Abstract
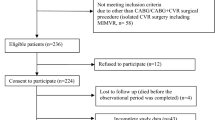
Post-stroke anxiety (PSA) is a common neuropsychiatric affective disorder occurring after stroke. The purpose of this study was to investigate the association between anxiety and the serum levels of oxidative stress markers at admission. First-ever or recurrent ischemic stroke patients were consecutively recruited into the study and followed up 1 month. Patients were divided into PSA and non-PSA group according DSM-IV criteria for anxiety due to stroke. Overall, 49 patients (24.1%) were diagnosed anxiety. Serum GPX (glutathione peroxidase), CAT (catalase), SOD (superoxide dismutase), and MDA (malondialdehyde) were significantly higher in patients with anxiety than patients without anxiety. The HAM-A scores had a significant positive association with MDA levels. In multivariate logistic regression analysis, serum antioxidant enzymes and MDA were independent predictors of PSA. An increased risk of PSA was associated with serum MDA levels ≥ 3.0 nmol/ml (adjusted OR 8.68, 95% CI 3.02–24.95; P < 0.001) after adjusting for relevant confounders such as social support and treatments at admission. Elevated serum levels of lipid oxidation products and antioxidant enzymes at admission were associated with anxiety 1 month after stroke, suggesting that these alterations might participate in the pathophysiology of anxiety symptoms in stroke patients.



Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- NIHSS:
-
National Institutes of Health Stroke Scale
- MMSE:
-
Mini-mental state examination
- PSQI:
-
Pittsburgh Sleep Quality Index
- SSRS:
-
Social Support Rating Scale
- BI:
-
Modified Barthel Index
- PSA:
-
Post-stroke anxiety
- FBG:
-
Fasting blood glucose
- TG:
-
Total cholesterol
- Hs-CRP:
-
High-sensitivity C-reactive protein
- GPX:
-
Glutathione peroxidase
- CAT:
-
Catalase
- SOD:
-
Superoxide dismutase
- MDA:
-
Malondialdehyde
- 95% CI:
-
95% Confidence interval
- OR:
-
Odds ratio
References
Campbell Burton CA, Murray J, Holmes J et al (2013) Frequency of anxiety after stroke: a systematic review and meta-analysis of observational studies. Int J Stroke 8:545–559
Chun HY, Whiteley WN, Carson A et al (2015) Anxiety after stroke: time for an intervention. Int J Stroke 10:655–656
Cumming TB, Blomstrand C, Skoog I, Linden T (2016) The high prevalence of anxiety disorders after stroke. Am J Geriatr Psychiatry 24:154–160
Lincoln NB, Brinkmann N, Cunningham S, Dejaeger E, de Weerdt W, Jenni W, Mahdzir A, Putman K, Schupp W, Schuback B, de Wit L (2013) Anxiety and depression after stroke: a 5 year follow-up. Disabil Rehabil 35:140–145
Ayerbe L, Ayis SA, Crichton S, Wolfe CDA, Rudd AG (2014) Natural history, predictors and associated outcomes of anxiety up to 10 years after stroke: the South London Stroke Register. Age Ageing 43:542–547
Johnson GA (1991) Research into psychiatric disorder after stroke: the need for further studies. Aust N Z J Psychiatry 25:358–370
Lambiase MJ, Kubzansky LD, Thurston RC (2014) Prospective study of anxiety and incident stroke. Stroke 45:438–443
Menlove L, Crayton E, Kneebone I, Allen-Crooks R, Otto E, Harder H (2015) Predictors of anxiety after stroke: a systematic review of observational studies. J Stroke Cerebrovasc Dis 24:1107–1117
Xu Y, Wang C, Klabnik JJ, O' Donnell J (2014) Novel therapeutic targets in depression and anxiety: antioxidants as a candidate treatment. Curr Neuropharmacol 12:108–119
