Abstract
Introduction
In carpal tunnel release, it is yet unclear whether a learning curve exists among surgeons. The aim of our study was to investigate if outcome after carpal tunnel release is dependent on surgeon’s experience and to get an impression of the learning curve for this procedure.
Methods
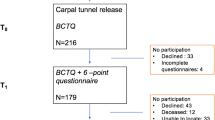
A total of 188 CTS patients underwent carpal tunnel release. Patients completed the Boston Carpal Tunnel Questionnaire at baseline and 6–8 months postoperatively together with a six-point scale for perceived improvement.
Results
Patients operated by an experienced resident or certified surgeon reported a favorable outcome more often than patients operated by an inexperienced resident (adjusted OR 3.23 and adjusted OR 3.16, respectively). In addition, a negative association was found between surgeon’s years of experience and postoperative Symptom Severity Scale and Functional Status Scale scores.
Discussion
Outcome after carpal tunnel release seems to be dependent on surgical experience, and there is a learning curve in residents.

Similar content being viewed by others
References
Padua L, Coraci D, Erra C, Pazzaglia C, Paolasso I, Loreti C, Caliandro P, Hobson-Webb LD (2016) Carpal tunnel syndrome: clinical features, diagnosis, and management. Lancet Neurol 15(12):1273–1284. https://doi.org/10.1016/S1474-4422(16)30231-9
Jansen MC, Evers S, Slijper HP, de Haas KP, Smit X, Hovius SE, Selles RW (2018) Predicting clinical outcome after surgical treatment in patients with carpal tunnel syndrome. J Hand Surg Am 43:1098–1106.e1. https://doi.org/10.1016/j.jhsa.2018.05.017
Bland JD (2001) Do nerve conduction studies predict the outcome of carpal tunnel decompression? Muscle Nerve 24(7):935–940
Longstaff L, Milner RH, O'Sullivan S, Fawcett P (2001) Carpal tunnel syndrome: the correlation between outcome, symptoms and nerve conduction study findings. J Hand Surg Br 26(5):475–480. https://doi.org/10.1054/jhsb.2001.0616
Conzen C, Conzen M, Rubsamen N, Mikolajczyk R (2016) Predictors of the patient-centered outcomes of surgical carpal tunnel release - a prospective cohort study. BMC Musculoskelet Disord 17:190. https://doi.org/10.1186/s12891-016-1046-3
Choi SJ, Ahn DS (1998) Correlation of clinical history and electrodiagnostic abnormalities with outcome after surgery for carpal tunnel syndrome. Plast Reconstr Surg 102(7):2374–2380
Concannon MJ, Gainor B, Petroski GF, Puckett CL (1997) The predictive value of electrodiagnostic studies in carpal tunnel syndrome. Plast Reconstr Surg 100(6):1452–1458
Chen SJ, Lin HS, Hsieh CH (2013) Carpal tunnel pressure is correlated with electrophysiological parameters but not the 3 month surgical outcome. J Clin Neurosci 20(2):272–277. https://doi.org/10.1016/j.jocn.2012.03.032
Warnack E, Simon J, Dang Q, Catino J, Bukur M (2018) Wiser with age? Increased per-surgeon elderly patient volume is associated with lower postinjury complications. Am Surg 84(6):1027–1032
Honegger J, Grimm F (2018) The experience with transsphenoidal surgery and its importance to outcomes. Pituitary 21:545–555. https://doi.org/10.1007/s11102-018-0904-4
Cahill PJ, Pahys JM, Asghar J, Yaszay B, Marks MC, Bastrom TP, Lonner BS, Shah SA, Shufflebarger HL, Newton PO, Betz RR, Samdani AF (2014) The effect of surgeon experience on outcomes of surgery for adolescent idiopathic scoliosis. J Bone Joint Surg Am 96(16):1333–1339. https://doi.org/10.2106/JBJS.M.01265
Hsu CE, Lin TK, Lee MH, Lee ST, Chang CN, Lin CL, Hsu YH, Huang YC, Hsieh TC, Chang CJ (2016) The impact of surgical experience on major intraoperative aneurysm rupture and their consequences on outcome: a multivariate analysis of 538 microsurgical clipping cases. PLoS One 11(3):e0151805. https://doi.org/10.1371/journal.pone.0151805
Sgroi MD, Darby GC, Kabutey NK, Barleben AR, Lane JS 3rd, Fujitani RM (2015) Experience matters more than specialty for carotid stenting outcomes. J Vasc Surg 61(4):933–938. https://doi.org/10.1016/j.jvs.2014.11.066
