Abstract
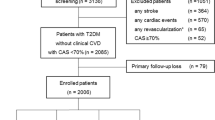
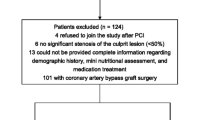
The risk factors for post-procedural events after carotid artery stenting (CAS) have not been well established. The aim of this study was to investigate the association between metabolic syndrome (MetS) and the risk of post-CAS complications. A total of 358 consecutive patients who underwent CAS were enrolled in this prospective study. Patients’ demographic data, clinical characteristics, and complications after CAS within 30 days were recorded. Logistic regression analysis was performed to identify possible risk factors for post-procedural complications after CAS. The incidence of complications after CAS within 30 days was 7.0%. Logistic regression analysis identified the following as independent risk factors for 30-day transient ischemic attacks, stroke, myocardial infarction, and death after CAS: metabolic syndrome (OR = 2.31, 95% CI 1.91–3.01, P = 0.004), diabetes (OR = 2.24, 95% CI 1.74–2.76, P = 0.026), symptomatic patient (OR = 1.73, 95% CI 1.23–3.05, P = 0.011), and age (OR = 1.87, 95% CI 1.35–2.57, P = 0.042). Among the components of MetS, central obesity (OR = 2.21, 95% CI 1.24–2.63, P = 0.006), low high-density lipoprotein cholesterol (HDL-C) (OR = 1.66, 95% CI 1.34–2.27, P = 0.022), and high fasting plasma glucose (OR = 2.32, 95% CI 1.85–2.74, P = 0.003) were associated with increased risk of 30-day complications after CAS. This present study suggests that patients with metabolic syndrome have significantly increased risk of complications after CAS within 30 days. Moreover, MetS patients with central obesity, high fasting plasma glucose, or low HDL-C have significantly increased risk of complications after CAS within 30 days.
Similar content being viewed by others
References
Suri MF, Qiao Y, Ma X, Guallar E, Zhou J, Zhang Y (2016) Prevalence of intracranial atherosclerotic stenosis using high-resolution magnetic resonance angiography in the general population: the atherosclerosis risk in communities study. Stroke 47(5):1187. doi:10.1161/STROKEAHA.115.011292
Abbott AL, Paraskevas KI, Kakkos SK, Golledge J, Eckstein HH, Diaz-Sandoval LJ (2015) Systematic review of guidelines for the management of asymptomatic and symptomatic carotid stenosis. Stroke 46(11):32–88. doi:10.1161/STROKEAHA.115.011292
Furie KL, Kasner SE, Adams RJ, Albers GW, Bush RL, Fagan SC (2011) Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the american heart association/american stroke asso ciation. Stroke 42(1):227–276. doi:10.1161/STR.0b013e3181f7d043
Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S (2011) Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 42(2):517–584. doi:10.1161/STR.0b013e3181fcb238
Rosenfield K, Matsumura JS, Chaturvedi S et al (2016) Randomized trial of stent versus surgery for asymptomatic carotid stenosis. N Engl J Med 64(2):536–536. doi:10.1056/NEJMoa1515706
Economopoulos KP, Sergentanis TN, Tsivgoulis G, Mariolis AD, Stefanadis C (2011) Carotid artery stenting versus carotid endarterectomy: a comprehensive meta-analysis of short-term and long-term outcomes. Stroke 42(3):687–692. doi:10.1161/STROKEAHA.110.606079
Brott TG, Hobson RW, Howard G, Roubin GS, Clark WM, Brooks W (2010) Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med 363(1):11–23. doi:10.1056/NEJMoa0912321
Hobeanu C, Lavallée PC, Rothwell PM (2017) Symptomatic patients remain at substantial risk of arterial disease complications before and after endarterectomy or stenting. Stroke 48(4):1005. doi:10.1161/STROKEAHA.116.015171
Stingele R, Berger J, Alfke K, Eckstein HH, Fraedrich G, Allenberg J (2008) Clinical and angiographic risk factors for stroke and death within 30 days after carotid endarterectomy and stent-protected angioplasty: a subanalysis of the SPACE study. Lancet Neurol 7(3):216–222. doi:10.1016/S1474-4422(08)70024-3
