Abstract
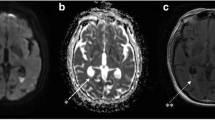
The aim of the study is to explore the experiences in diagnosis and treatment of severe neurosurgical patients with pyogenic ventriculitis caused by gram-negative bacteria (G−). Nineteen patients with pyogenic ventriculitis were reviewed for their treatment. The bacterial testing results of cerebrospinal fluid (CSF), the clinical intervention, and the patients’ prognosis were evaluated. The bacterial smears of ventricular drainage from all the cases were G− bacteria. Head CT and MRI scans confirmed that they were intraventricular empyema. Eighteen cases of CSF bacterial test were positive, including 12 cases of Acinetobacter baumannii positive, 2 of Klebsiella pneumonia positive, 2 of Serratia marcescens positive, 1 of Pseudomonas maltophila positive, and 1 case of Escherichia coli positive. One case of the bacterial culture was negative. All patients were treated by using intraventricular lavage in combination with intravenous and intraventricular antibiotics in accordance with the clinical conditions. After treatment for 2 to 8 weeks, 14 patients were cured (74%) and 5 were died (26%). Eight patients who were cured had received ventriculoperitoneal shunt due to hydrocephalus at 2 to 6 weeks after infection controlled, and none of them had any reinfection. Twelve of the 14 cured cases came to consciousness, but 2 were persistent in vegetative state starting before the infection; they did not show any improving consciousness after infection had been cured. Suppurative ventriculitis in severe neurosurgical patients is mainly infected by G− with a higher mortality. Early diagnosis, especially in identifying pathogen types, timely ventricular irrigation, and ventricular drainage together with intravenous and intraventricular antibiotic treatment, should improve prognosis.
Similar content being viewed by others
References
Akhaddar A (2017) Pyogenic ventriculitis. Atlas of Infections in Neurosurgery and Spinal Surgery. Springer, Champions 2017; 105–110
Jorens PG, Voormolen MH, Robert D, Parizel PM (2009) Imaging findings in pyogenic ventriculitis. Neurocrit Care 11:403–405
Zambito Marsala S, Gioulis M, Pistacchi M (2015) Cerebrospinal fluid and lumbar puncture: the story of a necessary procedure in the history of medicine. Neurol Sci 36:1011–1015
Becker DP, Nulsen FE (1968) Control of hydrocephalus by valve-regulated venous shunt: avoidance of complications in prolonged shunt maintenance. J Neurosurg 28:215–226
Wang F, Yao XY, Zou ZR, HL Y, Sun T (2017) Management of pyogenic cerebral ventriculitis by neuroendoscopic surgery. World Neurosurg 98:6–13
Rolinson GN, Russell EJ (1972) New method for antibiotic susceptibility testing. Antimicrob Agents Chemother 2:51–56
Jennett B, Bond M (1975) Assessment of outcome after severe brain damage. Lancet 1:480–484. https://doi.org/10.1016/S0140-6736(75)92830-5.
Xu M, Shi ZH, Chen GQ, Zhao JW, Shi GZ, Wang T, Wang T, Tang MZ (2014) Zhou JX (2014) A retrospective analysis of post-craniotomy intracranial infection in pediatric patients with supratentorial neurosurgical operation: incidence, risk factors and outcomes. Chin J Neurosurg 30:1249–1252
Srinivas D, Veena Kumari HB, Somanna S, Bhagavatula I, Anandappa CB (2011) The incidence of postoperative meningitis in neurosurgery: an institutional experience. Neurol India 59:195–198
Neuberger A, Shofty B, Bishop B, Naffaa ME, Binawi T, Babich T, Rappaport ZH, Zaaroor M, Sviri G, Yahav D, Paul M (2016) Risk factors associated with death or neurological deterioration among patients with Gram-negative postneurosurgical meningitis. Clin Microbiol Infect 22:573.e1–573.e4
Kim BN, Peleg AY, Lodise TP, Lipman J, Li J, Nation R, Paterson DL (2009) Management of meningitis due to antibiotic-resistant Acinetobacter species. Lancet Infect Dis 9:245–255
Zhang XJ, YC X, YS Y et al (2012) Chinet 2010 surveillance of bacterial distribution and resistance in sterile body fluids. Chin J Infect Chemother 12:259–267
Li Y (2012) Zhang GL (2012) Experience of the diagnosis and treatment of intracranial infection caused by multi drug resistant acinetobactor species. Chin Remedies Clin 12:107–109
Li TH, Song LJ, Guo FY, Sun HW, Ma SQ (2013) Experience of the diagnosis and treatment of empyema and ventriculitis caused by multi drug resistant acinetobactor sepcies. Chin J Pract Nerv dis 16:24–25
Li ZQ, Wu X, Hu J, Gao L, XH W, Jin Y, Yu J, Sun YR, ZY D (2014) Clinical experience summary and analysis of the patients with intracranial infeciton secondary to brain injury. Chinese. J Neurosurg 30:1115–1119
Qiu BH, Qi ST, Zeng H, Mo YP, SX X (2014) Treatment of intracranial infeciton due to drug-resistant Acinetobacter Baumannii in neurosurgical. Chinese. J Neurosurg 30:586–588
Liu CG, Cheng H, Xu CL, Sun Z, Wang T (2014) The clinical analysis of the treatment of severe ventricular inflammation by continuous drainage of bilateral ventricular drainage and lavage in the brain. Chin J Pract Nerv Dis 17:64–65
Min Q, Wei JW (2007) Treatment for the pyogenic ventriculitis by continuous ventricle lavage. Chinese Journal of postgraduates of. Medicine 30:37–38
Zhang YZ (2011) Surgery of the cerebral ventricle. The people’s medical publishing house. 1st Edit
C CNS (2012) Expert consensus on application of antibiotics in nosocomial infection in department of neurosurgery. Natl Med J China 93:322–329
Worthington RJ, Meander C (2013) Combination approaches to combat multidrug-resistant bacteria. Trends Biotechnol 31:177–184
Cascio A, Conti A, Sinardi L, Iaria C, Angileri FF, Stassi G, David T, Versaci A, Iaria M, David A (2010) Post-neurosurgical multidrug-resistant Acinetobacter baumannii meningitis successfully treated with intrathecal colistin. A new case and a systematic review of the literature. Int. J Infect Dis 14:e572–e579
Guan F, ZQ H, Huang H, Ren ZY, Wang ZY, JD F, Li YB, Liu B, Xing B (2014) Strategy of neuroendoscopic diagnosis and treatment for ventricular system infeciton. Chinese. J Neurosurg 30:377–380
Acknowledgements
None.
Funding information
None.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shang, F., Xu, Y., Wang, N. et al. Diagnosis and treatment of severe neurosurgical patients with pyogenic ventriculitis caused by gram-negative bacteria. Neurol Sci 39, 79–84 (2018). https://doi.org/10.1007/s10072-017-3146-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-017-3146-8