Smaga I, Niedzielska E, Gawlik M, Moniczewski A, Krzek J, Przegaliński E, Pera J, Filip M (2015) Oxidative stress as an etiological factor and a potential treatment target of psychiatric disorders. Part 2. Depression, anxiety, schizophrenia and autism. Pharmacol Rep 67:569–580
Gökçe Çokal B, Yurtdaş M, Keskin Güler S, Güneş HN, Ataç Uçar C, Aytaç B, Durak ZE, Yoldaş TK, Durak İ, Çubukçu HC (2017) Serum glutathione peroxidase, xanthine oxidase, and superoxide dismutase activities and malondialdehyde levels in patients with Parkinson’s disease. Neurol Sci 38:425–431
Çokal BG, Aytaç B, Durak ZE et al (2015) Serum oxidant and antioxidant status of patients with chronic tension-type headache: possible effects of medical treatment. Neurol Sci 36:1–5
Moylan S, Maes M, Wray NR, Berk M (2013) The neuroprogressive nature of major depressive disorder: pathways to disease evolution and resistance, and therapeutic implications. Mol Psychiatry 18:595–606
Islam MR, Ahmed MU, Islam MS et al (2013) Comparative analysis of serum malondialdehyde, antioxidant vitamins and immunoglobulin levels in patients suffering from generalized anxiety disorder. Drug Res 64:406–411
Matsumoto K, Yobimoto K, Huong NTT, Abdel-Fattah M, van Hien T, Watanabe H (1999) Psychological stress-induced enhancement of brain lipid peroxidation via nitric oxide systems and its modulation by anxiolytic and anxiogenic drugs in mice. Brain Res 839:74–84
Kuloglu M, Atmaca M, Tezcan E, Gecici Ö, Tunckol H, Ustundag B (2002) Antioxidant enzyme activities and malondialdehyde levels in patients with obsessive-compulsive disorder. Neuropsychobiology 46:27–32
Ozdemi̇r E, Ceti̇nkaya S, Ersan S et al (2009) Serum selenium and plasma malondialdehyde levels and antioxidant enzyme activities in patients with obsessive-compulsive disorder. Prog Neuro-Psychopharmacol Biol Psychiatry 33:62–65
Tezcan E, Atmaca M, Kuloglu M, Ustundag B (2003) Free radicals in patients with post-traumatic stress disorder. Eur Arch Psychiatry Clin Neurosci 253:89–91
Milanlioglu A, Aslan M, Ozkol H, Çilingir V, Nuri Aydın M, Karadas S (2016) Serum antioxidant enzymes activities and oxidative stress levels in patients with acute ischemic stroke: influence on neurological status and outcome. Wien Klin Wochenschr 128:169–174
Cheng Y, Liu C, Mao C, Qian J, Liu K, Ke G (2008) Social support plays a role in depression in Parkinson's disease: a cross-section study in a Chinese cohort. Parkinsonism Relat Disord 14:43–45
Brott T, Adams HP, Olinger CP, Marler JR, Barsan WG, Biller J, Spilker J, Holleran R, Eberle R, Hertzberg V (1989) Measurements of acute cerebral infarction: a clinical examination scale. Stroke 20:864–870
Jr AH, Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel index. Md State Med J 14:61–65
Folstein MF, Robins LN, Helzer JE (1983) The mini-mental state examination. Arch Gen Psychiatry 40:812
Buysse DJ, Reynolds CF 3rd, Monk TH et al (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Hamilton M (1959) The assessment of anxiety states by rating. Br J Med Psychol 32:50–55
Lobbestael J, Leurgans M, Arntz A (2011) Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I disorders (SCID I) and Axis II disorders (SCID II). Clin Psychol Psychother 18:75–79
Youden WJ (1950) Index for rating diagnosis tests. Cancer 3:32–35
Atmaca M, Kuloglu M, Tezcan E, Ustundag B (2008) Antioxidant enzyme and malondialdehyde levels in patients with social phobia. Psychiatry Res 159:95–100
Behl A, Swami G, Sircar SS, Bhatia MS, Banerjee BD (2010) Relationship of possible stress-related biochemical markers to oxidative/antioxidative status in obsessive-compulsive disorder. Neuropsychobiology 61:210–214
