Abstract
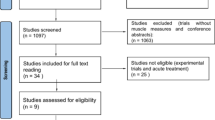
To perform a systematic review with meta-analysis to verify muscle strength, muscle mass, and physical function of patients with systemic lupus erythematosus (SLE) and compare then with healthy individuals and patients with rheumatoid arthritis (RA). A systematic review with meta-analysis of observational studies published in English up to 2022 was performed using MEDLINE (via PubMed) and other relevant sources. Search strategies were based on pre-defined keywords and medical subject headings. The methodological quality of the studies was assessed using the Newcastle–Ottawa Scale. Mean difference (MD) or standardized mean difference (SMD) and 95% confidence intervals (CI) were combined using a random-effects model. Sensitivity analyses were performed when necessary. The significance level was set at p < 0.05. The systematic review included 19 studies and the meta-analysis included 11 studies. SLE patients appear to have less muscle strength assessed by handgrip than healthy controls (SLE = 21.74 kg; healthy controls = 29.34 kg; p < 0.05). SLE patients seem to have greater strength than patients with RA, but this difference was not statistically significant (RA = 17.24 kg; p = 0.210). However, in the sensitivity analysis, SLE group without deforming arthropathy showed higher muscle strength than the RA (p = 0.0001). SLE patients with deforming arthropathy have lower muscle strength compared to SLE patients without deforming arthropathy (p < 0.01). Muscle mass was similar in SLE patients compared to the RA group and healthy controls (p > 0.05). However, RA patients have a higher BMI than the two groups (p < 0.05). Patients with SLE have regular physical function. Muscle strength is affected in SLE patients. SLE patients with deforming arthropathy have less muscle strength than patients without deforming arthropathies.





Similar content being viewed by others
References
Rao AP, Raghuram J (2016) Systemic lupus erythematosus. Indian J Pract Pediatr 18:313–319. https://doi.org/10.7326/aitc202006020
di Battista M (2018) One year in review 2018: systemic lupus erythematosus. Clin Exp Rheumatol 36(5):763–777
Fortuna G, Brennan MT (2013) Systemic lupus erythematosus. Epidemiology, pathophysiology, manifestations, and management. Dent Clin North Am 57:631–655
Malcus Johnsson P, Sandqvist G, Bengtsson A, Nived O (2008) Hand function and performance of daily activities in systemic lupus erythematosus. Arthritis Rheum 59:1432–1438. https://doi.org/10.1002/art.24108
Bağlan Yentür S, Tuna Z, Mete O et al (2018) Hand functions in systemic lupus erythematosus: a comparative study with rheumatoid arthritis patients and healthy subjects. Turk J Med Sci 48:840–844. https://doi.org/10.3906/sag-1803-183
Balsamo S, da Mota LMH, de Carvalho JF et al (2013) Low dynamic muscle strength and its associations with fatigue, functional performance, and quality of life in premenopausal patients with systemic lupus erythematosus and low disease activity: a case-control study. BMC Musculoskelet Disord 14:263. https://doi.org/10.1186/1471-2474-14-263
Stockton KA, Kandiah DA, Paratz JD, Bennell KL (2012) Fatigue, muscle strength and vitamin D status in women with systemic lupus erythematosus compared with healthy controls. Lupus 21:271–278. https://doi.org/10.1177/0961203311425530
Mahran S, Fathi N, Seddek M, Goma SH (2021) Physical ability and quality of life in rheumatoid arthritis and systemic lupus erythematosus: a brief comparison. Aktuelle Rheumatol 46:88–96. https://doi.org/10.1055/a-1224-3540
Loureiro Galvão V, Santos FVD, D, Santiago MB, (2020) The influence of hand dominance on the degree of deformities in patients with systemic lupus erythematosus and Jaccoud arthropathy. J Clin Rheumatol 26:S205–S207. https://doi.org/10.1097/RHU.0000000000001392
Lhakum P, Kasitanon N, Sivasomboon C et al (2016) Deforming arthropathy in Thai patients with systemic lupus erythematosus. J Clin Rheumatol 22:1–7. https://doi.org/10.1097/RHU.0000000000000333
Rydholm M, Wikström I, Hagel S et al (2019) The relation between upper extremity joint involvement and grip force in early rheumatoid arthritis: a retrospective study. Rheumatol Int 39:2031–2041. https://doi.org/10.1007/s00296-019-04438-x
