Abstract
Objective
We aimed to investigate the muscle coordination differences between a control group and patients with mild and severe knee osteoarthritis (KOA) using muscle synergy analysis and determine whether muscle coordination was associated with symptoms of KOA.
Method
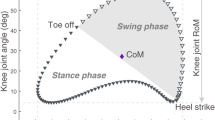
Fifty-three women with medial KOA and 19 control patients participated in the study. The gait analyses and muscle activity measurements of seven lower limb muscles were assessed using a motion capture system and electromyography. Gait speed and knee adduction moment impulse were calculated. The spatiotemporal components of muscle synergy were extracted using non-negative matrix factorization, and the dynamic motor control index during walking (walk-DMC) was computed. The number of muscle synergy and their spatiotemporal components were compared among the mild KOA, severe KOA, and control groups. Moreover, the association between KOA symptoms with walk-DMC and other gait parameters was evaluated using multi-linear regression analysis.
Results
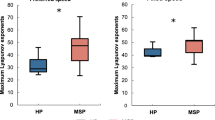
The number of muscle synergies was lower in mild and severe KOA compared with those in the control group. In synergy 1, the weightings of biceps femoris and gluteus medius in severe KOA were higher than that in the control group. In synergy 3, the weightings of higher tibial anterior and lower gastrocnemius lateralis were confirmed in the mild KOA group. Regression analysis showed that the walk-DMC was independently associated with knee-related symptoms of KOA after adjusting for the covariates.
Conclusions
Muscle coordination was altered in patients with KOA. The correlation between muscle coordination and KOA may be attributed to the knee-related symptoms.
Key points • Patients with knee osteoarthritis (OA) experienced a deterioration in muscle coordination when walking. • Loss of muscle coordination was associated with severe knee-related symptoms in knee OA. • Considering muscle coordination as a knee OA symptom-related factor may provide improved treatment. |



Similar content being viewed by others
Data availability
Data will be made available on request.
Code availability
Not applicable.
References
Saxby DJ, Lloyd DG (2017) Osteoarthritis year in review 2016: mechanics. Osteoarthr Cartil 25(2):190–198. https://doi.org/10.1016/j.joca.2016.09.023
Boekesteijn RJ, van Gerven J, Geurts ACH, Smulders K (2022) Objective gait assessment in individuals with knee osteoarthritis using inertial sensors: a systematic review and meta-analysis. Gait Posture 98:109–120. https://doi.org/10.1016/j.gaitpost.2022.09.002
Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S (2002) Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis 61(7):617–622
Kito N, Shinkoda K, Yamasaki T, Kanemura N, Anan M, Okanishi N, Ozawa J, Moriyama H (2010) Contribution of knee adduction moment impulse to pain and disability in Japanese women with medial knee osteoarthritis. Clin Biomech (Bristol, Avon) 25(9):914–919. https://doi.org/10.1016/j.clinbiomech.2010.06.008
Chang AH, Moisio KC, Chmiel JS, Eckstein F, Guermazi A, Prasad PV, Zhang Y, Almagor O, Belisle L, Hayes K, Sharma L (2015) External knee adduction and flexion moments during gait and medial tibiofemoral disease progression in knee osteoarthritis. Osteoarthr Cartil 23(7):1099–1106. https://doi.org/10.1016/j.joca.2015.02.005
Lewek MD, Rudolph KS, Snyder-Mackler L (2004) Control of frontal plane knee laxity during gait in patients with medial compartment knee osteoarthritis. Osteoarthr Cartil 12(9):745–751. https://doi.org/10.1016/j.joca.2004.05.005
Schmitt LC, Rudolph KS (2007) Influences on knee movement strategies during walking in persons with medial knee osteoarthritis. Arthritis Rheum 57(6):1018–1026. https://doi.org/10.1002/art.22889
Zeni JA, Rudolph K, Higginson JS (2010) Alterations in quadriceps and hamstrings coordination in persons with medial compartment knee osteoarthritis. J Electromyogr Kinesiol 20(1):148–154. https://doi.org/10.1016/j.jelekin.2008.12.003
Hubley-Kozey CL, Hill NA, Rutherford DJ, Dunbar MJ, Stanish WD (2009) Co-activation differences in lower limb muscles between asymptomatic controls and those with varying degrees of knee osteoarthritis during walking. Clin Biomech (Bristol, Avon) 24(5):407–414. https://doi.org/10.1016/j.clinbiomech.2009.02.005
Hodges PW, van den Hoorn W, Wrigley TV, Hinman RS, Bowles KA, Cicuttini F, Wang Y, Bennell K (2016) Increased duration of co-contraction of medial knee muscles is associated with greater progression of knee osteoarthritis. Man Ther 21:151–158. https://doi.org/10.1016/j.math.2015.07.004
