Abstract
Objective
To compare the interhemispheric asymmetry of the motor cortex excitability of chronic stroke patients with healthy and to observe if the magnitude of this asymmetry is associated to sensory-motor impairment and stroke chronicity.
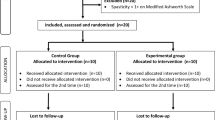
Methods
This cross-sectional study was performed with chronic stroke and aged and sex-matched healthy individuals. The interhemispheric asymmetry index was calculated by the difference of rest motor threshold (rMT) of the brain hemispheres. The rMT was assessed by transcranial magnetic stimulation over the cortical representation of the first dorsal interosseous muscle. To investigate the relationship of the asymmetry with sensory-motor impairment and injury chronicity, the stroke patients were grouped according to the level of sensory-motor impairment (mild/moderate, moderate/severe, and severe) and different chronicity stages (> 3–12, 13–24, 25–60, and > 60 months since stroke).
Results
Fifty-six chronic stroke and twenty-six healthy were included. We found higher interhemispheric asymmetry in stroke patients (mean, 27.1 ± 20.9) compared to healthy (mean, 4.9 ± 4.7). The asymmetry was higher in patients with moderate/severe (mean, 35.4 ± 20.4) and severe (mean, 32.9 ± 22.7) impairment. No difference was found between patients with mild/moderate impairment (mean, 15.5 ± 12.5) and healthy. There were no differences of the interhemispheric asymmetry between patients with different times since stroke (> 3–12, mean, 32 ± 18.1; > 13–24, mean, 20.7 ± 16.2; > 25–60, mean, 29.6 ± 18.1; > 60 months, mean, 25.9 ± 17.5).
Conclusion
Stroke patients showed higher interhemispheric asymmetry of the motor cortex excitability when compared to healthy, and the magnitude of this asymmetry seems to be correlated with the severity of sensory-motor impairment, but not with stroke chronicity.
Significance
Higher interhemispheric asymmetry was found in stroke patients with greatest sensory-motor impairment.





Similar content being viewed by others
References
Ackerley SJ, Stinear CM, Barber PA, Byblow WD (2010) Combining theta burst stimulation with training after subcortical stroke. Stroke 41:1568–1572
Allman C, Amadi U, Winkler AM et al (2016) Ipsilesional anodal tDCS enhances the functional benefits of rehabilitation in patients after stroke. Sci Transl Med 8:330re331
Bertolucci F, Chisari C, Fregni F (2018) The potential dual role of transcallosal inhibition in post-stroke motor recovery. Restor Neurol Neurosci 36:83–97. https://doi.org/10.3233/RNN-170778
Boddington L, Reynolds J (2017) Targeting interhemispheric inhibition with neuromodulation to enhance stroke rehabilitation. Brain Stimul 10:214–222
Bradnam LV, Stinear CM, Barber PA, Byblow WD (2012) Contralesional hemisphere control of the proximal paretic upper limb following stroke. Cereb Cortex 22:2662–2671. https://doi.org/10.1093/cercor/bhr344
Bradnam LV, Stinear CM, Byblow WD (2011) Cathodal transcranial direct current stimulation suppresses ipsilateral projections to presumed propriospinal neurons of the proximal upper limb. J Neurophysiol 105:2582–2589. https://doi.org/10.1152/jn.01084.2010
Bradnam LV, Stinear CM, Byblow WD (2013) Ipsilateral motor pathways after stroke: implications for non-invasive brain stimulation. Front Hum Neurosci 7:184
Chagas AP, Monteiro M, Mazer V, Baltar A, Marques D, Carneiro M, Rodrigues de Araújo MDG, Piscitelli D, Monte-Silva K (2018) Cortical excitability variability: insights into biological and behavioral characteristics of healthy individuals. J Neurol Sci 390:172–177. https://doi.org/10.1016/j.jns.2018.04.036
Di Pino G, Pellegrino G, Assenza G et al (2014) Modulation of brain plasticity in stroke: a novel model for neurorehabilitation. Nat Rev Neurol 10:597–608. https://doi.org/10.1038/nrneurol.2014.162
Dodd KC, Nair VA, Prabhakaran V (2017) Role of the contralesional vs. ipsilesional hemisphere in stroke recovery. Front Hum Neurosci 11:469
Feigin VL, Roth GA, Naghavi M et al (2016) Global burden of stroke and risk factors in 188 countries, during 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet Neurol 15:913–924
