 18:849–858
Kang P et al (2016) Sleep pathology in Creutzfeldt-Jakob disease. J Clin Sleep Med 12:1033–1039. https://doi.org/10.5664/jcsm.5944
Brown RE, Basheer R, McKenna JT, Strecker RE, McCarley RW (2012) Control of sleep and wakefulness. Physiol Rev 92:1087–1187. https://doi.org/10.1152/physrev.00032.2011
Krasnianski A et al (2008) Fatal familial insomnia: clinical features and early identification. Ann Neurol 63:658–661. https://doi.org/10.1002/ana.21358
Montagna P, Gambetti P, Cortelli P, Lugaresi E (2003) Familial and sporadic fatal insomnia. Lancet Neurol 2:167–176. https://doi.org/10.1016/s1474-4422(03)00323-5
Parchi P, Strammiello R, Giese A, Kretzschmar H (2011) Phenotypic variability of sporadic human prion disease and its molecular basis: past, present, and future. Acta Neuropathol 121:91–112. https://doi.org/10.1007/s00401-010-0779-6
Katsube M, Shiota Y, Harada T, Shibata H, Nagai A (2013) A case of MM1+2 Creutzfeldt-Jakob disease with a longitudinal study of EEG and MRI. Rinsho Byori 61:995–1000
Abraham RR, Pallath V, Am C, Ramnarayan K, Kamath A (2012) Avenues for professional development: faculty perspectives from an Indian medical school. Kathmandu Univ Med J (KUMJ) 10:60–65. https://doi.org/10.3126/kumj.v10i4.10997
Parchi P et al (2000) Genetic influence on the structural variations of the abnormal prion protein. Proc Natl Acad Sci U S A 97:10168–10172. https://doi.org/10.1073/pnas.97.18.10168
Parchi P et al (1999) Classification of sporadic Creutzfeldt-Jakob disease based on molecular and phenotypic analysis of 300 subjects. Ann Neurol 46:224–233
Parchi P et al (2009) Incidence and spectrum of sporadic Creutzfeldt-Jakob disease variants with mixed phenotype and co-occurrence of PrPSc types: an updated classification. Acta Neuropathol 118:659–671. https://doi.org/10.1007/s00401-009-0585-1
Parchi P et al (2012) Consensus classification of human prion disease histotypes allows reliable identification of molecular subtypes: an inter-rater study among surveillance centres in Europe and USA. Acta Neuropathol 124:517–529. https://doi.org/10.1007/s00401-012-1002-8
Kobayashi A et al (2008) Plaque-type deposition of prion protein in the damaged white matter of sporadic Creutzfeldt-Jakob disease MM1 patients. Acta Neuropathol 116:561–566. https://doi.org/10.1007/s00401-008-0425-8
Rossi M et al (2017) Atypical Creutzfeldt-Jakob disease with PrP-amyloid plaques in white matter: molecular characterization and transmission to bank voles show the M1 strain signature. Acta Neuropathol Commun 5:87. https://doi.org/10.1186/s40478-017-0496-7
Gelpi E et al (2013) Atypical neuropathological sCJD-MM phenotype with abundant white matter Kuru-type plaques sparing the cerebellar cortex. Neuropathology 33:204–208. https://doi.org/10.1111/j.1440-1789.2012.01341.x
Meissner B et al (2005) Sporadic Creutzfeldt-Jakob disease: clinical and diagnostic characteristics of the rare VV1 type. Neurology 65:1544–1550. https://doi.org/10.1212/01.wnl.0000184674.32924.c9
Krasnianski A et al (2006) Clinical features and diagnosis of the MM2 cortical subtype of sporadic Creutzfeldt-Jakob disease. Arch Neurol 63:876–880. https://doi.org/10.1001/archneur.63.6.876
Zerr I, Parchi P (2018) Sporadic Creutzfeldt-Jakob disease. Handb Clin Neurol 153:155–174. https://doi.org/10.1016/B978-0-444-63945-5.00009-X
Gambetti P, Kong Q, Zou W, Parchi P, Chen SG (2003) Sporadic and familial CJD: classification and characterisation. Br Med Bull 66:213–239. https://doi.org/10.1093/bmb/66.1.213
Barash JA (2009) Clinical features of sporadic fatal insomnia. Rev Neurol Dis 6:E87–E93
Acknowledgements
We thank the participants and all the study staff.
Ethical approval
The present study was approved by ethics committees at Changchun in Chian.
Informed consent
The present study has obtained informed consent from all patients and authors.
Competing interests
The authors declare no competing interests.
Author information
Authors and Affiliations
Contributions
Yanyuan Dai and Jie Shao: conception, study design, execution, acquisition of data, analysis and interpretation, and writing
Yue Lang: acquisition of data, analysis, and interpretation;
Yudan Lv: analysis and interpretation;
Li Cui: conception, study design, analysis and interpretation, and critical review of the article.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dai, Y., Shao, J., Lang, Y. et al. Clinical manifestations and polysomnography-based analysis in nine cases of probable sporadic Creutzfeldt-Jakob disease. Neurol Sci 42, 4209–4219 (2021). https://doi.org/10.1007/s10072-021-05102-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05102-8