Abstract
Objective
To assess the frequency of uveitis in patients with psoriatic arthritis (PsA) in the era of biologics and to identify risk factors associated with uveitis.
Methods
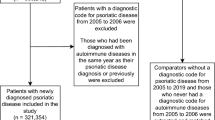
A retrospective matched cohort study was conducted within the database of a large healthcare provider. Newly diagnosed 6147 adult PsA patients between 2005 and 2020 were matched by the index date of PsA diagnosis, age, sex, and ethnicity to 23,999 randomly selected controls. This cohort was used to examine the association between PsA and uveitis. An additional analysis was conducted within the PsA group to identify uveitis risk factors, using two analytic approaches: a retrospective cohort study and a nested case-control study.
Results
Uveitis was diagnosed in 107 patients in the PsA group (1.7%) vs 187 (0.8%) patients in the control group (adjusted HR, 2.38, 95% CI 1.80–3.15, p<0.005) and was similar when the analysis was confined to patients without past uveitis. Uveitis was diagnosed more in females (2.1% vs 1.3%, HR 1.61, 95% CI 1.09–2.40, p<0.05), and was acute in all cases. Anterior uveitis was documented in 41.1% of the cases, 64.5% unilateral, and 9.3% bilateral. In the PsA group, using nested case control approach, only past uveitis [adjusted OR 136.4 (95% CI 27.38–679.88), p<0.005] and treatment with etanercept [adjusted OR 2.57 (95% CI 1.45–4.57), p=0.001] were independently associated with uveitis. Only one PsA patient with uveitis (out of 107) required systemic oral treatment with prednisone, while the rest of the patients were treated with topical glucocorticosteroids only.
Conclusion
PsA is associated with increased risk of uveitis. Past uveitis and treatment with etanercept were associated with higher risk of uveitis.
Key Points • Psoriatic arthritis (PsA) is a major risk factor for uveitis with hazard ratio of 2.38 compared to healthy individuals without PsA. • Among PsA patients, the past event of uveitis and treatment with etanercept are risk factors for uveitis. • Uveitis in patients treated with biologics for their PsA requires topical therapy only in most of the cases. |
Similar content being viewed by others
References
Perez-Chada LM, Merola JF (2020) Comorbidities associated with psoriatic arthritis: Review and update. Clin Immunol 214:108397
Haddad A, Zisman D (2017) Comorbidities in patients with psoriatic arthritis. Rambam Maimonides Med J 8(1)
Pittam B, Gupta S, Harrison NL, Robertson S, Hughes DM, Zhao SS (2020) Prevalence of extra-articular manifestations in psoriatic arthritis: a systematic review and meta-analysis. Rheumatology 59(9):2199–2206
Singh JA, Guyatt G, Ogdie A, Gladman DD, Deal C, Deodhar A et al (2019) Special article: 2018 american college of rheumatology/national psoriasis foundation guideline for the treatment of psoriatic arthritis. Arthritis Care Res (Hoboken) 71(1):2–29
Abbouda A, Abicca I, Fabiani C, Scappatura N, Peña-García P, Scrivo R et al (2017) Psoriasis and psoriatic arthritis-related uveitis: different ophthalmological manifestations and ocular inflammation features. Semin Ophthalmol 32(6):715–720
Feld J, Ye JY, Chandran V, Inman RD, Haroon N, Cook R et al (2020) Is axial psoriatic arthritis distinct from ankylosing spondylitis with and without concomitant psoriasis? Rheumatology 59(6):1340–1346
Marotte H, Cimaz R (2014) Etanercept - TNF receptor and IgG1 Fc fusion protein: is it different from other TNF blockers? Expert Opin Biol Ther 14(5):569–572
Leclercq M, Desbois A-C, Domont F, Maalouf G, Touhami S, Cacoub P et al (2020) Biotherapies in uveitis. J Clin Med 9(11)
Rennert G, Peterburg Y (2001) Prevalence of selected chronic diseases in Israel. Isr Med Assoc J 3(6):404–408
Eder L, Cohen AD, Feldhamer I, Greenberg-Dotan S, Batat E, Zisman D (2018) The epidemiology of psoriatic arthritis in Israel - a population-based study. Arthritis Res Ther 20(1):3
