Abstract
Introduction/objectives
Delayed diagnosis of axial spondyloarthritis (axSpA) is well documented; little is known about the diagnostic journey and impediments for US patients with nonradiographic axSpA (nr-axSpA). It is hypothesized that impediments are varied and exist at both the healthcare provider (HCP) and patient levels. This study aims to understand patient experiences and contributors to delayed nr-axSpA diagnosis in the USA.
Method
Interviews of adults with rheumatologist-diagnosed nr-axSpA, recruited through Spondylitis Association of America outreach and patient panels, and of rheumatologists, explored the diagnostic journey and diagnostic barriers. Emerging themes were further explored in an online patient survey. A multiple logistic regression analysis evaluated the main outcome variable, factors affecting time to nr-axSpA diagnosis.
Results
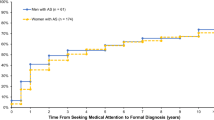
Interviews were conducted with 25 patients and 16 rheumatologists. Survey responses from 186 eligible patients revealed median time from symptom onset to diagnosis of nr-axSpA was 3.25 years. Delayed diagnosis was significantly more likely for women and people in rural areas. Most patients consulted ≥4 different types of HCPs before a rheumatologist and ≥2 rheumatologists before diagnosis. Impediments to timely diagnosis included insidious chronic pain; episodic symptom patterns attributed to activity; symptoms other than chronic lumbosacral back pain requiring medical consultation; and unfamiliarity with and misperceptions about nr-axSpA among HCPs, radiologists, and rheumatologists.
Conclusions
Delayed nr-axSpA diagnosis is common and reflects HCP knowledge gaps and frequent patient presentation with dominant nonaxial symptoms. Targeted HCP education, research into early disease patterns, and interventions sensitive to the broader spectrum of nr-axSpA manifestations are needed to improve timely diagnosis.
Key Points • Patients with nr-axSpA often see multiple types of HCPs, and multiple rheumatologists, before receiving a diagnosis. • Both patients and HCPs are unfamiliar with nr-axSpA and its symptoms, lacking understanding that nr-axSpA can occur in young people, females, and those presenting with normal x-rays. • Disease recognition by nonrheumatology HCPs is key for early referral. • Education on cardinal features, epidemiology, burden, and benefits of timely nr-axSpA diagnosis is warranted for HCPs who commonly manage back pain. |



Similar content being viewed by others
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Rudwaleit M, van der Heijde D, Landewe R et al (2009) The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis 68(6):777–783. https://doi.org/10.1136/ard.2009.108233
Lopez-Medina C, Ramiro S, van der Heijde D, Sieper J, Dougados M, Molto A (2019) Characteristics and burden of disease in patients with radiographic and non-radiographic axial spondyloarthritis: a comparison by systematic literature review and meta-analysis. RMD Open 5(2):e001108. https://doi.org/10.1136/rmdopen-2019-001108
López-Medina C, Molto A, Claudepierre P, Dougados M (2020) Clinical manifestations, disease activity and disease burden of radiographic versus non-radiographic axial spondyloarthritis over 5 years of follow-up in the DESIR cohort. Ann Rheum Dis 79(2):209–216. https://doi.org/10.1136/annrheumdis-2019-216218
Mease PJ, Heijde DV, Karki C et al (2018) Characterization of patients with ankylosing spondylitis and nonradiographic axial spondyloarthritis in the US-based Corrona registry. Arthritis Care Res (Hoboken) 70(11):1661–1670. https://doi.org/10.1002/acr.23534
Reveille JD, Witter JP, Weisman MH (2012) Prevalence of axial spondylarthritis in the United States: estimates from a cross-sectional survey. Arthritis Care Res (Hoboken) 64(6):905–910. https://doi.org/10.1002/acr.21621