Prystowsky JB, Bordage G, Feinglass JM (2002) Patient outcomes for segmental colon resection according to surgeon's training, certification, and experience. Surgery 132(4):663–670 discussion 670-662
Evers S, Jansen MC, Slijper HP, de Haas N, Smit X, Porsius JT, Hovius SER, Amadio PC, Selles RW (2018) Hand surgeons performing more open carpal tunnel releases do not show better patient outcomes. Plast Reconstr Surg 141(6):1439–1446. https://doi.org/10.1097/PRS.0000000000004369
Claes F, Kasius KM, Meulstee J, Verhagen WI (2013) Comparing a new ultrasound approach with electrodiagnostic studies to confirm clinically defined carpal tunnel syndrome: a prospective, blinded study. Am J Phys Med Rehabil 92(11):1005–1011. https://doi.org/10.1097/PHM.0b013e31829b4bd8
Leite JC, Jerosch-Herold C, Song F (2006) A systematic review of the psychometric properties of the Boston carpal tunnel questionnaire. BMC Musculoskelet Disord 7:78. https://doi.org/10.1186/1471-2474-7-78
Beck JD, Deegan JH, Rhoades D, Klena JC (2011) Results of endoscopic carpal tunnel release relative to surgeon experience with the Agee technique. J Hand Surg Am 36(1):61–64. https://doi.org/10.1016/j.jhsa.2010.10.017
Serra L, Panagiotopoulos K, Bucciero A, Mehrabi FK, Pescatore G, Santangelo M, Vizioli L (2003) Endoscopic release in carpal tunnel syndrome: analysis of clinical results in 200 cases. Minim Invasive Neurosurg 46(1):11–15. https://doi.org/10.1055/s-2003-37966
Makowiec RL, Nagle DJ, Chow JC (2002) Outcome of first-time endoscopic carpal tunnel release in a teaching environment. Arthroscopy 18(1):27–31
Chow JC (1994) Endoscopic carpal tunnel release. Two-portal technique. Hand Clin 10(4):637–646
De Kleermaeker F, Boogaarts HD, Meulstee J, Verhagen WIM (2018) Minimal clinically important difference for the Boston carpal tunnel questionnaire: new insights and review of literature. J Hand Surg Eur 44:283–289. https://doi.org/10.1177/1753193418812616
Turner A, Kimble F, Gulyas K, Ball J (2010) Can the outcome of open carpal tunnel release be predicted?: a review of the literature. ANZ J Surg 80(1–2):50–54. https://doi.org/10.1111/j.1445-2197.2009.05175.x
Straub TA (1999) Endoscopic carpal tunnel release: a prospective analysis of factors associated with unsatisfactory results. Arthroscopy 15(3):269–274
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49(12):1373–1379
Harrell FE (2001) Regression modeling strategies with applications to linear models, logistic regression and survival analysis. Springer-Verlag, New York
Amadio PC, Silverstein MD, Ilstrup DM, Schleck CD, Jensen LM (1996) Outcome assessment for carpal tunnel surgery: the relative responsiveness of generic, arthritis-specific, disease-specific, and physical examination measures. J Hand Surg Am 21(3):338–346. https://doi.org/10.1016/S0363-5023(96)80340-6
Greenslade JR, Mehta RL, Belward P, Warwick DJ (2004) Dash and Boston questionnaire assessment of carpal tunnel syndrome outcome: what is the responsiveness of an outcome questionnaire? J Hand Surg Br 29(2):159–164. https://doi.org/10.1016/j.jhsb.2003.10.010
Merolli A, Luigetti M, Modoni A, Masciullo M, Lucia Mereu M, Lo Monaco M (2013) Persistence of abnormal electrophysiological findings after carpal tunnel release. J Reconstr Microsurg 29(8):511–516. https://doi.org/10.1055/s-0033-1348038
Schrijver HM, Gerritsen AA, Strijers RL, Uitdehaag BM, Scholten RJ, de Vet HC, Bouter LM (2005) Correlating nerve conduction studies and clinical outcome measures on carpal tunnel syndrome: lessons from a randomized controlled trial. J Clin Neurophysiol 22(3):216–221
Acknowledgements
The authors would like to thank all the participants who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Permission from the local Medical Ethics Committee (Medisch Spectrum Twente) was obtained. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
De Kleermaeker, F.G.C.M., Meulstee, J., Claes, F. et al. Outcome after carpal tunnel release: effects of learning curve. Neurol Sci 40, 1813–1819 (2019). https://doi.org/10.1007/s10072-019-03908-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-019-03908-1