Abstract
Objectives
The aim of this study was to evaluate the relationship between the presence of neuropathic pain (NeP), disease activity scores and biologic drug–switching decisions in the subjects with axial spondyloarthritis (axSpA) receiving biologic treatment.
Methods
PainDETECT Questionnaire was used to evaluate the presence of NeP in the patients with axSpA aged ≥18 years who had been receiving biologic treatment for at least 6 months. The relationships between disease activity scores, inflammatory markers, life quality index, biologic drug–switching decisions and the presence of NeP were analyzed.
Results
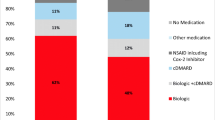
A total number of 175 patients with axSpA [ankylosing spondylitis (AS) (n:150) and non-radiographic axSpA (nr-axSpA) (n:25)] were enrolled in the study. NeP was detected in 41.7% of the patients and it was more common in females than in males (p:0.009). PainDETECT scores were positively correlated with disease activity scores, but they were not correlated with inflammatory marker levels. NeP was found to be significantly more common in whom the biologics had been switched 3 or more times (p:0.007). PainDETECT scores were higher and NeP was more prevalent (p:0.028) in the patients for whom drug-switching decisions had been made due to primary or secondary unresponsiveness.
Conclusion
NeP is more common than estimated in the patients with axSpA and current disease activity scores are insufficient to make a distinction between NeP and inflammatory pain. NeP is a confounding factor in the evaluation of treatment response to biologic agents. In the subjects with AS and nr-axSpA with primary or secondary treatment unresponsiveness, the presence of NeP must be considered before biologic drug–switching decisions.
Key Points • Neuropathic pain (NeP) is common in subjects with AxSpA treated with multiple biologic agents. • Current disease activity scores for AxSpA are insufficient to make a differentiation between NeP and inflammatory pain. • NeP is a confounding factor in the evaluation of treatment response to biologic agents. • Patients with AxSpA should be re-evaluated in terms of the presence of neuropathic pain before making biologic drug-switching decisions. |


Similar content being viewed by others
References
Sieper J, Braun J, Dougados M, Baeten D (2015) Axial spondyloarthritis. Nat Rev Dis Primers 1:15013. https://doi.org/10.1038/nrdp.2015.13
Gok K, Cengiz G, Erol K, Ozgocmen S (2018) Neuropathic pain component in axial spondyloarthritis and the ınfluence on disease burden. J Clin Rheumatol 24(6):324–327. https://doi.org/10.1097/RHU.0000000000000711
Kim TW, Son SM, Lee JS (2020) Neuropathic pain in ankylosing spondylitis: a meta-analysis. Neuropathischer Schmerz bei ankylosierender Spondylitis – eine Metaanalyse. Z Rheumatol 79(1):95–102. https://doi.org/10.1007/s00393-019-0654-3
Wu Q, Inman RD, Davis KD (2013) Neuropathic pain in ankylosing spondylitis: a psychophysics and brain imaging study. Arthritis Rheum 65(6):1494–1503. https://doi.org/10.1002/art.37920
Mease PJ (2017) Fibromyalgia, a missed comorbidity in spondyloarthritis: prevalence and impact on assessment and treatment. Curr Opin Rheumatol 29(4):304–310. https://doi.org/10.1097/BOR.0000000000000388
Macfarlane GJ et al (2017) Co-occurrence and characteristics of patients with axial spondyloarthritis who meet criteria for fibromyalgia: results from a UK National Register. Arthritis Rheumatol 69(11):2144–2150. https://doi.org/10.1002/art.40185
Gau SY, Lee YH, Tsou HK, Huang JY, Chen X, Ye Z, Wei JC (2021) Patients with ankylosing spondylitis are associated with high risk of fibromyalgia: a nationwide population-based cohort study. Front Med (Lausanne) 8:618594. https://doi.org/10.3389/fmed.2021.618594
Freynhagen R, Baron R, Gockel U, Tölle TR (2006) painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin 22(10):1911–1920. https://doi.org/10.1185/030079906X132488
Rudwaleit M, van der Heijde D, Landewé R et al (2009) The development of assessment of spondyloarthritis international society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis 68(6):777–783. https://doi.org/10.1136/ard.2009.108233
Braun J, Sieper J (2007) Ankylosing spondylitis. Lancet 369(9570):1379–1390. https://doi.org/10.1016/S0140-6736(07)60635-7