Curtis JR, Harrold LR, Asgari MM et al (2016) Diagnostic prevalence of ankylosing spondylitis using computerized health care data, 1996 to 2009: underrecognition in a US health care setting. Perm J 20(4):15–151. https://doi.org/10.7812/TPP/15-151
Deodhar A, Mease PJ, Reveille JD et al (2016) Frequency of axial spondyloarthritis diagnosis among patients seen by US rheumatologists for evaluation of chronic back pain. Arthritis Rheumatol 68(7):1669–1676. https://doi.org/10.1002/art.39612
Yi E, Ahuja A, Rajput T, George AT, Park Y (2020) Clinical, economic, and humanistic burden associated with delayed diagnosis of axial spondyloarthritis: a systematic review. Rheumatol Ther 7(1):65–87. https://doi.org/10.1007/s40744-020-00194-8
Barnett R, Ingram T, Sengupta R (2020) Axial spondyloarthritis 10 years on: still looking for the lost tribe. Rheumatology (Oxford) 59(Suppl4):iv25–iv37. https://doi.org/10.1093/rheumatology/keaa472
Danve A, Deodhar A (2019) Axial spondyloarthritis in the USA: diagnostic challenges and missed opportunities. Clin Rheumatol 38(3):625–634. https://doi.org/10.1007/s10067-018-4397-3
Rusman T, van Vollenhoven RF, van der Horst-Bruinsma IE (2018) Gender differences in axial spondyloarthritis: women are not so lucky. Curr Rheumatol Rep 20(6):35. https://doi.org/10.1007/s11926-018-0744-2
Danve A, Deodhar A (2022) Treatment of axial spondyloarthritis: an update. Nat Rev Rheumatol 18(4):205–216. https://doi.org/10.1038/s41584-022-00761-z
Martindale J, Goodacre L (2014) The journey to diagnosis in AS/axial SpA: the impact of delay. Musculoskeletal Care 12(4):221–231. https://doi.org/10.1002/msc.1080
Deodhar A, Mittal M, Reilly P et al (2016) Ankylosing spondylitis diagnosis in US patients with back pain: identifying providers involved and factors associated with rheumatology referral delay. Clin Rheumatol 35(7):1769–1776. https://doi.org/10.1007/s10067-016-3231-z
Masson Behar V, Dougados M, Etcheto A et al (2017) Diagnostic delay in axial spondyloarthritis: a cross-sectional study of 432 patients. Joint Bone Spine 84(4):467–471. https://doi.org/10.1016/j.jbspin.2016.06.005
Redeker I, Callhoff J, Hoffmann F et al (2019) Determinants of diagnostic delay in axial spondyloarthritis: an analysis based on linked claims and patient-reported survey data. Rheumatology (Oxford) 58(9):1634–1638. https://doi.org/10.1093/rheumatology/kez090
Garrido-Cumbrera M, Poddubnyy D, Gossec L et al (2019) The European map of axial spondyloarthritis: capturing the patient perspective-an analysis of 2846 patients across 13 countries. Curr Rheumatol Rep 21(5):19. https://doi.org/10.1007/s11926-019-0819-8
Ogdie A, Benjamin Nowell W, Reynolds R et al (2019) Real-world patient experience on the path to diagnosis of ankylosing spondylitis. Rheumatol Ther 6(2):255–267. https://doi.org/10.1007/s40744-019-0153-7
Jovani V, Blasco-Blasco M, Pascual E, Ruiz-Cantero MT (2018) Challenges to conquer from the gender perspective in medicine: the case of spondyloarthritis. PloS One 13(10):e0205751. https://doi.org/10.1371/journal.pone.0205751
Sykes MP, Doll H, Sengupta R, Gaffney K (2015) Delay to diagnosis in axial spondyloarthritis: are we improving in the UK? Rheumatology (Oxford) 54(12):2283–2284. https://doi.org/10.1093/rheumatology/kev288
Rudwaleit M, Landewe R, van der Heijde D et al (2009) The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part I): classification of paper patients by expert opinion including uncertainty appraisal. Ann Rheum Dis 68(6):770–776. https://doi.org/10.1136/ard.2009.108217
Zhao SS, Pittam B, Harrison NL, Ahmed AE, Goodson NJ, Hughes DM (2021) Diagnostic delay in axial spondyloarthritis: a systematic review and meta-analysis. Rheumatology (Oxford) 60(4):1620–1628. https://doi.org/10.1093/rheumatology/keaa807
