Abstract
Objective
To examine the associations between restless sleep and knee symptoms among individuals with radiographically confirmed KOA.
Methods
Cross-sectional and longitudinal associations were examined using Osteoarthritis Initiative (OAI) data. Participants with radiographic KOA (n = 2517) were asked how often sleep was restless in the past week over the 4 years, and the Western Ontario and McMaster Universities Arthritis Index (WOMAC) was used to measure knee symptoms. Adjusted β coefficients (aβ) and 95% confidence intervals (CI) were derived from generalized estimating equations (GEEs) models stratified by sex.
Results
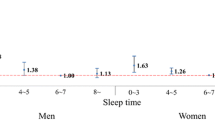
One in 7 participants reported ≥ 3 nights with restless sleep. Cross-sectional analyses indicated that restless sleep 5–7 nights was associated with worse symptoms (Women: pain: aβ 1.93, 95% CI 1.12–2.74, stiffness: aβ 0.57, 95% CI 0.19–0.94, physical function: aβ 5.68, 95% CI 3.09-8.27; Men: pain: aβ = 1.85, 95% CI 0.85–2.86; stiffness: aβ 0.63, 95% CI 0.15–1.12; physical function: aβ 5.89, 95% CI 2.68–9.09) compared with < 1 night. Longitudinal analyses confirmed that more nights with restless sleep were associated with worse pain (P trend = 0.01) and function (P trend = 0.04) in women and physical function in men (P trend = 0.04), although estimates did not meet thresholds for minimal clinically meaningful differences.
Conclusion
While the analysis of cross-sectional data supported the association between restless sleep and KOA symptoms, such relationships were not confirmed in more robust longitudinal analysis. Further research examining whether sleep quality, duration, or disorders is associated with worsening symptoms in persons with KOA is warranted.
Key Points • The prevalence of frequent restless sleep among persons with knee OA is not uncommon. • There were linear trends between frequency of restless sleep and self-reported symptoms of the knee in cross-sectional analyses. • In the more robust longitudinal analysis, despite the statistically significant linear trends observed between frequency of restless sleep and symptoms (women: pain and physical function; men: function), none appeared to reach the a priori selected ranges for minimally clinically relevant differences. |
Similar content being viewed by others
Data availability
The datasets used in the current study are available through the Osteoarthritis Initiative website: https://nda.nih.gov/oai/.
References
Brault M, Hootman J, Helmick CG, Thesis KAAB (2009) Prevalence and most common causes of disability among adults--United States, 2005. MMWR Morb Mortal Wkly Rep 58:421–426
Felson DT, Lawrence RC, Dieppe PA, Hirsch R, Helmick CG, Jordan JM, Kington RS, Lane NE, Nevitt MC, Zhang Y, Sowers M, McAlindon T, Spector TD, Poole AR, Yanovski SZ, Ateshian G, Sharma L, Buckwalter JA, Brandt KD, Fries JF (2000) Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med 133:635–646
Oliveria SA, Felson DT, Reed JI, Cirillo PA, Walker AM (1995) Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis Rheum 38:1134–1141. https://doi.org/10.1002/art.1780380817
Losina E, Weinstein AM, Reichmann WM, Burbine SA, Solomon DH, Daigle ME, Rome BN, Chen SP, Hunter DJ, Suter LG, Jordan JM, Katz JN (2013) Lifetime risk and age at diagnosis of symptomatic knee osteoarthritis in the US. Arthritis Care Res 65:703–711. https://doi.org/10.1002/acr.21898
Dillon CF, Rasch EK, Gu Q, Hirsch R (2006) Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991-94. J Rheumatol 33:2271–2279
Kramer JS, Yelin EH, Epstein WV, Kramer J (1983) Social and economic impacts of four musculoskeletal conditions. A study using national community-based data. Arthritis Rheum 26:901–907
Kotlarz H, Gunnarsson CL, Fang H, Rizzo JA (2010) Osteoarthritis and absenteeism costs: evidence from US national survey data. J Occup Environ Med 52:263–268. https://doi.org/10.1097/JOM.0b013e3181cf00aa
Kotlarz H, Gunnarsson CL, Fang H (2009) Insurer and out-of-pocket costs of osteoarthritis in the US: evidence from national survey data. Arthritis Rheum 60:3546–3553
Guccione AA, Felson DT, Anderson JJ, Anthony JM, Zhang Y, Wilson PW, Kelly-Hayes M, Wolf PA, Kreger BE, Kannel WB (1994) The effects of specific medical conditions on the functional limitations of elders in the Framingham study. Am J Public Health 84:351–358. https://doi.org/10.2105/AJPH.84.3.351
