Abstract
Objectives
Localized scleroderma (LSc) is a disease characterized by the excessive deposition of collagen and thereby thickening of the dermis. In recent years, studies reported that LSc demonstrated compromised skin barrier related to the progression of the disease. However, human studies examining epidermis in scleroderma are still sparse and lack systematic research. This study aims to investigate the structural and functional changes in the LSc epidermis and further explore the underlying mechanisms, providing a new angle to treat LSc in the clinic.
Methods
A total of 136 skin sites, including lesion and non-lesion control, from 27 LSc patients were analyzed. Ultrasonic testing, trans-epidermal water loss (TEWL), and epidermal hydration were assessed to investigate the structural and functional alternations; correlations between these parameters were analyzed. To explore the underlying mechanism, skin-fibrosis mouse model and cellular model by bleomycin (BLM) were deployed.
Results
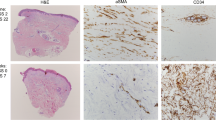
The epidermal thickness was markedly increased, with a significant decline of hydration (dryness) in the LSc lesion skin. Epidermal hydration presented a negative correlation with the thickness. TEWL was not altered. The mouse model validated these morphological changes in the epidermis and indicated that interleukin-6 (IL-6) was significantly elevated. Furthermore, cellular study demonstrated that increased phosphorylation of p38 in keratinocyte promoted the secretion of IL-6, stimulating cell proliferation.
Conclusion
This study characterized the epidermal alterations in LSc patients, suggesting that keratinocyte-derived abnormal IL-6 secretion can lead to the thickening of the epidermis, promoting dryness. The topical application of moisturizer may largely relieve dryness and related pruritus, thus improve the quality of life in LSc patients.
Key Points • Epidermal thickness was increased in LSc lesion skin with declined hydration level. • Skin fibrosis mouse model validated the epidermal alteration in LSc patient. • p38-dependent IL-6 overexpression in keratinocyte result in epidermal thickening. |





Similar content being viewed by others
References
Distler O, Cozzio A (2016) Systemic sclerosis and localized scleroderma–current concepts and novel targets for therapy. Semin Immunopathol 38:87–95. https://doi.org/10.1007/s00281-015-0551-z
Laxer RM, Zulian F (2006) Localized scleroderma. Curr Opin Rheumatol 18:606–613. https://doi.org/10.1097/01.bor.0000245727.40630.c3
Kreuter A, Hyun J, Skrygan M, Sommer A, Bastian A, Altmeyer P et al (2006) Ultraviolet al-induced downregulation of human beta-defensins and interleukin-6 and interleukin-8 correlates with clinical improvement in localized scleroderma. Br J Dermatol 155:600–607. https://doi.org/10.1111/j.1365-2133.2006.07391.x
Alten R, Maleitzke T (2013) Tocilizumab: a novel humanized anti-interleukin 6 (IL-6) receptor antibody for the treatment of patients with non-RA systemic, inflammatory rheumatic diseases. Ann Med 45:357–363. https://doi.org/10.3109/07853890.2013.771986
Careta MF, Romiti R (2015) Localized scleroderma: clinical spectrum and therapeutic update. An Bras Dermatol 90:62–73. https://doi.org/10.1590/abd1806-4841.20152890
Kim MW, Park JT, Kim JH, Koh SJ, Yoon HS, Cho S et al (2017) Periostin in mature stage localized scleroderma. Ann Dermatol 29:268–275. https://doi.org/10.5021/ad.2017.29.3.268
Torok KS, Li SC, Jacobe HM, Taber SF, Stevens AM, Zulian F, et al (2019) Immunopathogenesis of pediatric localized scleroderma. Front Immunol 10.https://doi.org/10.3389/fimmu.2019.00908
Wolska-Gawron K, Bartosinska J, Krasowska D (2020) MicroRNA in localized scleroderma: a review of literature. Arch Dermatol Res 312:317–324. https://doi.org/10.1007/s00403-019-01991-0
Ihn H, Sato S, Fujimoto M, Kikuchi K, Takehara K (1995) Demonstration of interleukin-2, interleukin-4 and interleukin-6 in sera from patients with localized scleroderma. Arch Dermatol Res 287:193–197. https://doi.org/10.1007/bf01262331
Klimas NK, Shedd AD, Bernstein IH, Jacobe H (2015) Health-related quality of life in morphoea. Br J Dermatol 172:1329–1337. https://doi.org/10.1111/bjd.13572
Minato H, Taki R, Miyachi Y, Utani A (2009) Symmetrical pigmented sclerosis enclosed by pruritic erythema: a new variant of morphoea? Br J Dermatol 161:703–706. https://doi.org/10.1111/j.1365-2133.2009.09360.x
