Abstract
Background and purpose
The predictors of progressive motor deficits in acute subcortical infarctions are still controversial. It is not known whether glycemic control influences on stroke progression.
Methods
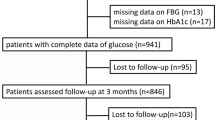
A total of 268 consecutive patients with diabetes or prediabetes who had acute (< 24 h) subcortical infarction were enrolled. (1) All patients were divided into 4 groups by quartile of glycated hemoglobin (HbA1c). (2) Only the patients with diabetes were divided by effective glycemic control. Progressive motor deficits were prospectively captured and defined as an increase of motor score ≥ 1 on the upper or lower limb items of the National Institute of Health Stroke Scale within 72 h from stroke onset.
Results
Progressive motor deficits occur in 8/78 (10.3%) for ≤ 5.9, 15/61 (24.6%) for 6.0–6.4, 16/62 (25.8%) for 6.5–7.4, and 30/67 (44.8%) for ≥ 7.5. In diabetic patients alone, those occur in 5/37 (13.5%) for ≤ 6.5, 10/42 (23.8%) for 6.6–7.0, 12/42 (28.6%) for 7.1–8.0, and 24/50 (48.0%) for ≥ 8.1. An adjusted OR of progressive motor deficits was 2.61 (95% confidence interval [CI] 0.98–7.00, P = .056) for 6.0–6.4, 3.42 (95% CI 1.27–9.18, P = .015) for 6.5–7.4, and 6.65 (95% CI 2.38–18.62, P < .001) for ≥ 7.5. In diabetic patients alone, those were 3.15 (95% CI 0.89–11.15, P = .075) for 6.6–7.0, 2.90 (95% CI 0.79–10.61, P = .107) for 7.1–8.0, and 4.17 (95% CI 1.07–16.25, P = .038) for ≥ 8.1. The optimal cutoff value of HbA1c was 6.65% in discriminating progressive motor deficits.
Conclusion
Increased HbA1c was associated with higher incidence of progressive motor deficits in acute subcortical infarction with diabetes and prediabetes.


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bamford J, Sandercock P, Dennis M, Burn J, Warlow C (1991) Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet 337(8756):1521–1526
Sacco S, Marini C, Totaro R, Russo T, Cerone D, Carolei A (2006) A population-based study of the incidence and prognosis of lacunar stroke. Neurology 66(9):1335–1338
Jorgensen HS, Nakayama H, Raaschou HO, Olsen TS (1994) Effect of blood pressure and diabetes on stroke in progression. Lancet 344(8916):156–159
Nakamura K, Saku Y, Ibayashi S, Fujishima M (1999) Progressive motor deficits in lacunar infarction. Neurology 52(1):29–33
Vahidy FS, Hicks WJ 2nd, Acosta I, Hallevi H, Peng H, Pandurengan R, Gonzales NR, Barreto AD, Martin-Schild S, Wu TC et al (2014) Neurofluctuation in patients with subcortical ischemic stroke. Neurology 83(5):398–405
Steinke W, Ley SC (2002) Lacunar stroke is the major cause of progressive motor deficits. Stroke 33(6):1510–1516
Sumer M, Ozdemir I, Erturk O (2003) Progression in acute ischemic stroke: frequency, risk factors and prognosis. J Clin Neurosci 10(2):177–180