Setacci C, Chisci E, Setacci F, Iacoponi F, de Donato G, Rossi A (2010) Siena carotid artery stenting score: a risk modelling study for individual patients. Stroke 41(6):1259–1265. doi:10.1161/STROKEAHA.110.578583
Sayeed S, Stanziale SF, Wholey MH, Makaroun MS (2008) Angiographic lesion characteristics can predict adverse outcomes after carotid artery stenting. J Vasc Surg 47(1):81–87. doi:10.1016/j.jvs.2007.09.047
Hofmann R, Niessner A, Kypta A, Steinwender C, Kammler J, Kerschner K (2006) Risk score for peri-interventional complications of carotid artery stenting. Stroke 37(10):2557–2561. doi:10.1161/01.STR.0000240688.81918.32
Naggara O, Touze E, Beyssen B, Trinquart L, Chatellier G, Meder JF (2011) Anatomical and technical factors associated with stroke or death during carotid angioplasty and stenting: results from the endarterectomy versus angioplasty in patients with symptomatic severe carotid stenosis (EVA-3S) trial and systematic review. Stroke 42(2):380–388. doi:10.1161/STROKEAHA.110.588772
Vatan MB, Acar BA, Aksoy M, Can Y, Varım C, Agac MT (2016) Predictors of periprocedural complications of carotid artery stenting—a multivariate analysis of a single-centre experience. Vasa Zeitschrift Für Gefässkrankheiten Journal for Vascular Diseases 45(5):1–7. doi:10.1024/0301-1526/a000550
Touze E, Trinquart L, Chatellier G, Mas JL (2009) Systematic review of the perioperative risks of stroke or death after carotid angioplasty and stenting. Stroke 40(12):e683–e693. doi:10.1161/STROKEAHA.109.562041
Alberti KG, Zimmet P, Shaw J (2005) The metabolic syndrome—a new worldwide definition. Lancet 366(9491):1059–1062. doi:10.1016/S0140-6736(05)67402-8
North American Symptomatic Carotid Endarterectomy Trial (1991) Methods, patient characteristics, and progress. Stroke 22(6):711–720
Goldstein JA, Demetriou D, Grines CL, Pica M, Shoukfeh M, O’Neill WW (2000) Multiple complex coronary plaques in patients with acute myocardial infarction. N Engl J Med 343:915–922. doi:10.1056/NEJM200009283431303
Wang Y, Zhao X, Liu L, Soo YO, Pu Y, Pan Y (2014) Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in china: the Chinese Intracranial Atherosclerosis (CICAS) Study. Stroke 45(3):663. doi:10.1161/STROKEAHA.113.003508
Kastrup A, Groschel K, Schulz JB, Nagele T, Ernemann U (2005) Clinical predictors of transient ischemic attack, stroke, or death within 30 days of carotid angioplasty and stenting. Stroke 36(4):787–791. doi:10.1161/01.STR.0000157585.01437.1f
Pigna G, Napoli A, Zaccagna F, Marincola BC, Monticolo R, Catalano C (2011) The relationship between metabolic syndrome, its components, and the whole-body atherosclerotic disease burden as measured by computed tomography angiography. Atherosclerosis 215(2):417–420. doi:10.1016/j.atherosclerosis.2010.12.038
Ren D, Wang J, Hua L, Li Y, Li Z (2017) Red blood cell distribution width and carotid intima-media thickness in patients with metabolic syndrome. BMC Cardiovasc Disord 17(1):44. doi:10.1186/s12872-017-0481-x
Yao MF, He J, Sun X, Ji XL, Ding Y, Zhao YM (2016) Gender differences in risks of coronary heart disease and stroke in patients with type 2 diabetes mellitus and their association with metabolic syndrome in china. Int J Endocrinol 2016:1–7. doi:10.1155/2016/8483405
Protack CD, Bakken AM, Xu J, Saad WA, Lumsden AB, Davies MG (2009) Metabolic syndrome: a predictor of adverse outcomes after carotid revascularization. J Vasc Surg 49(5):1172–1180. doi:10.1016/j.jvs.2008.12.011
Lev-Ran A (2001) Human obesity: an evolutionary approach to understanding our bulging waistline. Diabetes Metab Res Rev 17:347–362
