Abstract
Background and objectives
Migraine is an episodic disorder that is characterized by unilateral headache lasting 4–72 h along with certain associated features. Modifying dietary habits have been considered an appropriate therapeutic approach in these patients. This study was designed to examine the association between dietary diversity score (DDS) and severity, frequency, and duration of migraine attacks.
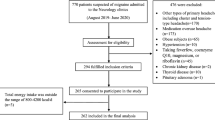
Methods and materials
The present study was conducted using a cross-sectional design on 256 women 18–50 years old referred to neurology clinics for the first time. After the diagnosis of migraine by a neurologist, the data related to anthropometric measures and dietary intake (147-item semi-quantitative food frequency questionnaire) were collected. To assess migraine severity, the migraine disability assessment questionnaire (MIDAS), visual analog scale (VAS), and a 30-day headache diary were used. Multinomial logistic regression was used to evaluate the association between DDS and migraine severity. The age, physical activity, BMI, and job were considered confounding variables in regression model. Data were analyzed using SPSS software and P values < 0.05 considered statistically significant.
Results
Totally, 256 subjects participated in the present study with mean age, height, weight, and BMI of 34.28 ± 7.88 years, 161.78 ± 5.18 cm, 69.25 ± 13.06 kg, and 26.46 ± 4.89 kg/m2, respectively. Subjects with higher DDS had a lower waist circumference (P = 0.01). There was no association between DDS and other anthropometric measures and demographic characteristics (P > 0.05). In the crude model of logistic regression, participants with lower DDS had higher odds of more pain severity (OR = 2.30; 95% CI = 1.28, 4.12; P = 0.005), migraine disability (OR = 2.66; 95% CI = 1.51, 4.69; P = 0.001), and headache duration (OR = 2.32; CI = 1.22, 4.40; P = 0.01) compared to reference group. No association was found between headache frequency and DDS. Adjusting for the effect of confounding variables did not change the significant association.
Conclusion
DDS was inversely associated with migraine disability, pain severity, and headache frequency. Additional studies are needed to replicate these findings and to explore mechanisms that mediate the association between DDS and migraine attacks.
Similar content being viewed by others
References
Goadsby PJ, Holland PR (2019) Pathophysiology of migraine: an update. Neurol Clin 37(4):651–671
Steiner TJ, Huynh N, Stovner LJ (2019) Headache disorders and the World Health Organization. In: Societal impact of headache, vol 56(10). Springer, pp 37–43
Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I et al (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386(9995):743–800
Whiteford HA, Ferrari AJ, Degenhardt L, Feigin V, Vos T (2015) The global burden of mental, neurological and substance use disorders: an analysis from the global burden of disease study 2010. PLoS One 10(2):e0116820
Sprenger T, Goadsby PJ (2009) Migraine pathogenesis and state of pharmacological treatment options. BMC Med 7(1):71
Marmura MJ, Silberstein SD, Schwedt TJ (2015) The acute treatment of migraine in adults: the a merican H eadache S ociety evidence assessment of migraine pharmacotherapies. Headache 55(1):3–20
Silberstein S, Holland S, Freitag F, Dodick DW, Argoff C, Ashman E (2012) Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the quality standards Subcommittee of the American Academy of neurology and the American headache Society. Neurology. 78(17):1337–1345
Society AH (2019) The American headache society position statement on integrating new migraine treatments into clinical practice. Headache 59(1):1–18
Diener H-C, Charles A, Goadsby PJ, Holle D (2015) New therapeutic approaches for the prevention and treatment of migraine. Lancet Neurol 14(10):1010–1022
Börü ÜT, Koçer A, Lüleci A, Sur H, Tutkan H, Atli H (2005) Prevalence and characteristics of migraine in women of reproductive age in Istanbul, Turkey: a population based survey. Tohoku J Exp Med 206(1):51–59