Davalos A, Cendra E, Teruel J, Martinez M, Genis D (1990) Deteriorating ischemic stroke: risk factors and prognosis. Neurology 40(12):1865–1869
Bogousslavsky J, Barnett HJ, Fox AJ, Hachinski VC, Taylor W (1986) Atherosclerotic disease of the middle cerebral artery. Stroke 17(6):1112–1120
Yamamoto Y, Ohara T, Hamanaka M, Hosomi A, Tamura A, Akiguchi I (2011) Characteristics of intracranial branch atheromatous disease and its association with progressive motor deficits. J Neurol Sci 304(1–2):78–82
Caplan LR (1996) Diabetes and brain ischemia. Diabetes 45(Suppl 3):S95–S97
Nakase T, Yoshioka S, Sasaki M, Suzuki A (2013) Clinical evaluation of lacunar infarction and branch atheromatous disease. J Stroke Cerebrovasc Dis 22(4):406–412
Yamanouchi H, Shimada H, Tomonaga M, Matsushita S (1989) Recurrence of embolic stroke in non-valvular atrial fibrillation (NVAF). An autopsy study. Acta Neurol Scand 80(2):123–129
Sacco RL, Foulkes MA, Mohr JP, Wolf PA, Hier DB, Price TR (1989) Determinants of early recurrence of cerebral infarction. The Stroke Data Bank. Stroke 20(8):983–989
Kim BJ, Park JM, Kang K, Lee SJ, Ko Y, Kim JG, Cha JK, Kim DH, Nah HW, Han MK, Park TH, Park SS, Lee KB, Lee J, Hong KS, Cho YJ, Lee BC, Yu KH, Oh MS, Kim DE, Ryu WS, Cho KH, Kim JT, Choi JC, Kim WJ, Shin DI, Yeo MJ, Sohn SI, Hong JH, Lee J, Lee JS, Yoon BW, Bae HJ (2015) Case characteristics, hyperacute treatment, and outcome information from the clinical research center for stroke-fifth division registry in South Korea. J Stroke 17(1):38–53
Kim SK, Song P, Hong JM, Pak CY, Chung CS, Lee KH, Kim GM (2008) Prediction of progressive motor deficits in patients with deep subcortical infarction. Cerebrovasc Dis 25(4):297–303
Nannoni S, Del Bene A, Palumbo V, Petrone L, Sottile F, Pracucci G, Inzitari D (2015) Predictors of progression in patients presenting with minor subcortical stroke. Acta Neurol Scand 132(5):304–309
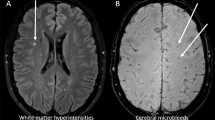
Kapeller P, Barber R, Vermeulen RJ, Ader H, Scheltens P, Freidl W, Almkvist O, Moretti M, del Ser T, Vaghfeldt P et al (2003) Visual rating of age-related white matter changes on magnetic resonance imaging: scale comparison, interrater agreement, and correlations with quantitative measurements. Stroke 34(2):441–445
Chimowitz MI, Lynn MJ, Howlett-Smith H, Stern BJ, Hertzberg VS, Frankel MR, Levine SR, Chaturvedi S, Kasner SE, Benesch CG, Sila CA, Jovin TG, Romano JG (2005) Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med 352(13):1305–1316
American Diabetes Association. (2015). 2. Classification and diagnosis of diabetes. Diabetes care, 38(Supplement 1), S8-S16.
American Diabetes Association. (2016). 5. Glycemic targets. Diabetes Care, 39(Supplement 1), S39-S46.