Shichiri M (2014) The role of lipid peroxidation in neurological disorders. J Clin Biochem Nutr 54:151–160
Davies SJ, Allgulander C (2013) Anxiety and cardiovascular disease. Mod Trends Pharmacopsychiatri 29:85–97
Li H, Horke S, Forstermann U (2013) Oxidative stress in vascular disease and its pharmacological prevention. Trends Pharmacol Sci 34:313–319
Zhang L, Wu J, Duan X et al (2016) NADPH oxidase: a potential target for treatment of stroke. Oxidative Med Cell Longev 2016:5026984
Dirnagl U, Iadecola C, Moskowitz MA (1999) Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci 22:391–397
Garcia-Yebenes I, Sobrado M, Moraga A et al (2012) Iron overload, measured as serum ferritin, increases brain damage induced by focal ischemia and early reperfusion. Neurochem Int 61:1364–1369
Wang J, Lei H, Hou J et al (2015) Involvement of oxidative stress in SAMP10 mice with age-related neurodegeneration. Neurol Sci 36:1–8
McCubrey JA, Lahair MM, Franklin RA (2006) Reactive oxygen species-induced activation of the MAP kinase signaling pathways. 8:1775–89
Wang X, Lei XG, Wang J (2014) Malondialdehyde regulates glucose-stimulated insulin secretion in murine islets via TCF7L2-dependent Wnt signaling pathway. Mol Cell Endocrinol 382:8–16
Ambade A, Mandrekar P (2012) Oxidative stress and inflammation: essential partners in alcoholic liver disease. Int J Hepatol 2012:853175 1, 9
Xu G, Luo K, Liu H, Huang T, Fang X, Tu W (2015) The progress of inflammation and oxidative stress in patients with chronic kidney disease. Ren Fail 37:45–49
Pandya CD, Howell KR, Pillai A (2013) Antioxidants as potential therapeutics for neuropsychiatric disorders. Prog Neuro-Psychopharmacol Biol Psychiatry 46:214–223
Bouayed J (2010) Polyphenols: a potential new strategy for the prevention and treatment of anxiety and depression. Curr Nutr Food Sci 6:13–18
Pajović SB, Pejić S, Stojiljković V, Gavrilović L, Dronjak S, Kanazir DT (2006) Alterations in hippocampal antioxidant enzyme activities and sympatho-adrenomedullary system of rats in response to different stress models. Physiol Res 55:453–460
Maldonado-Bouchard S, Peters K, Woller SA, Madahian B, Faghihi U, Patel S, Bake S, Hook MA (2016) Inflammation is increased with anxiety- and depression-like signs in a rat model of spinal cord injury. Brain Behav Immun 51:176–195
Pierce GL, Kalil GZ, Ajibewa T, Holwerda SW, Persons J, Moser DJ, Fiedorowicz JG (2017) Anxiety independently contributes to elevated inflammation in humans with obesity. Obesity (Silver Spring) 25:286–289
Robinson RG, Jorge RE (2016) Post-stroke depression: a review. Am J Psychiatry 173:221–231
Herrmann N, Black SE, Lawrence J, Szekely C, Szalai JP (1998) The Sunnybrook Stroke Study: a prospective study of depressive symptoms and functional outcome. Stroke 29:618–624
Funding
This work was supported by the National Key Technology Research and Development Program of the Ministry of Science and Technology of China (grant number: 2015BAI13B01) and Wenzhou Municipal Sci-Tech Bureau Program (grant number:Y20160002).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Electronic supplementary material
ESM 1
(DOCX 51 kb)
Rights and permissions
About this article
Cite this article
Liu, Z., Cai, Y., Zhang, X. et al. High serum levels of malondialdehyde and antioxidant enzymes are associated with post-stroke anxiety. Neurol Sci 39, 999–1007 (2018). https://doi.org/10.1007/s10072-018-3287-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-018-3287-4