Li Z, Shang J, Zeng S et al (2019) Altered body composition and increased visceral adipose tissue in premenopausal and late postmenopausal patients with SLE. Clin Rheumatol 38:3117–3127. https://doi.org/10.1007/s10067-019-04701-3
Liyanage A, Lekamwasam S, Dissanayake SP, Munidasa D (2013) Factors that determine body composition of female systemic lupus erythematosus (SLE) patients in Sri Lanka: a comparative study using dual-energy x-ray absorptiometry. Lupus 22:972–976. https://doi.org/10.1177/0961203313496338
Seguro LPC, Paupitz JA, Caparbo VF et al (2018) Increased visceral adipose tissue and altered adiposity distribution in premenopausal lupus patients: correlation with cardiovascular risk factors. Lupus 27:1001–1006. https://doi.org/10.1177/0961203318758504
Santos MJ, Vinagre F, Canas da Silva J et al (2011) Body composition phenotypes in systemic lupus erythematosus and rheumatoid arthritis: a comparative study of Caucasian female patients. Clin Exp Rheumatol 29:470–476
Dey M, Bukhari M (2018) Predictors of fracture risk in patients with systemic lupus erythematosus. Lupus 27:1547–1551. https://doi.org/10.1177/0961203318768886
Elera-Fitzcarrald C, Ugarte-Gil MF, Gamboa-Cárdenas R, v, et al (2017) Prolactin levels are associated with a pro-inflammatory body mass distribution among women with systemic lupus erythematosus. Lupus 26:808–814. https://doi.org/10.1177/0961203316678673
Andrews JS, Trupin L, Schmajuk G et al (2015) Muscle strength, muscle mass, and physical disability in women with systemic lupus erythematosus. Arthritis Care Res (Hoboken) 67:120–127. https://doi.org/10.1002/acr.22399
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31
Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al (2010) Sarcopenia: European consensus on definition and diagnosis. Age Ageing 39:412–423. https://doi.org/10.1093/ageing/afq034
Doherty TJ (2003) Invited review: aging and sarcopenia. J Appl Physiol 95:1717–1727
Morley JE, Anker SD, von Haehling S (2014) Prevalence, incidence, and clinical impact of sarcopenia: facts, numbers, and epidemiology—update 2014. J Cachexia Sarcopenia Muscle 5:253–259
Brown JC, Harhay MO, Harhay MN (2016) Sarcopenia and mortality among a population-based sample of community-dwelling older adults. J Cachexia Sarcopenia Muscle 290–298. https://doi.org/10.1002/jcsm.12073
Alves de Araujo Silva T, Frisoli Junior A, Medeiros Pinheiro M, Lúcia Szejnfeld V (2006) Sarcopenia Associada ao Envelhecimento: Aspectos Etiológicos e Opções Terapêuticas Sarcopenia and Aging: Etiological Aspects and Therapeutic Options. Rev Bras Reumatol 46(6).
Moher D, Shamseer L, Clarke M et al (2016) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Rev Espanola de Nutr Hum y Diet 20:148–160. https://doi.org/10.1186/2046-4053-4-1
Mattos CT, de Ruellas AC, O, (2015) Systematic review and meta-analysis: what are the implications in the clinical practice? Dental Press J Orthod 20:17–19. https://doi.org/10.1590/2176-9451.20.1.017-019.ebo
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
dos Santos LP, do Espírito Santo RC, Ramis TR, et al (2021) The effects of resistance training with blood flow restriction on muscle strength, muscle hypertrophy and functionality in patients with osteoarthritis and rheumatoid arthritis: a systematic review with meta-analysis. PLoS One 16(11):e0259574. https://doi.org/10.1371/journal.pone.0259574
Higgins JPT, Thomas J, Chandler J et al (2021) Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). In: Cochrane handbook for systematic reviews of interventions version 6.2, Cochran
Modesti PA, Reboldi G, Cappuccio FP et al (2016) Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS One 11(1):e0147601. https://doi.org/10.1371/journal.pone.0147601
Toledano E, Candelas G, Rosales Z et al (2012) A meta-analysis of mortality in rheumatic diseases. Reumatol Clín (English Edition) 8:334–341. https://doi.org/10.1016/j.reumae.2012.05.002
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557
Sumantri S, Rengganis I, Laksmi PW et al (2021) The impact of low muscle function on health-related quality of life in Indonesian women with systemic lupus erythematosus. Lupus 30:680–686. https://doi.org/10.1177/0961203320988595
Sola-Rodríguez S, Gavilán-Carrera B, Vargas-Hitos JA et al (2019) Physical fitness and body composition in women with systemic lupus erythematosus. Medicina (Kaunas) 55. https://doi.org/10.3390/medicina55020057