Federation ID: IDF global guideline for managing older people with type 2 diabetes. 2013
Kamouchi M, Matsuki T, Hata J, Kuwashiro T, Ago T, Sambongi Y, Fukushima Y, Sugimori H, Kitazono T (2011) Prestroke glycemic control is associated with the functional outcome in acute ischemic stroke: the Fukuoka stroke registry. Stroke 42(10):2788–2794
Del Bene A, Palumbo V, Lamassa M, Saia V, Piccardi B, Inzitari D (2012) Progressive lacunar stroke: review of mechanisms, prognostic features, and putative treatments. Int J Stroke 7(4):321–329
Nagakane Y, Naritomi H, Oe H, Nagatsuka K, Yamawaki T (2008) Neurological and MRI findings as predictors of progressive-type lacunar infarction. Eur Neurol 60(3):137–141
Kramer D, Raji A, Plutzky J (2003) Prediabetes mellitus and its links to atherosclerosis. Curr Diab Rep 3(1):11–18
Park JH, Kwon HM, Roh JK (2007) Metabolic syndrome is more associated with intracranial atherosclerosis than extracranial atherosclerosis. Eur J Neurol 14(4):379–386
Park HY, Kyeong H, Park DS, Lee HS, Chang H, Kim YS, Cho KH (2008) Correlation between insulin resistance and intracranial atherosclerosis in patients with ischemic stroke without diabetes. J Stroke Cerebrovasc Dis 17(6):401–405
Tanaka R, Ueno Y, Miyamoto N, Yamashiro K, Tanaka Y, Shimura H, Hattori N, Urabe T (2013) Impact of diabetes and prediabetes on the short-term prognosis in patients with acute ischemic stroke. J Neurol Sci 332(1–2):45–50
Ago T, Matsuo R, Hata J, Wakisaka Y, Kuroda J, Kitazono T, Kamouchi M (2018) Insulin resistance and clinical outcomes after acute ischemic stroke. Neurology 90(17):e1470–e1477
Katakami N (2018) Mechanism of development of atherosclerosis and cardiovascular disease in diabetes mellitus. J Atheroscler Thromb 25(1):27–39
Choi N, Lee JY, Sunwoo JS, Roh H, Ahn MY, Park ST, Lee KB (2017) Recently uncontrolled glycemia in diabetic patients is associated with the severity of intracranial atherosclerosis. J Stroke Cerebrovasc Dis 26(11):2615–2621
Wu S, Shi Y, Wang C, Jia Q, Zhang N, Zhao X, Liu G, Wang Y, Liu L, Wang Y, On Behalf of the Investigators for the Survey on Abnormal Glucose Regulation in Patients With Acute Stroke Across China (ACROSS-China) (2013) Glycated hemoglobin independently predicts stroke recurrence within one year after acute first-ever non-cardioembolic strokes onset in a Chinese cohort study. PLoS One 8(11):e80690
Baird TA, Parsons MW, Phan T, Butcher KS, Desmond PM, Tress BM, Colman PG, Chambers BR, Davis SM (2003) Persistent poststroke hyperglycemia is independently associated with infarct expansion and worse clinical outcome. Stroke 34(9):2208–2214
MacDougall NJ, Muir KW (2011) Hyperglycaemia and infarct size in animal models of middle cerebral artery occlusion: systematic review and meta-analysis. J Cereb Blood Flow Metab 31(3):807–818
Bang OY, Joo SY, Lee PH, Joo US, Lee JH, Joo IS, Huh K (2004) The course of patients with lacunar infarcts and a parent arterial lesion: similarities to large artery vs small artery disease. Arch Neurol 61(4):514–519
Kwon, H. M., Lim, J. S., Park, H. K., & Lee, Y. S. (2011). Hypertriglyceridemia as a possible predictor of early neurological deterioration in acute lacunar stroke. Journal of the neurological sciences, 309(1-2), 128-130.
Code availability
Not applicable
Funding
This study was supported by the (1) Yuhan Corporation and (2) Soonchunhyang University Research Fund.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design: Material preparation by Kayeong Im and Kyung Bok Lee; data collection by Hyunjin Ju, Mina Lee, Byung-Euk Joo, Kyum-Yil Kwon, Hakjae Roh, and Moo-Young Ahn; analysis by Hye-Won Hwang. The first draft of the manuscript was written by Kayeong Im, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study design was approved by the local institutional review board before study initiation (No. 2019-11-028-001).
Consent to participate
All patients agreed on the informed consent form for the stroke registry at admission.
Consent for publication
Not applicable
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Im, K., Ju, H., Lee, M. et al. Recent glycemic control can predict the progressive motor deficits of acute subcortical infarction with diabetes or prediabetes. Neurol Sci 42, 285–291 (2021). https://doi.org/10.1007/s10072-020-04634-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04634-9