Abstract
Objective
Cervicocephalic artery dissection (CeAD) is the most common cause of ischemic stroke in young adults. Although the exact cause is unknown, inflammation is thought to have a role. Here, we investigated the relationship between CeAD and inflammation.
Methods
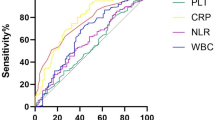
Patients diagnosed with CeAD in our stroke center were evaluated retrospectively, and their demographic and clinical features were recorded. The C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), white blood cell, neutrophil and lymphocyte counts, platelet/lymphocyte ratio (PLR), and neutrophil/lymphocyte ratio (NLR) were recorded on admission. Modified Rankin scores (mRS) were noted on admission and at 6 months to evaluate the dependency status and functional outcome of each patient.
Results
Of the 95 patients in the study, 70 (73.7%) were male, and the mean age was 44.4 ± 9.8 years. Patients with high WBC count, ESR, PLR, and NLR frequently had mRS scores of 3–6 at admission; these differences were significant (p = 0.04, p = 0.02, p = 0.04, and p = 0.02, respectively). At 6 months, patients with high CRP and ESR at admission also had significantly poorer prognoses (p < 0.001, p = 0.002, respectively). PLR and NLR values were higher in patients with mRS of 3–6. But there were no significant differences between the good and poor prognosis groups regarding PLR and NLR (p = 0.22, p = 0.05, respectively).
Conclusion
Inflammation may have a role in the prognosis of CeAD, and inflammatory markers can be evaluated as auxiliary tests for determining prognosis.
Similar content being viewed by others
References
Debette S, Leys D (2009) Cervical-artery dissections: predisposing factors, diagnosis, and outcome. Lancet Neurol 8(7):668–678
Lee VH, Brown RD Jr, Mandrekar JN, Mokri B (2006) Incidence and outcome of cervical artery dissection: a population-based study. Neurology 67(10):1809–1812
Engelter ST, Grond-Ginsbach C, Metso TM et al (2013) Cervical Artery Dissection and Ischemic Stroke Patients Study Group. Cervical artery dissection: trauma and other potential mechanical trigger events. Neurology 80(21):1950–1957
Caso V, Paciaroni M, Bogousslavsky J (2005) Environmental factors and cervical artery dissection. Front Neurol Neurosci 20:44–53
Naggara O, Touzé E, Marsico R et al (2009) High-resolution MR imaging of periarterial edema associated with biological inflammation in spontaneous carotid dissection. Eur Radiol 19(9):2255–2260
Pfefferkorn T, Saam T, Rominger A, Habs M, Gerdes LA, Schmidt C, Cyran C, Straube A, Linn J, Nikolaou K, Bartenstein P, Reiser M, Hacker M, Dichgans M (2011) Vessel wall inflammation in spontaneous cervical bartery dissection: a prospective, observational positron emission tomography, computed tomography, and magnetic resonance imaging study. Stroke. 42(6):1563–1568
Debette S (2014) Pathophysiology and risk factors of cervical artery dissection: what have we learnt from large hospital-based cohorts? Curr Opin Neurol 27(1):20–28
Metso AJ, Metso TM, Debette S, Dallongeville J, Lyrer PA, Pezzini A, Lichy C, Kloss M, Brandt T, Touzé E, Southerland AM, Worrall BB, Abboud S, del Zotto E, Leys D, Engelter S, Grond-Ginsbach C, Tatlisumak T, for the CADISP group (2012) Gender and cervical artery dissection. Eur J Neurol 19(4):594–602
Arnold M, Bousser MG, Fahrni G, Fischer U, Georgiadis D, Gandjour J, Benninger D, Sturzenegger M, Mattle HP, Baumgartner RW (2006) Vertebral artery dissection: presenting findings and predictors of outcome. Stroke 37:2499–2503
Völker W, Besselmann M, Dittrich R et al (2005) Generalized arteriopathy in patients with cervical artery dissection. Neurology 64(9):1508–1513
Forster K, Poppert H, Conrad B, Sander D (2006) Elevated inflammatory laboratory parameters in spontaneous cervical artery dissection as compared to traumatic dissection: a retrospective case-control study. J Neurol 253(6):741–745
Whiteley W, Jackson C, Lewis S, Lowe G, Rumley A, Sandercock P, Wardlaw J, Dennis M, Sudlow C (2009) Inflammatory markers and poor outcome after stroke: a prospective cohort study and systematic review of interleukin-6. PLoS Med 6(9):e1000145
Xue J, Huang W, Chen X, Li Q, Cai Z, Yu T, Shao B (2017) Neutrophil-to-lymphocyte ratio is a prognostic marker in acute ischemic stroke. J Stroke Cerebrovasc Dis 26(3):650–657
Kim JY, Kawabori M, Yenari MA (2014) Innate inflammatory responses in stroke: mechanisms and potential therapeutic targets. Curr Med Chem 21:2076–2097
Franks ZG, Campbell RA, Weyrich AS, Rondina MT (2010) Platelet-leukocyte interactions link inflammatory and thromboembolic events in ischemic stroke. Ann N Y Acad Sci 1207:11–17
Xu JH, He XW, Li Q et al (2019) Higher platelet-to-lymphocyte ratio is associated with worse outcomes after intravenous thrombolysis in acute ischaemic stroke. Front Neurol 10:1192
İdil Soylu A, Arıkan Cortcu S, Uzunkaya F, Atalay YO, Bekçi T, Güngör L, Belet Ü (2017) The correlation of the platelet-to-lymphocyte ratio with the severity of stenosis and stroke in patients with carotid arterial disease. Vascular 25(3):299–306
Li S, Zi W, Chen J, Zhang S, Bai Y, Guo Y, Shang X, Sun B, Liang M, Liu Y, Wan Y, Wang M, Zhao M, Liu R, Zhu W, Liu X, Xu G (2018) Feasibility of thrombectomy in treating acute ischemic stroke because of cervical artery dissection. Stroke 49(12):3075–3077
CADISS trial investigators, Markus HS, Hayter E et al (2015) Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS): a randomised trial. Lancet Neurol 14(4):361–367
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical approval
This study has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Senadim, S., Çoban, E., Tekin, B. et al. The inflammatory markers and prognosis of cervicocephalic artery dissection: a stroke center study from a tertiary hospital. Neurol Sci 41, 3741–3745 (2020). https://doi.org/10.1007/s10072-020-04699-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04699-6