Andrews JS, Trupin L, Schmajuk G et al (2015) Muscle strength and changes in physical function in women with systemic lupus erythematosus. Arthritis Care Res (Hoboken) 67:1070–1077. https://doi.org/10.1002/acr.22560
Keramiotou K, Anagnostou C, Konstantonis G et al (2021) Impaired hand function and performance in activities of daily living in systemic lupus erythematosus, even in patients achieving lupus low disease activity state (LLDAS). Rheumatol Adv Pract 5. https://doi.org/10.1093/rap/rkab029
Plantinga L, Tift BD, Dunlop-Thomas C et al (2018) Geriatric assessment of physical and cognitive functioning in a diverse cohort of systemic lupus erythematosus patients: a pilot study. Arthritis Care Res (Hoboken) 70:1469–1477. https://doi.org/10.1002/acr.23507
Santiago MB, Galvão V (2008) Jaccoudarthropathy in systemic lupus erythematosus analysis of clinical characteristics and review of the literature. https://doi.org/10.1097/MD.0b013e318632d18
Piga M, Gabba A, Congia M et al (2016) Predictors of musculoskeletal flares and Jaccoud’s arthropathy in patients with systemic lupus erythematosus: a 5-year prospective study. Semin Arthritis Rheum 46:217–224. https://doi.org/10.1016/j.semarthrit.2016.04.005
Roberts HC, Denison HJ, Martin HJ et al (2011) A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing 40:423–429
Amaral JF, Mancini M, Novo Júnior JM (2012) Comparison of three hand dynamometers in relation to the accuracy and precision of the measurements. Braz J Phys Ther 16:216–224. https://doi.org/10.1590/S1413-35552012000300007
Keramiotou K, Anagnostou C, Kataxaki E et al (2020) The impact of upper limb exercise on function, daily activities and quality of life in systemic lupus erythematosus: a pilot randomised controlled trial. RMD Open 6. https://doi.org/10.1136/rmdopen-2019-001141
Baker JF, Mostoufi-Moab S, Long J et al (2018) Intramuscular fat accumulation and associations with body composition, strength, and physical functioning in patients with rheumatoid arthritis. Arthritis Care Res (Hoboken) 70:1727–1734. https://doi.org/10.1002/acr.23550
Mok CC, To CH, Ma KM (2008) Changes in body composition after glucocorticoid therapy in patients with systemic lupus erythematosus. Lupus 17:1018–1022. https://doi.org/10.1177/0961203308093552
Guralnik JM, Simonsick EM, Ferrucci L et al (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49(2):M85–94. https://doi.org/10.1093/geronj/49.2.m85
Acknowledgements
We thank Vânia Naomi Hirakata, statistician at the Biostatistics Service of the Hospital de Clínicas de Porto Alegre (HCPA), for her scientific support in our systematic review with meta-analysis. Moreover, we thank the Fundo de Incentivo à Pesquisa e Eventos (FIPE) of the Hospital de Clínicas de Porto Alegre and research support fund of the Society of Rheumatology of Rio Grande do Sul for the financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary material 1
(DOCX 23 kb)
Supplementary material 2
(DOCX 16 kb)

Supplementary material 3
Forest plot of the handgrip strength test comparing studies with patients with systemic lupus erythematosus (SLE) with or without deforming arthropathies; MRAW, raw mean; ES, estimated; I^2, heterogeneity between studies; CI; Confidence Interval. (PNG 552 kb)

Supplementary material 4
Forest plot of the handgrip strength test excluding two studies with female and male SLE (systemic lupus erythematosus) patients in the same sample. Including the other two studies from the control group and from the group of patients with rheumatoid arthritis (RA). MRAW, raw mean; ES, estimated; I^2, heterogeneity between studies; CI; Confidence Interval. (TIF 1380 kb) (PNG 600 kb)
Supplementary material 5
(DOCX 90 kb)

Supplementary material 6
Forest plot comparing different study designs that include the handgrip test from our meta-analysis. MRAW, raw mean; ES, estimated; I^2, heterogeneity between studies; CI; Confidence Interval. (PNG 493 kb)
Supplementary material 7
(DOCX 208 kb)
Supplementary material 8
(DOCX 73 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pena, É., dos Santos, L.P., do Espírito Santo, R.C. et al. Systemic lupus erythematosus: a systematic review with meta-analysis on muscle strength, muscle mass, and physical function. Clin Rheumatol 42, 1237–1248 (2023). https://doi.org/10.1007/s10067-023-06516-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-023-06516-9