Negro A, D’Alonzo L, Martelletti P (2010) Chronic migraine: comorbidities, risk factors, and rehabilitation. Intern Emerg Med 5(1):13–19
Nuaman BN, Sadik AM (2019) Migraine is strongly associated with central obesity than with general obesity: a case-control study. Turk J Endocrinol Metab 23(1):25–32
Sun-Edelstein C, Mauskop A (2009) Foods and supplements in the management of migraine headaches. Clin J Pain 25(5):446–452
Gazerani P (2020) Migraine and diet. Nutrients. 12(6):1658
Jahromi SR, Ghorbani Z, Martelletti P, Lampl C, Togha M (2019) Association of diet and headache. J Headache Pain 20(1):1–11
Thompson D, Saluja H (2017) Prophylaxis of migraine headaches with riboflavin: a systematic review. J Clin Pharm Ther 42(4):394–403
Chiu H-Y, Yeh TH, Huang YC, Chen PY (2016) Effects of intravenous and oral magnesium on reducing migraine: a meta-analysis of randomized controlled trials. Pain Phys 19(1):E97–E112
Martin VT, Vij B (2016) Diet and headache: part 1. Headache 56(9):1543–1552
Evans EW, Lipton RB, Peterlin BL, Raynor HA, Thomas JG, O'Leary KC, Pavlovic J, Wing RR, Bond DS (2015) Dietary intake patterns and diet quality in a nationally representative sample of women with and without severe headache or migraine. Headache 55(4):550–561
Herforth A, Martínez-Steele E, Calixto G, Sattamini I, Olarte D, Ballard T et al (2019) Development of a diet quality questionnaire for improved measurement of dietary diversity and other diet quality indicators (P13-018-19). Curr Dev Nutr 3(Supplement_1):1236
Crawford P, Simmons M (2006) What dietary modifications are indicated for migraines? Clinical Inquiries 55(1):1–3
Hu FB (2002) Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 13(1):3–9
Finkel AG, Yerry JA, Mann JD (2013) Dietary considerations in migraine management: does a consistent diet improve migraine? Curr Pain Headache Rep 17(11):373
Kant AK, Graubard BI (2005) A comparison of three dietary pattern indexes for predicting biomarkers of diet and disease. J Am Coll Nutr 24(4):294–303
Azadbakht L, Mirmiran P, Azizi F (2005) Dietary diversity score is favorably associated with the metabolic syndrome in Tehranian adults. Int J Obes 29(11):1361–1367
Kant AK, Schatzkin A, Ziegler RG (1995) Dietary diversity and subsequent cause-specific mortality in the NHANES I epidemiologic follow-up study. J Am Coll Nutr 14(3):233–238
Committee IR (2005) Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ)-short and long forms. http://www.ipaqkise/scoring.pdf.
Levin M (2013) The international classification of headache disorders, (ICHD III)–changes and challenges. Headache 53(8):1383–1395
Stewart WF, Lipton RB, Dowson AJ, Sawyer J (2001) Development and testing of the migraine disability assessment (MIDAS) questionnaire to assess headache-related disability. Neurology. 56(suppl 1):S20–SS8
Ghorbani A, Chitsaz A (2011) Comparison of validity and reliability of the migraine disability assessment (MIDAS) versus headache impact test (HIT) in an Iranian population. Iran J Neurol 10(3–4):39–42
Price DD, McGrath PA, Rafii A, Buckingham B (1983) The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 17(1):45–56
Joy EJ, Green R, Agrawal S, Aleksandrowicz L, Bowen L, Kinra S et al (2017) Dietary patterns and non-communicable disease risk in Indian adults: secondary analysis of Indian migration study data. Public Health Nutr 20(11):1963–1972
Azadbakht L, Akbari F, Esmaillzadeh A (2015) Diet quality among Iranian adolescents needs improvement. Public Health Nutr 18(4):615–621
Arimond M, Wiesmann D, Becquey E, Carriquiry A, Daniels MC, Deitchler M, Fanou-Fogny N, Joseph ML, Kennedy G, Martin-Prevel Y, Torheim LE (2010) Simple food group diversity indicators predict micronutrient adequacy of women's diets in 5 diverse, resource-poor settings. J Nutr 140(11):2059S–2069S
Evans EW, Lipton RB, Peterlin BL, Raynor HA, Thomas JG, O'Leary KC, Pavlovic J, Wing RR, Bond DS (2015) Dietary intake patterns and diet quality in a nationally representative sample of women with and without severe headache or migraine. Headache. 55(4):550–561
