Abstract
Objectives
The social pain or invalidation denoting painful feeling following social conflicts or misunderstanding about illness legitimacy has been proposed as a salient disabling symptom besides physical pain or non-pain symptoms in fibromyalgia (FM). We sought to evaluate the effect of 1-month administration of duloxetine or pregabalin on the invalidation dimensions in FM patients with respect to the comparison of these two drugs on this issue.
Method
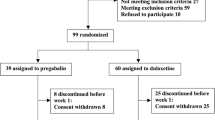
This open-label randomized clinical trial study was performed on FM patients whose diagnoses were confirmed by a rheumatologist based on the 2016 American College of Rheumatology (ACR). Primary outcome measure (Illness Invalidation Inventory (3*I)) and secondary outcome measures (Beck Depression Inventory-II (BDI-II), widespread pain index (WPI), and polysymptomatic distress scale (PSD)) were compared before and after treatment, using paired t test or Wilcoxon signed test.
Results
Of 81 eligible FM patients, 44 patients in the duloxetine arm and 27 patients in the pregabalin arm completed the study protocol. Overall, no significant improvement was seen in 3*I scores after treatment with either duloxetine or pregabalin, except in the lack of understanding of medical professionals which improved after treatment with pregabalin (2.43 ± 1.38 to 1.79 ± 0.94, p value: 0.01). There were no intragroup and intergroup differences in the effects of duloxetine and pregabalin on 3*I scores when adjusted with the cofounders. Both duloxetine and pregabalin improved WPI, BDI-II, and PSD scores significantly.
Conclusions
Short-term FM pharmacological treatment had no effect on social pain. This finding was regardless of drug type, improvement of physical pain, and depression.
Key Points • Social pain may behave as an independent but influential factor in FM rather than physical pain and depression. • Approved FM medications do not seem to change predictably the invalidation perception, which is a crucial factor in chronicity and maintaining of FM symptoms. • Dedicated approach to social pain seems necessary for the depiction of future successful therapeutic plan in FM. |

Similar content being viewed by others
Data availability
Data associated with the paper is available and will be provided if requested under reasonable conditions.
Code availability
Not applicable.
References
Williams ACC, Craig KD (2016) Updating the definition of pain. Pain 157(11):2420–2423. https://doi.org/10.1097/j.pain.0000000000000613
Ghavidel-Parsa B, Bidari A (2020) Two sides on the fibromyalgia coin: physical pain and social pain (invalidation). Clin Rheumatol. https://doi.org/10.1007/s10067-020-05304-z
Kool MB, van Middendorp H, Boeije HR, Geenen R (2009) Understanding the lack of understanding: invalidation from the perspective of the patient with fibromyalgia. Arthritis Rheum 61(12):1650–1656. https://doi.org/10.1002/art.24922
Villemure C, Bushnell CM (2002) Cognitive modulation of pain: how do attention and emotion influence pain processing? Pain 95(3):195–199. https://doi.org/10.1016/s0304-3959(02)00007-6
Macdonald G, Leary MR (2005) Why does social exclusion hurt? The relationship between social and physical pain. Psychol Bull 131(2):202–223. https://doi.org/10.1037/0033-2909.131.2.202
Peyron R, Laurent B, García-Larrea L (2000) Functional imaging of brain responses to pain A review and meta-analysis (2000). Neurophysiol Clin 30(5):263–288. https://doi.org/10.1016/s0987-7053(00)00227-6
Ghavidel-Parsa B, Bidari A, Tohidi S, Shenavar I, Kazemnezhad Leyli E, Hosseini K, Khosousi MJ (2021) Implication of invalidation concept in fibromyalgia diagnosis. Clin Rheumatol. https://doi.org/10.1007/s10067-020-05515-4
Eisenberger NI (2012) The neural bases of social pain: evidence for shared representations with physical pain. Psychosom Med 74(2):126–135. https://doi.org/10.1097/PSY.0b013e3182464dd1
Santiago MG, Marques A, Kool M, Geenen R, da Silva JAP (2017) Invalidation in patients with rheumatic diseases: clinical and psychological framework. J Rheumatol 44(4):512–518. https://doi.org/10.3899/jrheum.160559
Rook KS (1984) The negative side of social interaction: impact on psychological well-being. J Pers Soc Psychol 46(5):1097–1108. https://doi.org/10.1037//0022-3514.46.5.1097
Eisenberger NI, Jarcho JM, Lieberman MD, Naliboff BD (2006) An experimental study of shared sensitivity to physical pain and social rejection. Pain 126(1–3):132–138. https://doi.org/10.1016/j.pain.2006.06.024
Macfarlane GJ, Kronisch C, Dean LE, Atzeni F, Häuser W, Fluß E, Choy E, Kosek E, Amris K, Branco J, Dincer F, Leino-Arjas P, Longley K, McCarthy GM, Makri S, Perrot S, Sarzi-Puttini P, Taylor A, Jones GT (2017) EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis 76(2):318. https://doi.org/10.1136/annrheumdis-2016-209724
Bidari A, Moazen-Zadeh E, Ghavidel-Parsa B, Rahmani S, Hosseini S, Hassankhani A (2019) Comparing duloxetine and pregabalin for treatment of pain and depression in women with fibromyalgia: an open-label randomized clinical trial. Daru 27(1):149–158. https://doi.org/10.1007/s40199-019-00257-4
Kia S, Choy E (2017) Update on treatment guideline in fibromyalgia syndrome with focus on pharmacology. Biomedicines 5(2):20. https://doi.org/10.3390/biomedicines5020020
Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Häuser W, Katz RL, Mease PJ, Russell AS, Russell IJ, Walitt B (2016) 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum 46(3):319–329. https://doi.org/10.1016/j.semarthrit.2016.08.012
Kool MB, van Middendorp H, Lumley MA, Schenk Y, Jacobs JW, Bijlsma JW, Geenen R (2010) Lack of understanding in fibromyalgia and rheumatoid arthritis: the Illness Invalidation Inventory (3*I). Ann Rheum Dis 69(11):1990–1995. https://doi.org/10.1136/ard.2009.123224
Ghavidel-Parsa B, Amir Maafi A, Aarabi Y, Haghdoost A, Khojamli M, Montazeri A, Sanaei O, Bidari A (2015) Correlation of invalidation with symptom severity and health status in fibromyalgia. Rheumatology (Oxford) 54(3):482–486. https://doi.org/10.1093/rheumatology/keu355
García-Batista ZE, Guerra-Peña K, Cano-Vindel A, Herrera-Martínez SX, Medrano LA (2018) Validity and reliability of the Beck Depression Inventory (BDI-II) in general and hospital population of Dominican Republic. PLoS ONE 13(6):e0199750. https://doi.org/10.1371/journal.pone.0199750
Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Häuser W, Katz RS, Mease P, Russell AS, Russell IJ, Winfield JB (2011) Fibromyalgia criteria and severity scales for clinical and epidemiological studies: a modification of the ACR Preliminary Diagnostic Criteria for Fibromyalgia. J Rheumatol 38(6):1113–1122. https://doi.org/10.3899/jrheum.100594
Bidari A, Ghavidel-Parsa B, Amir Maafi A, Montazeri A, Ghalehbaghi B, Hassankhani A, Aarabi Y, Haghdoost A (2015) Validation of fibromyalgia survey questionnaire and polysymptomatic distress scale in a Persian population. Rheumatol Int 35(12):2013–2019. https://doi.org/10.1007/s00296-015-3340-z
Faul F, Erdfelder E, Buchner A, Lang A-G (2009) statstical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41:1149–1160. https://doi.org/10.3758/BRM.41.4.1149
Tatsuoka M (1993) Effect size. A handbook for data analysis in the behavioral sciences: methodological issues. Lawrence Erlbaum Associates Inc, Hillsdale, pp 461–479
Sancassiani F, Machado S, Ruggiero V, Cacace E, Carmassi C, Gesi C, Dell’Osso L, Carta MG (2017) The management of fibromyalgia from a psychosomatic perspective: an overview. Int Rev Psychiatry 29(5):473–488. https://doi.org/10.1080/09540261.2017.1320982
Cameron N, Kool M, Estévez-López F, López-Chicheri I, Geenen R (2018) The potential buffering role of self-efficacy and pain acceptance against invalidation in rheumatic diseases. Rheumatol Int 38(2):283–291. https://doi.org/10.1007/s00296-017-3859-2
Schmidt-Wilcke T, Diers M (2017) New insights into the pathophysiology and treatment of fibromyalgia. Biomedicines 5(2):22. https://doi.org/10.3390/biomedicines5020022
Huang ER, Jones KD, Bennett RM, Hall GCN, Lyons KS (2018) The role of spousal relationships in fibromyalgia patients’ quality of life. Psychol Health Med 23(8):987–995. https://doi.org/10.1080/13548506.2018.1444183
Bernardy K, Klose P, Busch AJ, Choy EH, Häuser W (2013) Cognitive behavioural therapies for fibromyalgia. Cochrane Database Syst Rev 2013(9):Cd009796
Scheidt CE, Waller E, Endorf K, Schmidt S, König R, Zeeck A, Joos A, Lacour M (2013) Is brief psychodynamic psychotherapy in primary fibromyalgia syndrome with concurrent depression an effective treatment? A randomized controlled trial. Gen Hosp Psychiatry 35(2):160–167. https://doi.org/10.1016/j.genhosppsych.2012.10.013
Diers M (2019) Neuroimaging the pain network — implications for treatment. Best Pract Res Clin Rheumatol 33(3):101418. https://doi.org/10.1016/j.berh.2019.05.003
Acknowledgements
The authors thank all the colleagues at the Guilan University of Medical Sciences, Rasht, Iran, who contributed to this research.
Funding
The source of funding was the Guilan University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
B.G.H. and A.B. contributed equally to the design of the work; all the authors made substantial contributions to the acquisition, analysis, interpretation of data, and first draft of the article. All the authors read and approved the final manuscript. They agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval
The study protocol was approved by the ethics committee of Guilan University of Medical Sciences (IR.GUMS.REC.1398.208) in accordance with the World Medical Association’s code of ethics (Declaration of Helsinki, revised in Brazil 2013) and registered at an ICMJE-recognized registry of clinical trials (IRCT20181113041646N1; www.irct.ir).
Consent to participate
All participants were clearly informed about the study design and written informed consent was obtained from all volunteers.
Consent for publication
All participants gave their written consent on the publication of their clinical data. They were assured that their names will not be revealed.
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ghavidel-Parsa, B., Bidari, A., Rahimi, A. et al. No effect of approved fibromyalgia drugs on the social pain (invalidation) contrary to physical pain: an open-label short-term randomized clinical trial. Clin Rheumatol 41, 245–254 (2022). https://doi.org/10.1007/s10067-021-05890-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-021-05890-6