Heiden TL, Lloyd DG, Ackland TR (2009) Knee joint kinematics, kinetics and muscle co-contraction in knee osteoarthritis patient gait. Clin Biomech (Bristol, Avon) 24(10):833–841. https://doi.org/10.1016/j.clinbiomech.2009.08.005
Ivanenko YP, Poppele RE, Lacquaniti F (2004) Five basic muscle activation patterns account for muscle activity during human locomotion. J Physiol 556(Pt 1):267–282. https://doi.org/10.1113/jphysiol.2003.057174
d'Avella A, Bizzi E (2005) Shared and specific muscle synergies in natural motor behaviors. Proc Natl Acad Sci U S A 102(8):3076–3081. https://doi.org/10.1073/pnas.0500199102
Torres-Oviedo G, Ting LH (2007) Muscle synergies characterizing human postural responses. J Neurophysiol 98(4):2144–2156. https://doi.org/10.1152/jn.01360.2006
Tang L, Li F, Cao S, Zhang X, Wu D, Chen X (2015) Muscle synergy analysis in children with cerebral palsy. J Neural Eng 12(4):046017. https://doi.org/10.1088/1741-2560/12/4/046017
Cheung VC, Turolla A, Agostini M, Silvoni S, Bennis C, Kasi P, Paganoni S, Bonato P, Bizzi E (2012) Muscle synergy patterns as physiological markers of motor cortical damage. Proc Natl Acad Sci U S A 109(36):14652–14656. https://doi.org/10.1073/pnas.1212056109
Kubota K, Yokoyama M, Onitsuka K, Kanemura N (2023) The investigation of an analysis method for co-activation of knee osteoarthritis utilizing normalization of peak dynamic method. Gait Posture 101:48–54. https://doi.org/10.1016/j.gaitpost.2023.01.021
Kubota K, Hanawa H, Yokoyama M, Kita S, Hirata K, Fujino T, Kokubun T, Ishibashi T, Kanemura N (2021) Usefulness of muscle synergy analysis in individuals with knee osteoarthritis during gait. IEEE Trans Neural Syst Rehabil Eng 29:239–248. https://doi.org/10.1109/TNSRE.2020.3043831
Diamond LE, Van den Hoorn W, Bennell KL, Wrigley TV, Hinman RS, O'Donnell J, Hodges PW (2017) Coordination of deep hip muscle activity is altered in symptomatic femoroacetabular impingement. J Orthop Res 35(7):1494–1504. https://doi.org/10.1002/jor.23391
Astephen Wilson JL, Deluzio KJ, Dunbar MJ, Caldwell GE, Hubley-Kozey CL (2011) The association between knee joint biomechanics and neuromuscular control and moderate knee osteoarthritis radiographic and pain severity. Osteoarthr Cartil 19(2):186–193. https://doi.org/10.1016/j.joca.2010.10.020
Preece SJ, Jones RK, Brown CA, Cacciatore TW, Jones AK (2016) Reductions in co-contraction following neuromuscular re-education in people with knee osteoarthritis. BMC Musculoskelet Disord 17(1):372. https://doi.org/10.1186/s12891-016-1209-2
Fingleton C, Smart K, Moloney N, Fullen BM, Doody C (2015) Pain sensitization in people with knee osteoarthritis: a systematic review and meta-analysis. Osteoarthr Cartil 23(7):1043–1056. https://doi.org/10.1016/j.joca.2015.02.163
Liao X, Mao C, Wang Y, Zhang Q, Cao D, Seminowicz DA, Zhang M, Yang X (2018) Brain gray matter alterations in Chinese patients with chronic knee osteoarthritis pain based on voxel-based morphometry. Medicine 97(12):e0145. https://doi.org/10.1097/MD.0000000000010145
Yamagata M, Taniguchi M, Tateuchi H, Kobayashi M, Ichihashi N (2021) The effects of knee pain on knee contact force and external knee adduction moment in patients with knee osteoarthritis. J Biomech 123:110538. https://doi.org/10.1016/j.jbiomech.2021.110538
Lee DD, Seung HS (1999) Learning the parts of objects by non-negative matrix factorization. Nature 401(6755):788–791. https://doi.org/10.1038/44565
Schwartz MH, Rozumalski A, Steele KM (2016) Dynamic motor control is associated with treatment outcomes for children with cerebral palsy. Dev Med Child Neurol 58(11):1139–1145. https://doi.org/10.1111/dmcn.13126
Steele KM, Rozumalski A, Schwartz MH (2015) Muscle synergies and complexity of neuromuscular control during gait in cerebral palsy. Dev Med Child Neurol 57(12):1176–1182. https://doi.org/10.1111/dmcn.12826
Taniguchi N, Matsuda S, Kawaguchi T, Tabara Y, Ikezoe T, Tsuboyama T, Ichihashi N, Nakayama T, Matsuda F, Ito H (2015) The KSS 2011 reflects symptoms, physical activities, and radiographic grades in a Japanese population. Clin Orthop Relat Res 473(1):70–75. https://doi.org/10.1007/s11999-014-3650-6
Pataky TC, Robinson MA, Vanrenterghem J (2013) Vector field statistical analysis of kinematic and force trajectories. J Biomech 46(14):2394–2401. https://doi.org/10.1016/j.jbiomech.2013.07.031
Lacquaniti F, Ivanenko YP, Zago M (2012) Patterned control of human locomotion. J Physiol 590(10):2189–2199. https://doi.org/10.1113/jphysiol.2011.215137
Clark DJ, Ting LH, Zajac FE, Neptune RR, Kautz SA (2010) Merging of healthy motor modules predicts reduced locomotor performance and muscle coordination complexity post-stroke. J Neurophysiol 103(2):844–857. https://doi.org/10.1152/jn.00825.2009