Carrera-Bastos P, Fontes-Villalba M, O'Keefe JH, Lindeberg S, Cordain L (2011) The western diet and lifestyle and diseases of civilization. Res Rep Clin Cardiol 2:15–35
Hajjarzadeh S, Mahdavi R, Shalilahmadi D, Nikniaz Z (2020) The association of dietary patterns with migraine attack frequency in migrainous women. Nutr Neurosci 23(9):724–730
Hajjarzadeh S, Nikniaz Z, Shalilahmadi D, Mahdavi R, Behrouz M (2019) Comparison of diet quality between women with chronic and episodic migraine. Headache 59(8):1221–1228
Ruel MT (2003) Operationalizing dietary diversity: a review of measurement issues and research priorities. J Nutr 133(11):3911S–3926S
Amer M, Woodward M, Appel LJ (2014) Effects of dietary sodium and the DASH diet on the occurrence of headaches: results from randomised multicentre DASH-sodium clinical trial. BMJ Open 4(12):e006671
Zaeem Z, Zhou L, Dilli E (2016) Headaches: a review of the role of dietary factors. Curr Neurol Neurosci Rep 16(11):101
Paliwal VK, Uniyal R, Anand S (2018) Hypertension and its relation to headache and other craniofacial neuralgiform pain. Hypertension. 4(1):27
Cooper W, Glover D, Hormbrey J, Kimber G (1989) Headache and blood pressure: evidence of a close relationship. J Hum Hypertens 3(1):41–44
Zhao W, Yu K, Tan S, Zheng Y, Zhao A, Wang P, Zhang Y (2017) Dietary diversity scores: an indicator of micronutrient inadequacy instead of obesity for Chinese children. BMC Public Health 17(1):440
Mirmiran P, Azadbakht L, Azizi F (2006) Dietary diversity within food groups: an indicator of specific nutrient adequacy in Tehranian women. J Am Coll Nutr 25(4):354–361
Acham H, Oldewage-Theron WH, Egal AA (2012) Dietary diversity, micronutrient intake and their variation among black women in informal settlements in South Africa: a cross-sectional study. Int J Nutri Metabol 4(2):24–39
Firger R, Haase G (2018) Compositions of ketogenic sources, micronutrients and phytochemicals for prophylaxis and mitigation of migraine headache. Google Patents, US 10,500,182 B2
Gaul C, Diener H-C, Danesch U, Group MS (2015) Improvement of migraine symptoms with a proprietary supplement containing riboflavin, magnesium and Q10: a randomized, placebo-controlled, double-blind, multicenter trial. J Headache Pain 16(1):32
Nattagh-Eshtivani E, Sani MA, Dahri M, Ghalichi F, Ghavami A, Arjang P, Tarighat-Esfanjani A (2018) The role of nutrients in the pathogenesis and treatment of migraine headaches. Biomed Pharmacother 102:317–325
Mak T-N, Angeles-Agdeppa I, Lenighan YM, Capanzana MV, Montoliu I (2019) Diet diversity and micronutrient adequacy among Filipino school-age children. Nutrients. 11(9):2197
Hjertholm KG, Holmboe-Ottesen G, Iversen PO, Mdala I, Munthali A, Maleta K et al (2019) Seasonality in associations between dietary diversity scores and nutrient adequacy ratios among pregnant women in rural Malawi–a cross-sectional study. Food Nutr Res 63(2712):1–8
Jayawardena R, Byrne NM, Soares MJ, Katulanda P, Yadav B, Hills AP (2013) High dietary diversity is associated with obesity in Sri Lankan adults: an evaluation of three dietary scores. BMC Public Health 13(1):314
Andreeva VA, Fezeu LK, Hercberg S, Galan P (2018) Obesity and migraine: effect modification by gender and perceived stress. Neuroepidemiology. 51(1–2):25–32
Acknowledgments
The authors thank the study participants for their cooperation and assistance in physical examinations. They also thank those involved in nutritional evaluation and database management, as well as the neurology clinics of Sina and Khatam Alanbia hospitals. We sincerely express our appreciation to the participants of this study.
Funding
This study was supported by the Tehran University of Medical Sciences and by grants from Tehran University of Medical Sciences (Grants ID:95-01-103-31348).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Informed consent
None.
Ethical approval
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khorsha, F., Mirzababaei, A., Togha, M. et al. Association of dietary diversity score (DDS) and migraine headache severity among women. Neurol Sci 42, 3403–3410 (2021). https://doi.org/10.1007/s10072-020-04982-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04982-6