Feng W, Wang J, Chhatbar PY et al (2015) Corticospinal tract lesion load: an imaging biomarker for stroke motor outcomes. Ann Neurol 78:860–870
Grefkes C, Fink GR (2011) Reorganization of cerebral networks after stroke: new insights from neuroimaging with connectivity approaches. Brain 134:1264–1276
Grefkes C, Ward NS (2014) Cortical reorganization after stroke: how much and how functional? Neuroscientist 20:56–70
Harris-Love ML, Harrington RM (2017) Non-invasive brain stimulation to enhance upper limb motor practice poststroke: a model for selection of cortical site. Front Neurol 8:224. https://doi.org/10.3389/fneur.2017.00224
Hummel FC, Cohen LG (2006) Non-invasive brain stimulation: a new strategy to improve neurorehabilitation after stroke? Lancet Neurol 5:708–712
Jaillard A, Martin CD, Garambois K, Lebas JF, Hommel M (2005) Vicarious function within the human primary motor cortex? A longitudinal fMRI stroke study. Brain 128:1122–1138
Katan M, Luft A (2018) Global burden of stroke. Semin Neurol 38:208–211. https://doi.org/10.1055/s-0038-1649503
Kelly-Hayes M, Beiser A, Kase CS, Scaramucci A, D'Agostino RB, Wolf PA (2003) The influence of gender and age on disability following ischemic stroke: the Framingham study. J Stroke Cerebrovasc Dis 12:119–126. https://doi.org/10.1016/S1052-3057(03)00042-9
Khedr EM, Ahmed MA, Fathy N, Rothwell JC (2005) Therapeutic trial of repetitive transcranial magnetic stimulation after acute ischemic stroke. Neurology 65:466–468
Khedr EM, Shawky OA, El-Hammady DH, Rothwell JC, Darwish ES, Mostafa OM, Tohamy AM (2013) Effect of anodal versus cathodal transcranial direct current stimulation on stroke rehabilitation: a pilot randomized controlled trial. Neurorehabil Neural Repair 27:592–601
Kim D-Y, Lim J-Y, Kang EK, You DS, Oh M-K, Oh B-M, Paik N-J (2010) Effect of transcranial direct current stimulation on motor recovery in patients with subacute stroke. Am J Phys Med Rehabil 89:879–886
Kubis N (2016) Non-invasive brain stimulation to enhance post-stroke recovery. Front Neural Circ 10:56
Levy CE, Nichols DS, Schmalbrock PM, Keller P, Chakeres DW (2001) Functional MRI evidence of cortical reorganization in upper-limb stroke hemiplegia treated with constraint-induced movement therapy. Am J Phys Med Rehabil 80:4–12
Lewis GN, Byblow WD (2004) Bimanual coordination dynamics in poststroke hemiparetics. J Mot Behav 36:174–188. https://doi.org/10.3200/JMBR.36.2.174-188
Luft AR, McCombe-Waller S, Whitall J, Forrester LW, Macko R, Sorkin JD, Schulz JB, Goldberg AP, Hanley DF (2004) Repetitive bilateral arm training and motor cortex activation in chronic stroke: a randomized controlled trial. Jama 292:1853–1861
McCambridge AB, Stinear JW, Byblow WD (2018) Revisiting interhemispheric imbalance in chronic stroke: a tDCS study. Clin Neurophysiol 129:42–50
McDonnell MN, Stinear CM (2017) TMS measures of motor cortex function after stroke: a meta-analysis. Brain Stimul 10:721–734. https://doi.org/10.1016/j.brs.2017.03.008
Nowak DA, Grefkes C, Ameli M, Fink GR (2009a) Interhemispheric competition after stroke: brain stimulation to enhance recovery of function of the affected hand. Neurorehabil Neural Repair 23:641–656. https://doi.org/10.1177/1545968309336661
Nowak DA, Hufnagel A, Ameli M, Timmann D, Hermsdorfer J (2009b) Interhemispheric transfer of predictive force control during grasping in cerebellar disorders. Cerebellum 8:108–115. https://doi.org/10.1007/s12311-008-0081-5
Plow E, Sankarasubramanian V, Cunningham D, Potter-Baker K, Varnerin N, Cohen L et al (2016) Models to tailor brain stimulation therapies in stroke. Neural Plast. https://doi.org/10.1155/2016/4071620
Rossi S, Hallett M, Rossini PM, Pascual-Leone A, Group SoTC (2009) Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol 120:2008–2039
Rosso C, Lamy JC (2018) Does resting motor threshold predict motor hand recovery after stroke? Front Neurol 9:1020. https://doi.org/10.3389/fneur.2018.01020
Sebastianelli L, Versace V, Martignago S, Brigo F, Trinka E, Saltuari L, Nardone R (2017) Low-frequency rTMS of the unaffected hemisphere in stroke patients: a systematic review. Acta Neurol Scand 136:585–605
