Abstract
Objectives
To assess the serum iron and ferritin levels in relation to the prevalence of hyperuricemia (HU) and the serum uric acid (SUA) level.
Methods
Serum iron and ferritin concentrations were detected by Ferene method and chemiluminescence method, respectively. SUA level was detected by uricase-PAP method. HU was defined as SUA ≥ 416 μmol/L for male and ≥ 357 μmol/L for female. Multivariable-adjusted logistic regressions were constructed to investigate the associations between serum iron/ferritin levels and prevalence of HU. Pearson correlation analysis and multivariable linear regression were performed to examine the correlations between serum iron/ferritin levels and SUA level.
Results
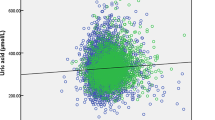
A total of 2824 subjects (mean age 52.2 ± 7.2) were included. The overall prevalence of HU was 17.3%. Compared with the lowest quartile, the multivariable-adjusted odds ratios (OR) and its 95% confidence interval (CI) of HU were 1.33 (95%CI 0.97–1.82), 1.17 (95%CI 0.85–1.60), and 1.56 (95%CI 1.14–2.13) in the second, third, and fourth quartiles of serum iron, respectively (P for trend = 0.012), and were 1.29 (95%CI 0.89–1.88) in the second, 2.13 (95%CI 1.47–3.07) in the third, and 2.25 (95%CI 1.54–3.29) in the fourth quartile of serum ferritin (P for trend < 0.001). Pearson correlation coefficient indicated a weak positive correlation between serum iron (r = 0.2, P < 0.001) and ferritin (r = 0.3, P < 0.001) levels and SUA. Such positive correlations were further confirmed by multiple linear regression (serum iron: standardized β = 0.059, P < 0.001; serum ferritin: standardized β = 0.061, P = 0.001).
Conclusions
Both serum iron and ferritin showed a positive correlation with the prevalence of HU, and a weak positive correlation with SUA level.
Key Points • Subjects with higher levels of serum iron or ferritin had higher prevalence of HU. • There was a weak positive correlation between serum iron/ferritin levels and SUA level. |


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding authors, HL and YX, upon reasonable request.
Abbreviations
- HU:
-
hyperuricemia
- SUA:
-
serum uric acid
- FBG:
-
fasting blood glucose
- LDL-cholesterol:
-
low-density lipoprotein cholesterol
- HDL-cholesterol:
-
high-density lipoprotein cholesterol
- TG:
-
triglyceride
- SBP:
-
systolic blood pressure
- DBP:
-
diastolic blood pressure
- OR:
-
odds ratio
- CI:
-
confidence interval
- eGFR:
-
estimated glomerular filtration rate
- XOR:
-
xanthine oxidoreductase
References
Waring WS, Webb DJ, Maxwell SR (2001) Systemic uric acid administration increases serum antioxidant capacity in healthy volunteers. J Cardiovasc Pharmacol 38(3):365–371. https://doi.org/10.1097/00005344-200109000-00005
Hou H, Xu X, Sun F, Zhang X, Dong H, Wang L, Ge S, An K, Sun Q, Li Y, Cao W, Song M, Hu S, Xing W, Wang W, Li D, Wang Y (2019) Hyperuricemia is associated with immunoglobulin G N-glycosylation: a community-based study of glycan biomarkers. OMICS 23:660–667. https://doi.org/10.1089/omi.2019.0004
Arrebola JP, Ramos JJ, Bartolome M, Esteban M, Huetos O, Canas AI, Lopez-Herranz A, Calvo E, Perez-Gomez B, Castano A, Bioambient. Es (2019) Associations of multiple exposures to persistent toxic substances with the risk of hyperuricemia and subclinical uric acid levels in BIOAMBIENT.ES study. Environ Int 123:512–521. https://doi.org/10.1016/j.envint.2018.12.030
Chen-Xu M, Yokose C, Rai SK, Pillinger MH, Choi HK (2019) Contemporary prevalence of gout and hyperuricemia in the United States and decadal trends: the National Health and Nutrition Examination Survey 2007-2016. Arthritis Rheum 71:991–999. https://doi.org/10.1002/art.40807
Trifiro G, Morabito P, Cavagna L, Ferrajolo C, Pecchioli S, Simonetti M, Bianchini E, Medea G, Cricelli C, Caputi AP, Mazzaglia G (2013) Epidemiology of gout and hyperuricaemia in Italy during the years 2005-2009: a nationwide population-based study. Ann Rheum Dis 72(5):694–700. https://doi.org/10.1136/annrheumdis-2011-201254