Bennett AN, Marzo-Ortega H, Kaur-Papadakis D, Rehman A, BRITSpA (2017) The use of magnetic resonance imaging in axial spondyloarthritis: time to bridge the gap between radiologists and rheumatologists. J Rheumatol 44(6):780–785. https://doi.org/10.3899/jrheum.161337
Weber U, Jurik AG, Zejden A et al (2018) Frequency and anatomic distribution of magnetic resonance imaging features in the sacroiliac joints of young athletes: exploring “background noise” toward a data-driven definition of sacroiliitis in early spondyloarthritis. Arthritis Rheumatol 70(5):736–745. https://doi.org/10.1002/art.40429
de Winter J, de Hooge M, van de Sande M et al (2018) Magnetic resonance imaging of the sacroiliac joints indicating sacroiliitis according to the Assessment of SpondyloArthritis international Society definition in healthy individuals, runners, and women with postpartum back pain. Arthritis Rheumatol 70(7):1042–1048. https://doi.org/10.1002/art.40475
de Bruin F, Treyvaud MO, Feydy A et al (2018) Prevalence of degenerative changes and overlap with spondyloarthritis-associated lesions in the spine of patients from the DESIR cohort. RMD Open 4(1):e000657. https://doi.org/10.1136/rmdopen-2018-000657
de Bruin F, ter Horst S, Bloem HL et al (2016) Prevalence of degenerative changes of the spine on magnetic resonance images and radiographs in patients aged 16-45 years with chronic back pain of short duration in the Spondyloarthritis Caught Early (SPACE) cohort. Rheumatology (Oxford) 55(1):56–65. https://doi.org/10.1093/rheumatology/kev283
Jamal M, Korver AM, Kuijper M et al (2020) The IMPACT study: a clustered randomized controlled trial to assess the effect of a referral algorithm for axial spondyloarthritis. PloS One 15(1):e0227025. https://doi.org/10.1371/journal.pone.0227025
Baraliakos X, Tsiami S, Redeker I et al (2020) Early recognition of patients with axial spondyloarthritis-evaluation of referral strategies in primary care. Rheumatology (Oxford) 59(12):3845–3852. https://doi.org/10.1093/rheumatology/keaa212
Renson T, Carron P, De Craemer AS et al (2021) Axial involvement in patients with early peripheral spondyloarthritis: a prospective MRI study of sacroiliac joints and spine. Ann Rheum Dis 80(1):103–108. https://doi.org/10.1136/annrheumdis-2020-218480
de Winter JJ, Paramarta JE, de Jong HM, van de Sande MG, Baeten DL (2019) Peripheral disease contributes significantly to the level of disease activity in axial spondyloarthritis. RMD Open 5(1):e000802. https://doi.org/10.1136/rmdopen-2018-000802
Swinnen TW, Vlaeyen JWS, Dankaerts W, Westhovens R, de Vlam K (2018) Activity limitations in patients with axial spondyloarthritis: a role for fear of movement and (re)injury beliefs. J Rheumatol 45(3):357–366. https://doi.org/10.3899/jrheum.170318
Masi AT (2014) Might axial myofascial properties and biomechanical mechanisms be relevant to ankylosing spondylitis and axial spondyloarthritis? Arthritis Res Ther 16(2):107. https://doi.org/10.1186/ar4532
Jacques P, McGonagle D (2014) The role of mechanical stress in the pathogenesis of spondyloarthritis and how to combat it. Best Pract Res Clin Rheumatol 28(5):703–710. https://doi.org/10.1016/j.berh.2014.10.009
Ramiro S, Landewé R, van Tubergen A et al (2015) Lifestyle factors may modify the effect of disease activity on radiographic progression in patients with ankylosing spondylitis: a longitudinal analysis. RMD Open 1(1):e000153. https://doi.org/10.1136/rmdopen-2015-000153
Ward MM, Reveille JD, Learch TJ, Davis JC Jr, Weisman MH (2008) Occupational physical activities and long-term functional and radiographic outcomes in patients with ankylosing spondylitis. Arthritis Rheum 59(6):822–832. https://doi.org/10.1002/art.23704
Jovani V, Blasco-Blasco M, Ruiz-Cantero MT, Pascual E (2017) Understanding how the diagnostic delay of spondyloarthritis differs between women and men: a systematic review and metaanalysis. J Rheumatol 44(2):174–183. https://doi.org/10.3899/jrheum.160825