Simis M, Di Lazzaro V, Kirton A et al (2016) Neurophysiological measurements of affected and unaffected motor cortex from a cross-sectional, multi-center individual stroke patient data analysis study. Clin Neurophysiol 46:53–61
Stewart JC, Dewanjee P, Tran G, Quinlan EB, Dodakian L, McKenzie A, See J, Cramer SC (2017) Role of corpus callosum integrity in arm function differs based on motor severity after stroke. Neuroimage Clin 14:641–647. https://doi.org/10.1016/j.nicl.2017.02.023
Stinear CM, Barber PA, Smale PR, Coxon JP, Fleming MK, Byblow WD (2006) Functional potential in chronic stroke patients depends on corticospinal tract integrity. Brain 130:170–180
Takeuchi N, Chuma T, Matsuo Y, Watanabe I, Ikoma K (2005) Repetitive transcranial magnetic stimulation of contralesional primary motor cortex improves hand function after stroke. Stroke 36:2681–2686
Theilig S, Podubecka J, Bösl K, Wiederer R, Nowak DA (2011) Functional neuromuscular stimulation to improve severe hand dysfunction after stroke: does inhibitory rTMS enhance therapeutic efficiency? Exp Neurol 230:149–155
Thickbroom GW, Cortes M, Rykman A et al (2015) Stroke subtype and motor impairment influence contralesional excitability. Neurology 85:517–520
Veldema J, Bösl K, Nowak DA (2018) Cortico-spinal excitability and hand motor recovery in stroke: a longitudinal study. J Neurol 265:1071–1078
Ward N (2011) Assessment of cortical reorganisation for hand function after stroke. J Physiol 589:5625–5632. https://doi.org/10.1113/jphysiol.2011.220939
Ward NS, Newton JM, Swayne OB, Lee L, Frackowiak RS, Thompson AJ, Greenwood RJ, Rothwell JC (2007) The relationship between brain activity and peak grip force is modulated by corticospinal system integrity after subcortical stroke. Eur J Neurosci 25:1865–1873
Webster BR, Celnik PA, Cohen LG (2006) Noninvasive brain stimulation in stroke rehabilitation. NeuroRx 3:474–481
Woytowicz EJ, Rietschel JC, Goodman RN, Conroy SS, Sorkin JD, Whitall J, McCombe Waller S (2017) Determining levels of upper extremity movement impairment by applying a cluster analysis to the Fugl-Meyer assessment of the upper extremity in chronic stroke. Arch Phys Med Rehabil 98:456–462. https://doi.org/10.1016/j.apmr.2016.06.023
Xu H, Qin W, Chen H, Jiang L, Li K, Yu C (2014) Contribution of the resting-state functional connectivity of the contralesional primary sensorimotor cortex to motor recovery after subcortical stroke. PLoS One 9:e84729
Zhu LL, Lindenberg R, Alexander MP, Schlaug G (2010) Lesion load of the corticospinal tract predicts motor impairment in chronic stroke. Stroke 41:910–915
Funding
Marina Berenguer was supported by the Fundação de Amparo à Ciência e Tecnologia (FACEPE: IBPG-1473-4.08/16), Brazil. Adriana Baltar was supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES). Sérgio Rocha was supported by the Fundação de Amparo à Ciência e Tecnologia (FACEPE: IBPG-1649-4.08/13). Lívia Shirahige is supported by the Fundação de Amparo à Ciência e Tecnologia (FACEPE: IBPG-1548-4.01/16). Monte-Silva K is supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (308291/2015-8), Brazil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Ethics Committee approval: University Research Ethics Committee
Informed consent
Written informed consent was obtained from all patients.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• Interhemispheric asymmetry in stroke patients is related to with sensory-motor impairment.
• Sensory-motor severity of stroke is not dependent of lower activity on affected motor cortex.
• Sensory-motor severity of stroke is related to unaffected motor cortex.
• The stroke chronicity does not influence the interhemispheric asymmetry.
Rights and permissions
About this article
Cite this article
Berenguer-Rocha, M., Baltar, A., Rocha, S. et al. Interhemispheric asymmetry of the motor cortex excitability in stroke: relationship with sensory-motor impairment and injury chronicity. Neurol Sci 41, 2591–2598 (2020). https://doi.org/10.1007/s10072-020-04350-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04350-4