McCormack HM, Horne DJ, Sheather S (1988) Clinical applications of visual analogue scales: a critical review. Psychol Med 18(4):1007–1019. https://doi.org/10.1017/s0033291700009934
Alkan H et al (2013) Turkish version of the painDETECT questionnaire in the assessment of neuropathic pain: a validity and reliability study. Pain med (Malden, Mass.) 14(12):1933–1943. https://doi.org/10.1111/pme.12222
Garrett S et al (1994) A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol 21(12):2286–2291
Haywood KL, Garratt AM, Dawes PT (2005) Patient-assessed health in ankylosing spondylitis: a structured review. Rheumatology (Oxford) 44(5):577–586. https://doi.org/10.1093/rheumatology/keh549
Wolfe F et al (2010) The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken) 62(5):600–610. https://doi.org/10.1002/acr.20140
Choi JH, Lee SH, Kim HR, Lee KA (2018) Association of neuropathic-like pain characteristics with clinical and radiographic features in patients with ankylosing spondylitis. Clin Rheumatol 37(11):3077–3086. https://doi.org/10.1007/s10067-018-4125-z
Atar E, Askin A (2020) Somatosensory dysfunction related neuropathic pain component affects disease activity, functional status and quality of life in ankylosing spondylitis. Int J Rheum Dis 23(12):1656–1663. https://doi.org/10.1111/1756-185X.13993
Geler-Külcü D, Batıbay S, Öztürk G, Mesci N (2018) The association of neuropathic pain and disease activity, functional level, and quality of life in patients with ankylosing spondylitis: a cross-sectional study. Turk J Med Sci 48(2):257–265. https://doi.org/10.3906/sag-1707-147
Koca T, Göğebakan H, Çetin G (2019) Should central sensitization and neuropathic pain be considered in disease activity and treatment decision in axial ankylosing spondilitis? Cukurova Med J 44(4):1–10. https://doi.org/10.17826/cumj.503652
Garip Y, Eser F, Kılıçarslan A, Bodur H (2015) Prevalence of neuropathic pain in rheumatic disorders: association with disease activity, functional status and quality of life. Arch Rheumatol 30(3):231–237. https://doi.org/10.5606/ArchRheumatol.2015.5295
Bidad K, Gracey E, Hemington KS, Mapplebeck JCS, Davis KD, Inman RD (2017) Pain in ankylosing spondylitis: a neuro-immune collaboration. Nat Rev Rheumatol 13(7):410–420. https://doi.org/10.1038/nrrheum.2017.92
Sieper J, Poddubnyy D (2017) Axial spondyloarthritis. Lancet 390(10089):73–84. https://doi.org/10.1016/S0140-6736(16)31591-4
Hess A et al (2011) Blockade of TNF-α rapidly inhibits pain responses in the central nervous system. Proc Natl Acad Sci U S A 108(9):3731–3736. https://doi.org/10.1073/pnas.1011774108
Danve A, Deodhar A (2017) Treat to target in axial spondyloarthritis: what are the ıssues? Curr Rheumatol Rep 19(5):22. https://doi.org/10.1007/s11926-017-0648-6
Ramiro S (2022) Update of the ASAS/EULAR recommendations on the management of axial spondyloarthritis. In: Oral presentation in the EULAR recommendations session. EULAR Congress, Copenhagen, Denmark
Son SM, Kim DS, Lee JS (2022) Fibromyalgia in axial spondyloarthritis: a meta-analysis. J Clin Rheumatol 28(1):e222–e227. https://doi.org/10.1097/RHU.0000000000001612
van der Horst-Bruinsma IE, Zack DJ, Szumski A, Koenig AS (2013) Female patients with ankylosing spondylitis: analysis of the impact of gender across treatment studies. Ann Rheum Dis 72(7):1221–1224. https://doi.org/10.1136/annrheumdis-2012-202431
Lee W et al (2007) Are there gender differences in severity of ankylosing spondylitis? Results from the PSOAS cohort. Ann Rheum Dis 66(5):633–638. https://doi.org/10.1136/ard.2006.060293
Ji Y, He Y, Nian X, Sun E, Li L (2019) Inflammatory or neuropathic pain: characteristics and their relationships with disease activity and functional status in axial spondyloarthritis patients. Pain Med 20(5):882–888. https://doi.org/10.1093/pm/pny138
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Öğüt, T.S., Erbasan, F., Terzioğlu, M.E. et al. Neuropathic pain in axial spondyloarthropathy is underdiagnosed and a confounding factor in biologic drug–switching decision: a cross-sectional study. Clin Rheumatol 42, 1275–1284 (2023). https://doi.org/10.1007/s10067-023-06531-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-023-06531-w