Swinnen TW, Westhovens R, Dankaerts W, de Vlam K (2018) Widespread pain in axial spondyloarthritis: clinical importance and gender differences. Arthritis Res Ther 20(1):156. https://doi.org/10.1186/s13075-018-1626-8
Templeton KJ (2020) Sex and gender issues in pain management. J Bone Joint Surg Am 102(Suppl 1):32–35. https://doi.org/10.2106/JBJS.20.00237
Lindstrom Egholm C, Krogh NS, Pincus T et al (2015) Discordance of global assessments by patient and physician is higher in female than in male patients regardless of the physician’s sex: data on patients with rheumatoid arthritis, axial spondyloarthritis, and psoriatic arthritis from the DANBIO registry. J Rheumatol 42(10):1781–1785. https://doi.org/10.3899/jrheum.150007
Samulowitz A, Gremyr I, Eriksson E, Hensing G (2018) “Brave men” and “emotional women”: a theory-guided literature review on gender bias in health care and gendered norms towards patients with chronic pain. Pain Res Manag 2018:6358624. https://doi.org/10.1155/2018/6358624
Lapane KL, Khan S, Shridharmurthy D et al (2020) Primary care physician perspectives on barriers to diagnosing axial spondyloarthritis: a qualitative study. BMC Fam Pract 21(1):204. https://doi.org/10.1186/s12875-020-01274-y
American College of Rheumatology (2016) 2015 workforce study of rheumatology specialists in the United States. https://www.rheumatology.org/portals/0/files/ACR-Workforce-Study-2015.pdf.
Acknowledgements
The authors would like to thank Dr Jill Foster and the Institute for Medical and Nursing Education editorial team for support in developing this manuscript. We would also like to acknowledge Erin Schulz, John Thomas, and the LaunchBox team for their help in conducting and analyzing interviews and the survey and in reporting initial findings.
Funding
UCB provided funding to the Spondylitis Association of America in support of this study.
Author information
Authors and Affiliations
Contributions
SK was integral in developing the study design, analyzing and interpreting the study datasets, and liaison with the statistician on dataset analysis. RH was integral in developing the study design, recruitment and enrollment of patients into the study, and analyzing and interpreting study datasets. DC provided statistical analysis on all datasets and verified data accuracy. AD was integral in development of the study design and analyzing and interpreting study datasets. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
All study participants provided their consent for participation. Consent forms are available upon request.
Competing interests
SK declares that she has no competing interests. RH declares that he has the following competing interests: Consulting/advisory board: Novartis, GSK; Stock: AbbVie, Amgen, Bristol Myers Squibb, GSK, Johnson & Johnson, Lilly, Merck, Novartis, Pfizer, Teva, UCB, Viatris. DC declares that he has no competing interests. AD declares that he has the following competing interests: Consulting/advisory boards: AbbVie, Amgen, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, GSK, Eli Lilly, Janssen, Novartis, Pfizer, UCB; Research grants: AbbVie, Lilly, Novartis, Pfizer, UCB.
Disclaimer
UCB did not participate in the survey design, interpretation of results, or manuscript development.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors acknowledge an overlap with a previously published article by the same authors: https://www.researchsquare.com/article/rs-876767/v1.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kiwalkar, S., Howard, R., Choi, D. et al. A mixed methods study to uncover impediments to accurate diagnosis of nonradiographic axial spondyloarthritis in the USA. Clin Rheumatol 42, 2811–2822 (2023). https://doi.org/10.1007/s10067-023-06671-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-023-06671-z