Barbara RC, Alina S, Tomasz W, Piotr R, Krzysztof G, Kornel B (2015) Low-grade risk of hypercoagulable state in patients suffering from diabetes mellitus type 2. Journal of Zhejiang University-SCIENCE B 16(9):788–795. doi:10.1631/jzus.B1500066
Tadokoro Y, Sakaguchi M, Yamagami H, Okazaki S, Furukado S, Matsumoto M (2014) Echogenicity of medium-to-large carotid plaques predicts future vascular events. Cerebrovasc Dis 38(5):354–361
Ostling G, Hedblad B, Berglund G, Goncalves I (2007) Increased echolucency of carotid plaques in patients with type 2 diabetes. Stroke 38(7):2074–2078. doi:10.1159/000365651
Mutharasan RK, Thaxton CS, Berry J, Daviglus ML, Yuan C, Sun J (2017) Hdl efflux capacity, HDL particle size and high-risk carotid atherosclerosis in a cohort of asymptomatic older adults: the Chicago Healthy Aging Study. J Lipid Res 58(3):600–606. doi:10.1194/jlr.P069039
Newman GC, Bang H, Hussain SI, Toole JF (2007) Association of diabetes, homocysteine, and HDL with cognition and disability after stroke. Neurology 69(22):2054–2062. doi:10.1212/01.wnl.0000280457.29680.9c
Paavola T, Kuusisto S, Jauhiainen M, Kakko S, Kangaskontio T, MetsoJ (2017) Impaired hdl2-mediated cholesterol efflux is associated with metabolic syndrome in families with early onset coronary heart disease and low HDL-cholesterol level. PLoS One, 12(2): e0171993. DOI: 10.1371/journal.pone.0171993
Lee JS, Chang PY, Zhang Y, Kizer JR, Best LG, Howard BV (2017) Triglyceride and HDL-C dyslipidemia and risks of coronary heart disease and ischemic stroke by glycemic dysregulation status: the strong heart study. Diabetes Care 40(4):529–537. doi:10.2337/dc16-1958
Tsompanidi EM, Brinkmeier MS, Fotiadou EH, Giakoumi SM, Kypreos KE (2010) HDL biogenesis and functions: role of HDL quality and quantity in atherosclerosis. Atherosclerosis 208(1):3–9. doi:10.1016/j.atherosclerosis.2009.05.034
Siebenhofer A, Jeitler K, Berghold A, Waltering A, Hemkens LG, Semlitsch T (2011) Long-term effects of weight-reducing diets in hypertensive patients. Cochrane Database Syst Rev 9:CD008274. doi:10.1002/14651858.CD008274.pub2
Cordero A, Bertomeu-Martinez V, Mazon P, Martin-Raymondi D, Palma JL, Anguita M (2011) Short-term metabolic changes achieved by weight loss in hypertensive patients. Int J Cardiol 153(3):286–290. doi:10.1016/j.ijcard.2010.08.051
Theiss W, Hermanek P, Mathias K, Bruckmann H, Dembski J, Hoffmann FJ (2008) Predictors of death and stroke after carotid angioplasty and stenting: a subgroup analysis of the pro-CAS data. Stroke 39(8):2325–2330. doi:10.1161/STROKEAHA.108.514356
Kastrup A, Groschel K, Schnaudigel S, Nagele T, Schmidt F, Ernemann U (2008) Target lesion ulceration and arch calcification are associated with increased incidence of carotid stenting-associated ischemic lesions in octogenarians. J Vasc Surg 47(1):88–95. doi:10.1016/j.jvs.2007.09.045
Lam RC, Lin SC, DeRubertis B, Hynecek R, Kent KC, Faries PL (2007) The impact of increasing age on anatomic factors affecting carotid angioplasty and stenting. J Vasc Surg 45(5):875–880. doi:10.1016/j.jvs.2006.12.059
Usman AA, Tang GL, Eskandari MK (2009) Metaanalysis of procedural stroke and death among octogenarians: carotid stenting versus carotid endarterectomy. J Am Coll Surg 208(6):1124–1131. doi:10.1016/j.jamcollsurg.2009.02.043
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the Institutional Review Board of the Third Military Medical University, and all of the participants and their caregivers provided written informed consent.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Dong, S., Peng, Z., Tao, Y. et al. Metabolic syndrome is associated with increased risk of short-term post-procedural complications after carotid artery stenting. Neurol Sci 38, 1933–1939 (2017). https://doi.org/10.1007/s10072-017-3085-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-017-3085-4