Liu R, Han C, Wu D, Xia X, Gu J, Guan H, Shan Z, Teng W (2015) Prevalence of Hyperuricemia and gout in mainland China from 2000 to 2014: a systematic review and meta-analysis. Biomed Res Int 2015:762820–762812. https://doi.org/10.1155/2015/762820
Billa G, Dargad R, Mehta A (2018) Prevalence of Hyperuricemia in Indian subjects attending Hyperuricemia screening programs-a retrospective study. J Assoc Physicians India 66(4):43–46
Zhu Y, Pandya BJ, Choi HK (2011) Prevalence of gout and hyperuricemia in the US general population: the National Health and Nutrition Examination Survey 2007-2008. Arthritis Rheum 63(10):3136–3141. https://doi.org/10.1002/art.30520
Chen S, Du H, Wang Y, Xu L (1998) The epidemiology study of hyperuricemia and gout in a community population of Huangpu District in Shanghai. Chin Med J 111(3):228–230
Huang H, Huang B, Li Y, Huang Y, Li J, Yao H, Jing X, Chen J, Wang J (2014) Uric acid and risk of heart failure: a systematic review and meta-analysis. Eur J Heart Fail 16(1):15–24. https://doi.org/10.1093/eurjhf/hft132
Zhu Y, Pandya BJ, Choi HK (2012) Comorbidities of gout and hyperuricemia in the US general population: NHANES 2007-2008. Am J Med 125(7):679–687.e671. https://doi.org/10.1016/j.amjmed.2011.09.033
Ford ES, Li C, Cook S, Choi HK (2007) Serum concentrations of uric acid and the metabolic syndrome among US children and adolescents. Circulation 115(19):2526–2532. https://doi.org/10.1161/CIRCULATIONAHA.106.657627
Wang H, Zhang H, Sun L, Guo W (2018) Roles of hyperuricemia in metabolic syndrome and cardiac-kidney-vascular system diseases. Am J Transl Res 10(9):2749–2763
Fernández-Real JM, Manco M (2014) Effects of iron overload on chronic metabolic diseases. Lancet Diabetes Endocrinol 2(6):513–526. https://doi.org/10.1016/s2213-8587(13)70174-8
Schmidt PJ (2015) Regulation of Iron metabolism by Hepcidin under conditions of inflammation. J Biol Chem 290(31):18975–18983. https://doi.org/10.1074/jbc.R115.650150
Flais J, Bardou-Jacquet E, Deugnier Y, Coiffier G, Perdriger A, Chales G, Ropert M, Loreal O, Guggenbuhl P (2017) Hyperferritinemia increases the risk of hyperuricemia in HFE-hereditary hemochromatosis. Joint Bone Spine 84(3):293–297. https://doi.org/10.1016/j.jbspin.2016.05.020
Haap M, Fritsche A, Mensing HJ, Haring HU, Stumvoll M (2003) Association of high serum ferritin concentration with glucose intolerance and insulin resistance in healthy people. Ann Intern Med 139(10):869–871. https://doi.org/10.7326/0003-4819-139-10-200311180-00029
Dasgupta S, Dasgupta A, Mukhopadhayay T, Bhattacharya S, Swaika B, Banarjee U, Chakrabarty P (2013) Serum uric acid: an early indicator of oxidative stress in beta thalassemia population. Mymensingh Med J 22(3):567–573
Budzyn M, Iskra M, Krasinski Z, Dzieciuchowicz L, Kasprzak M, Gryszczynska B (2011) Serum iron concentration and plasma oxidant-antioxidant balance in patients with chronic venous insufficency. Med Sci Monit 17(12):CR719–CR727. https://doi.org/10.12659/msm.882132
Zeng C, Wei J, Li H, Yang T, Zhang FJ, Pan D, Xiao YB, Yang TB, Lei GH (2015) Relationship between serum magnesium concentration and radiographic knee osteoarthritis. J Rheumatol 42(7):1231–1236. https://doi.org/10.3899/jrheum.141414
Zeng C, Wang YL, Wei J, Yang T, Li H, Xie DX, Li YS, Lei GH (2015) Association between low serum magnesium concentration and hyperuricemia. Magnes Res 28(2):56–63. https://doi.org/10.1684/mrh.2015.0384
Zeng C, Wei J, Terkeltaub R, Yang T, Choi HK, Wang YL, Xie DX, Hunter DJ, Zhang Y, Li H, Cui Y, Li LJ, Lei GH (2017) Dose-response relationship between lower serum magnesium level and higher prevalence of knee chondrocalcinosis. Arthritis Res Ther 19(1):236. https://doi.org/10.1186/s13075-017-1450-6
Zhang YN, Xu C, Xu L, Yu C, Miao M, Xie J, Li Y (2014) High serum ferritin levels increase the risk of hyperuricemia: a cross-sectional and longitudinal study. Ann Nutr Metab 64(1):6–12. https://doi.org/10.1159/000358337