Falaki A, Huang X, Lewis MM, Latash ML (2017) Motor equivalence and structure of variance: multi-muscle postural synergies in Parkinson’s disease. Exp Brain Res 235(7):2243–2258. https://doi.org/10.1007/s00221-017-4971-y
Hashiguchi Y, Ohata K, Osako S, Kitatani R, Aga Y, Masaki M, Yamada S (2018) Number of synergies is dependent on spasticity and gait kinetics in children with cerebral palsy. Pediatr Phys Ther 30(1):34–38. https://doi.org/10.1097/Pep.0000000000000460
Allison K, Salomoni SE, Bennell KL, Wrigley TV, Hug F, Vicenzino B, Grimaldi A, Hodges PW (2018) Hip abductor muscle activity during walking in individuals with gluteal tendinopathy. Scand J Med Sci Sports 28(2):686–695. https://doi.org/10.1111/sms.12942
Liikavainio T, Bragge T, Hakkarainen M, Karjalainen PA, Arokoski JP (2010) Gait and muscle activation changes in men with knee osteoarthritis. Knee 17(1):69–76. https://doi.org/10.1016/j.knee.2009.05.003
Rutherford DJ, Hubley-Kozey CL, Stanish WD (2013) Changes in knee joint muscle activation patterns during walking associated with increased structural severity in knee osteoarthritis. J Electromyogr Kinesiol 23(3):704–711. https://doi.org/10.1016/j.jelekin.2013.01.003
Yamagata M, Tateuchi H, Asayama A, Ichihashi N (2022) Influence of lower-limb muscle inactivation on medial and lateral knee contact forces during walking. Med Eng Phys 108:103889. https://doi.org/10.1016/j.medengphy.2022.103889
Mundermann A, Dyrby CO, Andriacchi TP (2005) Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum 52(9):2835–2844. https://doi.org/10.1002/art.21262
Chang A, Hayes K, Dunlop D, Song J, Hurwitz D, Cahue S, Sharma L (2005) Hip abduction moment and protection against medial tibiofemoral osteoarthritis progression. Arthritis Rheum 52(11):3515–3519. https://doi.org/10.1002/art.21406
Sutherland DH (2001) The evolution of clinical gait analysis part l: kinesiological EMG. Gait Posture 14(1):61–70. https://doi.org/10.1016/s0966-6362(01)00100-x
van den Hoorn W, Hodges PW, van Dieen JH, Hug F (2015) Effect of acute noxious stimulation to the leg or back on muscle synergies during walking. J Neurophysiol 113(1):244–254. https://doi.org/10.1152/jn.00557.2014
Gizzi L, Muceli S, Petzke F, Falla D (2015) Experimental muscle pain impairs the synergistic modular control of neck muscles. PloS One 10(9):e0137844. https://doi.org/10.1371/journal.pone.0137844
Iwabuchi SJ, Xing Y, Cottam WJ, Drabek MM, Tadjibaev A, Fernandes GS, Petersen KK, Arendt-Nielsen L, Graven-Nielsen T, Valdes AM, Zhang W, Doherty M, Walsh D, Auer DP (2020) Brain perfusion patterns are altered in chronic knee pain: a spatial covariance analysis of arterial spin labelling MRI. Pain 161(6):1255–1263. https://doi.org/10.1097/j.pain.0000000000001829
Hall M, Bennell KL, Wrigley TV, Metcalf BR, Campbell PK, Kasza J, Paterson KL, Hunter DJ, Hinman RS (2017) The knee adduction moment and knee osteoarthritis symptoms: relationships according to radiographic disease severity. Osteoarthr Cartil 25(1):34–41. https://doi.org/10.1016/j.joca.2016.08.014
Acknowledgements
The authors would like to thank all staff and patients for their participation in this study. We would like to thank Editage (www.editage.jp) for English language editing.
Funding
This study was supported by the JSPS KAKENHI Grant-in-Aid for Scientific Research (18H03164 and 20K19376).
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the conception and design of the study, revising it critically for important intellectual content, and final approval of the version to be submitted. The specific contributions of each author are as follows. (1) Analysis and interpretation of data: MT, JU, MoY, and NI. (2) Article drafting: MT, JU, MoY, and NI.
Corresponding author
Ethics declarations
Ethics approval
All study procedures were approved by the Ethics Committee of the Kyoto University Graduate School of Medicine (R3014) and were conducted in accordance with the principles of the Declaration of Helsinki.
Consent to participate and consent for publication
Written informed consent for participation and the use of data was obtained from all participants.
Disclosures
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Taniguchi, M., Umehara, J., Yamagata, M. et al. Understanding muscle coordination during gait based on muscle synergy and its association with symptoms in patients with knee osteoarthritis. Clin Rheumatol 43, 743–752 (2024). https://doi.org/10.1007/s10067-023-06852-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-023-06852-w