Lambert JR, Wright V (1976) Eye inflammation in psoriatic arthritis. Ann Rheum Dis 35(354)
Li C-R, Chen L, Wang L-F, Yan B, Liang Y-L, Luo J (2020) Association between uveitis and psoriatic disease: a systematic review and meta-analysis based on the evidence from cohort studies. Int J Ophthalmol 13(4):650–659
Chaiyabutr C, Ungprasert P, Silpa-Archa N, Wongpraparut C, Chularojanamontri L (2020) Psoriasis and risk of uveitis: a systematic review and meta-analysis. Biomed Res Int 2020:9308341
Lam M, Steen J, Lu JD, Vender R (2020) The Incidence and Prevalence of Uveitis in Psoriasis: A Systematic Review and Meta-Analysis. J Cutan Med Surg 24(6):601–607
Charlton R, Green A, Shaddick G, Snowball J, Nightingale A, Tillett W et al (2018) Risk of uveitis and inflammatory bowel disease in people with psoriatic arthritis: a population-based cohort study. Ann Rheum Dis 77(2):277–280
Egeberg A, Khalid U, Gislason GH, Mallbris L, Skov L, Hansen PR (2015) Association of psoriatic disease with uveitis: a Danish nationwide cohort study. JAMA Dermatol 151(11):1200–1205
Bengtsson K, Forsblad-d’Elia H, Deminger A, Klingberg E, Dehlin M, Exarchou S et al (2021) Incidence of extra-articular manifestations in ankylosing spondylitis, psoriatic arthritis and undifferentiated spondyloarthritis: results from a national register-based cohort study. Rheumatology 60(6):2725–2734
Zeboulon N, Dougados M, Gossec L (2008) Prevalence and characteristics of uveitis in the spondyloarthropathies: a systematic literature review. Ann Rheum Dis 67(7):955–959
Chi C-C, Tung T-H, Wang J, Lin Y-S, Chen Y-F, Hsu T-K et al (2017) Risk of uveitis among people with psoriasis: a nationwide cohort study. JAMA Ophthalmol 135(5):415–422
Aguado Casanova V, Ventas B, Arroyo Palomo J, Huelin Alcubierre FJ, Villalobos Sánchez L, Revenga Martínez M et al (2023) Epidemiology and clinical characteristics of psoriatic arthritis-related uveitis in Madrid, Spain. Int Ophthalmol 43(3):771–777
De Vicente DA, Sanchez-Bilbao L, Calvo-Río V, Martínez-López D, Herrero-Morant A, Galíndez-Agirregoikoa E et al (2023) Uveitis in psoriatic arthritis: study of 406 patients in a single university center and literature review. RMD Open 9(1)
Kakkassery V, Mergler S, Pleyer U (2010) Anti-TNF-alpha treatment: a possible promoter in endogenous uveitis? observational report on six patients: occurrence of uveitis following etanercept treatment. Curr Eye Res 35(8):751–756
Wendling D, Paccou J, Berthelot J-M, Flipo R-M, Guillaume-Czitrom S, Prati C et al (2011) New onset of uveitis during anti-tumor necrosis factor treatment for rheumatic diseases. Semin Arthritis Rheum 41(3):503–510
Biggioggero M, Crotti C, Becciolini A, Miserocchi E, Favalli EG (2018) The management of acute anterior uveitis complicating spondyloarthritis: present and future. Biomed Res Int 2018:9460187
Acknowledgements
This research paper pays tribute to the memory of Mrs. I. Lavi whom we would like to acknowledge and appreciate her invaluable contributions to this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was performed in accordance with the principles of the Declaration of Helsinki and was approved by the research ethics committee (institutional review board) of Carmel Medical Center (CMC-0014-14).
Consent to participate
Requirement for individual patient consent forms was waived due to the retrospective, observational nature of the study.
Consent for publication
All authors reviewed the manuscript, helped in editing it, and approved its publication.
Disclosures
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hijazi, ., Gazitt, T., Haddad, A. et al. The risk factors for uveitis among psoriatic arthritis patients: a population-based cohort study. Clin Rheumatol 43, 1053–1061 (2024). https://doi.org/10.1007/s10067-023-06834-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-023-06834-y