Oak SR, Ghodadra A, Winalski CS, Miniaci A, Jones MH (2013) Radiographic joint space width is correlated with 4-year clinical outcomes in patients with knee osteoarthritis: data from the osteoarthritis initiative. Osteoarthr Cartil 21:1185–1190. https://doi.org/10.1016/j.joca.2013.06.024
Taylor SS, Hughes JM, Coffman CJ, Jeffreys AS, Ulmer CS, Oddone EZ, Bosworth HB, Yancy WS Jr, Allen KD (2018) Prevalence of and characteristics associated with insomnia and obstructive sleep apnea among veterans with knee and hip osteoarthritis. BMC Musculoskelet Disord 19:79. https://doi.org/10.1186/s12891-018-1993-y
Whibley D, Braley TJ, Kratz AL, Murphy SL (2019) Transient effects of sleep on next-day pain and fatigue in older adults with symptomatic osteoarthritis. J Pain 20:1373–1382. https://doi.org/10.1016/j.jpain.2019.04.011
Campbell CM, Buenaver LF, Finan P, Bounds SC, Redding M, McCauley L, Robinson M, Edwards RR, Smith MT (2015) Sleep, pain catastrophizing, and central sensitization in knee osteoarthritis patients with and without insomnia. Arthritis Care Res 67:1387–1396. https://doi.org/10.1002/acr.22609
Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, Towheed T, Welch V, Wells G, Tugwell P, American College of Rheumatology (2012) American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res 64:465–474. https://doi.org/10.1002/acr.21596
Walach H (2002) The efficacy paradox in randomized controlled trials of CAM and elsewhere: beware of the placebo trap. J Altern Complement Med 7:213–218. https://doi.org/10.1089/107555301300328070
Zou K, Wong J, Abdullah N, Chen X, Smith T, Doherty M, Zhang W (2016) Examination of overall treatment effect and the proportion attributable to contextual effect in osteoarthritis: meta-analysis of randomised controlled trials. Ann Rheum Dis 75:1964–1970. https://doi.org/10.1136/annrheumdis-2015-208387
Gilbert AL, Lee J, Song J, Semanik PA, Ehrlich-Jones LS, Kwoh CK, Dunlop DD, Chang RW (2018) Relationship between self-reported restless sleep and objectively measured physical activity in adults with knee osteoarthritis. Arthritis Care & Research. https://doi.org/10.1002/acr.23581
Song J, Dunlop DD, Semanik PA, Chang AH, Lee YC, Gilbert AL, Jackson RD, Chang RW, Lee J (2018) Reallocating time spent in sleep, sedentary behavior and physical activity and its association with pain: a pilot sleep study from the Osteoarthritis Initiative. Osteoarthr Cartil 26:1595–1603. https://doi.org/10.1016/j.joca.2018.07.002
Tang NKY, Lereya ST, Boulton H, Miller MA, Wolke D, Cappuccio FP (2015) Nonpharmacological treatments of insomnia for long-term painful conditions: a systematic review and meta-analysis of patient-reported outcomes in randomized controlled trials. Sleep 38:1751–1764. https://doi.org/10.5665/sleep.5158
Radloff LS (1977) The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl Psychol Meas 1:385–401. https://doi.org/10.1177/014662167700100306
Burgard SA, Ailshire JA (2009) Putting Work to Bed: Stressful Experiences on the Job and Sleep Quality. J Health Soc Behav 50:476–492. https://doi.org/10.1177/002214650905000407
Leggett A, Burgard S, Zivin K (2016) The impact of sleep disturbance on the association between stressful life events and depressive symptoms. J Gerontol Ser B Psychol Sci Soc Sci 71:118–128. https://doi.org/10.1093/geronb/gbv072
Fülöp T, Hickson DA, Wyatt SB et al (2012) Sleep-disordered breathing symptoms among African-Americans in the Jackson Heart Study. Sleep Med 13:1039–1049. https://doi.org/10.1016/j.sleep.2012.06.005
Roos EM, Klässbo M, Lohmander LS (1999) WOMAC osteoarthritis index. Reliability, validity, and responsiveness in patients with arthroscopically assessed osteoarthritis. Western Ontario and MacMaster Universities. Scand J Rheumatol 28:210–215
Duryea J, Li J, Peterfy CG, Gordon C, Genant HK (2000) Trainable rule-based algorithm for the measurement of joint space width in digital radiographic images of the knee. Med Phys 27:580–591. https://doi.org/10.1118/1.598897
Ware JE, Kosinski M, Keller SD (1996) A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity. Med Care 34:220–233. https://doi.org/10.1097/00005650-199603000-00003
Katz JN, Chang LC, Sangha O et al (1996) Can Comorbidity Be Measured by Questionnaire Rather than Medical Record Review? Med Care 34:73–84. https://doi.org/10.1097/00005650-199601000-00006