Das S, Bernstein I, Jacobe H (2014) Correlates of self-reported quality of life in adults and children with morphea. J Am Acad Dermatol 70:904–910. https://doi.org/10.1016/j.jaad.2013.11.037
Ďurčanská V, Jedličková H, Vašků V (2016) Measurement of transepidermal water loss in localized scleroderma. Dermatol Ther 29:177–180. https://doi.org/10.1111/dth.12339
Nikitorowicz-Buniak J, Shiwen X, Denton CP, Abraham D, Stratton R (2014) Abnormally differentiating keratinocytes in the epidermis of systemic sclerosis patients show enhanced secretion of CCN2 and S100A9. J Invest Dermatol 134:2693–2702. https://doi.org/10.1038/jid.2014.253
Assassi S, Swindell WR, Wu M, Tan FD, Khanna D, Furst DE et al (2015) Dissecting the heterogeneity of skin gene expression patterns in systemic sclerosis. Arthritis Rheumatol (Hoboken, NJ) 67:3016–3026. https://doi.org/10.1002/art.39289
Takahashi T, Asano Y, Sugawara K, Yamashita T, Nakamura K, Saigusa R et al (2017) Epithelial Fli1 deficiency drives systemic autoimmunity and fibrosis: Possible roles in scleroderma. J Exp Med 214:1129–1151. https://doi.org/10.1084/jem.20160247
Peterson LS, Nelson AM, Su WP (1995) Classification of morphea (localized scleroderma). Mayo Clin Proc 70:1068–1076. https://doi.org/10.4065/70.11.1068
Moore TL, Lunt M, McManus B, Anderson ME, Herrick AL (2003) Seventeen-point dermal ultrasound scoring system–a reliable measure of skin thickness in patients with systemic sclerosis. Rheumatology (Oxford) 42:1559–1563. https://doi.org/10.1093/rheumatology/keg435
Nikam VN, Monteiro RC, Dandakeri S, Bhat RM (2019) Transepidermal water loss in psoriasis: a case-control study. Indian Dermatol Online J 10:267–271. https://doi.org/10.4103/idoj.IDOJ_180_18
Alanen E, Nuutinen J, Nicklén K, Lahtinen T, Mönkkönen J (2004) Measurement of hydration in the stratum corneum with the MoistureMeter and comparison with the Corneometer. Skin Res Technol 10:32–37. https://doi.org/10.1111/j.1600-0846.2004.00050.x
Makino K, Jinnin M, Hirano A, Yamane K, Eto M, Kusano T et al (2013) The downregulation of microRNA let-7a contributes to the excessive expression of type I collagen in systemic and localized scleroderma. J Immunol 190:3905–3915. https://doi.org/10.4049/jimmunol.1200822
Yan Q, Chen J, Li W, Bao C, Fu Q (2016) Targeting miR-155 to treat experimental scleroderma. Sci Rep 6:20314. https://doi.org/10.1038/srep20314
Bray NL, Pimentel H, Melsted P, Pachter L (2016) Near-optimal probabilistic RNA-seq quantification. Nat Biotechnol 34:525–527. https://doi.org/10.1038/nbt.3519
Tang CH, Chiu YC, Tan TW, Yang RS, Fu WM (2007) Adiponectin enhances IL-6 production in human synovial fibroblast via an AdipoR1 receptor, AMPK, p38, and NF-kappa B pathway. J Immunol 179:5483–5492. https://doi.org/10.4049/jimmunol.179.8.5483
Turner NA, Blythe NM (2019) Cardiac fibroblast p38 MAPK: a critical regulator of myocardial remodeling. J Cardiovasc Dev Dis 6.https://doi.org/10.3390/jcdd6030027
Morley SM, Gaylarde PM, Sarkany I (1985) Epidermal thickness in systemic sclerosis and morphoea. Clin Exp Dermatol 10:51–57. https://doi.org/10.1111/j.1365-2230.1985.tb02552.x
Rosenberger C, Solovan C, Rosenberger AD, Jinping L, Treudler R, Frei U et al (2007) Upregulation of hypoxia-inducible factors in normal and psoriatic skin. J Invest Dermatol 127:2445–2452. https://doi.org/10.1038/sj.jid.5700874
Toyama S, Sato S, Asano Y (2019) Localized scleroderma manifesting with skin lesions associated with mechanical stress. Eur J Dermatol: EJD 29:439–440. https://doi.org/10.1684/ejd.2019.3601
Romero LI, Pincus SH (1992) In situ localization of interleukin-6 in normal skin and atrophic cutaneous disease. Int Arch Allergy Immunol 99:44–49. https://doi.org/10.1159/000236334
Grossman RM, Krueger J, Yourish D, Granelli-Piperno A, Murphy DP, May LT et al (1989) Interleukin 6 is expressed in high levels in psoriatic skin and stimulates proliferation of cultured human keratinocytes. Proc Natl Acad Sci USA 86:6367–6371. https://doi.org/10.1073/pnas.86.16.6367
Johnson BZ, Stevenson AW, Prêle CM, Fear MW, Wood FM (2020) The role of IL-6 in skin fibrosis and cutaneous wound healing. Biomedicines 8. https://doi.org/10.3390/biomedicines8050101
Taniguchi K, Arima K, Masuoka M, Ohta S, Shiraishi H, Ontsuka K et al (2014) Periostin controls keratinocyte proliferation and differentiation by interacting with the paracrine IL-1alpha/IL-6 loop. J Invest Dermatol 134:1295–1304. https://doi.org/10.1038/jid.2013.500
Works MG, Yin F, Yin CC, Yiu Y, Shew K, Tran TT, et al (2014) Inhibition of TYK2 and JAK1 ameliorates imiquimod-induced psoriasis-like dermatitis by inhibiting IL-22 and the IL-23/IL-17 axis. J Immunol (Baltimore, Md : 1950) 193:3278–3287. https://doi.org/10.4049/jimmunol.1400205
Nagaoka T, Sato S, Hasegawa M, Ihn H, Takehara K (2000) Serum levels of soluble interleukin 6 receptor and soluble gp130 are elevated in patients with localized scleroderma. J Rheumatol 27:1917–1921
Denton CP, Ong VH, Xu S, Chen-Harris H, Modrusan Z, Lafyatis R et al (2018) Therapeutic interleukin-6 blockade reverses transforming growth factor-beta pathway activation in dermal fibroblasts: insights from the faSScinate clinical trial in systemic sclerosis. Ann Rheum Dis 77:1362–1371. https://doi.org/10.1136/annrheumdis-2018-213031
Khanna D, Lin CJF, Furst DE, Goldin J, Kim G, Kuwana M et al (2020) Tocilizumab in systemic sclerosis: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Respir Med 8:963–974. https://doi.org/10.1016/s2213-2600(20)30318-0
Brown M, O’Reilly S (2019) The immunopathogenesis of fibrosis in systemic sclerosis. Clin Exp Immunol 195:310–321. https://doi.org/10.1111/cei.13238
Heerfordt IM, Nissen CV, Poulsen T, Philipsen PA, Wulf HC (2016) Thickness of Actinic keratosis does not predict dysplasia severity or P53 expression. Sci Rep 6:33952. https://doi.org/10.1038/srep33952
Lichterfeld-Kottner A, Lahmann N, Blume-Peytavi U, Mueller-Werdan U, Kottner J (2018) Dry skin in home care: a representative prevalence study. J Tissue Viability 27:226–231. https://doi.org/10.1016/j.jtv.2018.07.001
Valdes-Rodriguez R, Mollanazar NK, Gonzalez-Muro J, Nattkemper L, Torres-Alvarez B, Lopez-Esqueda FJ et al (2015) Itch prevalence and characteristics in a Hispanic geriatric population: a comprehensive study using a standardized itch questionnaire. Acta Derm Venereol 95:417–421. https://doi.org/10.2340/00015555-1968
Therene C, Brenaut E, Sonbol H, Pasquier E, Saraux A, Devauchelle V et al (2017) Itch and systemic sclerosis: frequency, clinical characteristics and consequences. Br J Dermatol 176:1392–1393. https://doi.org/10.1111/bjd.14998
Misery L, Brenaut E, Le Garrec R, Abasq C, Genestet S, Marcorelles P et al (2014) Neuropathic pruritus. Nat Rev Neurol 10:408–416. https://doi.org/10.1038/nrneurol.2014.99
Frech T, Novak K, Revelo MP, Murtaugh M, Markewitz B, Hatton N et al (2011) Low-dose naltrexone for pruritus in systemic sclerosis. Int J Rheumatol 2011:804296. https://doi.org/10.1155/2011/804296
Funding
This work was supported by National Natural Science Foundation of China (81703097), China Postdoctoral Science Foundation (2017M621365), Shanghai Municipal Science and Technology Major Project (2017SHZDZX01), and CAMS Innovation Fund for Medical Sciences (2019-I2M-5–066).
Author information
Authors and Affiliations
Contributions
JX and XZ designed this study; XZ, QZ, XK, LZ, and RZ assessed skin morphology and physiology; XZ performed the animal and cellular experiments; LJ performed the RNA-seq analysis; YT supervised skin physiology assessment; JX and JW supervised the whole project; XZ and JX drafted the manuscript and substantially revised by JW; QL and WW for the intensive scientific discussion and suggestions.
Corresponding authors
Ethics declarations
Ethics approval
This research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. Study procedures were reviewed and approved by the Ethics Committee of School of Life Sciences, Fudan University (2017–619). Signed informed consent was obtained from all participants. Animal experiments were performed following the general guidelines, and the protocol was approved by the Animal Care and Use Committee of the School of Life sciences at Fudan University, China.
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhu, X., Jiang, L., Zhong, Q. et al. Abnormal expression of interleukin-6 is associated with epidermal alternations in localized scleroderma. Clin Rheumatol 41, 2179–2187 (2022). https://doi.org/10.1007/s10067-022-06127-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-022-06127-w