Washburn RA, Ficker JL (1999) Physical Activity Scale for the Elderly (PASE): the relationship with activity measured by a portable accelerometer. J Sports Med Phys Fitness 39:336–340
Zhang J, Lam SP, Li SX, Tang NL, Yu MWM, Li AM, Wing YK (2012) Insomnia, sleep quality, pain, and somatic symptoms: Sex differences and shared genetic components. Pain 153:666–673. https://doi.org/10.1016/j.pain.2011.12.003
Rifbjerg-Madsen S, Christensen AW, Christensen R, Hetland ML, Bliddal H, Kristensen LE, Danneskiold-Samsøe B, Amris K (2017) Pain and pain mechanisms in patients with inflammatory arthritis: A Danish nationwide cross-sectional DANBIO registry survey. PLoS One 12:e0180014
Koffel E, Kroenke K, Bair MJ, Leverty D, Polusny MA, Krebs EE (2016) The bidirectional relationship between sleep complaints and pain: Analysis of data from a randomized trial. Health Psychol 35:41–49. https://doi.org/10.1037/hea0000245
Frohnhofen H (2018) Pain and sleep. Z Gerontol Geriatr 51:871–874. https://doi.org/10.1007/s00391-018-01461-8
Twisk J (2003) Applied Longitudinal Data Analysis for Epidemiology: A Practical Guide. Cambridge University Press, New York
Atkinson JH, Ancoli-Israel S, Slater MA, Garfin SR, Gillin C (1988) Subjective sleep disturbance in chronic back pain. Clin J Pain 4:225–232. https://doi.org/10.1097/00002508-198812000-00007
Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ (2007) Comorbidity of chronic insomnia with medical problems. Sleep 30:213–218
Moldofsky H, Scarisbrick P (1976) Induction of neurasthenic musculoskeletal pain syndrome by selective sleep stage deprivation. Psychosom Med 38:35–44. https://doi.org/10.1097/00006842-197601000-00006
Irwin MR, Olmstead R, Carrillo C, Sadeghi N, FitzGerald JD, Ranganath VK, Nicassio PM (2012) Sleep Loss Exacerbates Fatigue, Depression, and Pain in Rheumatoid Arthritis. Sleep 35:537–543. https://doi.org/10.5665/sleep.1742
Haack M, Sanchez E, Mullington JM (2007) Elevated inflammatory markers in response to prolonged sleep restriction are associated with increased pain experience in healthy volunteers. Sleep 30:1145–1152
Kutner NG, Bliwise DL, Brogan D, Zhang R (2001) Race and Restless Sleep Complaint in Older Chronic Dialysis Patients and Nondialysis Community Controls. J Gerontol Ser B 56:P170–P175. https://doi.org/10.1093/geronb/56.3.P170
Fertelli TK, Tuncay FO (2019) Fatigue in individuals with knee osteoarthritis: Its relationship with sleep quality, pain and depression. Pakistan J Med Sci 35:1040–1044. https://doi.org/10.12669/pjms.35.4.383
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA (2010) Sleep duration and all-cause mortality: A systematic review and meta-analysis of prospective studies. Sleep 33:585–592. https://doi.org/10.1093/sleep/33.5.585
Jiawei Y, Xiaoling J, Zhilei S et al (2019) Relationship of Sleep Duration With All-Cause Mortality and Cardiovascular Events: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. J Am Heart Assoc 6:e005947. https://doi.org/10.1161/JAHA.117.005947
Shi L, Chen SJ, Ma MY, Bao YP, Han Y, Wang YM, Shi J, Vitiello MV, Lu L (2018) Sleep disturbances increase the risk of dementia: A systematic review and meta-analysis. Sleep Med Rev 40:4–16. https://doi.org/10.1016/j.smrv.2017.06.010
Bubu OM, Brannick M, Mortimer J et al (2017) Sleep, Cognitive impairment, and Alzheimer’s disease: A Systematic Review and Meta-Analysis. Sleep 40. https://doi.org/10.1093/sleep/zsw084
Funding
This work was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health (grant no. R21AR076641). The OAI is a public-private partnership composed of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories, Novartis Pharmaceuticals Corporation, GlaxoSmithKline, and Pfizer, Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners.
Competing interests
The authors declare that they have no competing interests.
Ethics approval
This study used publicly available data from the OAI and, as such, the University of Massachusetts Institutional Review Board considered this study exempt, and the informed consent was waived.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lapane, K.L., Shridharmurthy, D., Harkey, M.S. et al. The relationship between restless sleep and symptoms of the knee: data from the Osteoarthritis Initiative. Clin Rheumatol 40, 2167–2175 (2021). https://doi.org/10.1007/s10067-020-05531-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05531-4