Zhang W, Doherty M, Pascual E, Bardin T, Barskova V, Conaghan P, Gerster J, Jacobs J, Leeb B, Liote F, McCarthy G, Netter P, Nuki G, Perez-Ruiz F, Pignone A, Pimentao J, Punzi L, Roddy E, Uhlig T, Zimmermann-Gorska I, Therapeutics ESCfICSI (2006) EULAR evidence based recommendations for gout. Part I: diagnosis. Report of a task force of the standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis 65(10):1301–1311. https://doi.org/10.1136/ard.2006.055251
Veronese N, Stubbs B, Trevisan C, Bolzetta F, De Rui M, Maggi S, Sartori L, Musacchio E, Zambon S, Perissinotto E, Noale M, Crepaldi G, Manzato E, Sergi G (2017) Results of an observational cohort study of Hyperuricemia as a predictor of poor physical performance in the elderly. Arthritis Care Res 69(8):1238–1244. https://doi.org/10.1002/acr.23118
Levey AS, Stevens LA, Schmid CH, Zhang Y, Castro AF, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
Ghio AJ, Ford ES, Kennedy TP, Hoidal JR (2005) The association between serum ferritin and uric acid in humans. Free Radic Res 39(3):337–342. https://doi.org/10.1080/10715760400026088
Kuo CC, Weaver V, Fadrowski JJ, Lin YS, Guallar E, Navas-Acien A (2015) Arsenic exposure, hyperuricemia, and gout in US adults. Environ Int 76:32–40. https://doi.org/10.1016/j.envint.2014.11.015
Hunnicutt J, He K, Xun P (2014) Dietary iron intake and body iron stores are associated with risk of coronary heart disease in a meta-analysis of prospective cohort studies. J Nutr 144(3):359–366. https://doi.org/10.3945/jn.113.185124
van der A D, Grobbee DE, Roest M, Marx JJ, Voorbij HA, van der Schouw YT (2005) Serum ferritin is a risk factor for stroke in postmenopausal women. Stroke 36(8):1637–1641. https://doi.org/10.1161/01.STR.0000173172.82880.72
Mainous AG 3rd, Knoll ME, Everett CJ, Matheson EM, Hulihan MM, Grant AM (2011) Uric acid as a potential cue to screen for iron overload. J Am Board Fam Med 24(4):415–421. https://doi.org/10.3122/jabfm.2011.04.110015
Li X, He T, Yu K, Lu Q, Alkasir R, Guo G, Xue Y (2018) Markers of Iron status are associated with risk of Hyperuricemia among Chinese adults: nationwide population-based study. Nutrients 10(2):E191. https://doi.org/10.3390/nu10020191
Chen C, Lü J-M, Yao Q (2016) Hyperuricemia-related diseases and xanthine oxidoreductase (XOR) inhibitors: an overview. Med Sci Monit 22:2501–2512. https://doi.org/10.12659/msm.899852
Martelin E, Lapatto R, Raivio KO (2002) Regulation of xanthine oxidoreductase by intracellular iron. Am J Phys Cell Phys 283(6):C1722–C1728. https://doi.org/10.1152/ajpcell.00280.2002
Zeng QY, Chen R, Darmawan J, Xiao ZY, Chen SB, Wigley R, Le Chen S, Zhang NZ (2008) Rheumatic diseases in China. Arthritis Res Ther 10(1):R17. https://doi.org/10.1186/ar2368
Kelley MK, Amy NK (1984) Effect of molybdenum-deficient and low iron diets on xanthine oxidase activity and iron status in rats. J Nutr 114(9):1652–1659. https://doi.org/10.1093/jn/114.9.1652
Ghio AJ, Kennedy TP, Stonehuerner J, Carter JD, Skinner KA, Parks DA, Hoidal JR (2002) Iron regulates xanthine oxidase activity in the lung. Am J Phys Lung Cell Mol Phys 283(3):L563–L572. https://doi.org/10.1152/ajplung.00413.2000
Huang J, Jones D, Luo B, Sanderson M, Soto J, Abel ED, Cooksey RC, McClain DA (2011) Iron overload and diabetes risk: a shift from glucose to fatty acid oxidation and increased hepatic glucose production in a mouse model of hereditary hemochromatosis. Diabetes 60(1):80–87. https://doi.org/10.2337/db10-0593
Valenti L, Fracanzani AL, Dongiovanni P, Bugianesi E, Marchesini G, Manzini P, Vanni E, Fargion S (2007) Iron depletion by phlebotomy improves insulin resistance in patients with nonalcoholic fatty liver disease and hyperferritinemia: evidence from a case-control study. Am J Gastroenterol 102(6):1251–1258. https://doi.org/10.1111/j.1572-0241.2007.01192.x
Quinones Galvan A, Natali A, Baldi S, Frascerra S, Sanna G, Ciociaro D, Ferrannini E (1995) Effect of insulin on uric acid excretion in humans. Am J Phys 268(1 Pt 1):E1–E5. https://doi.org/10.1152/ajpendo.1995.268.1.E1
Modan M, Halkin H, Karasik A, Lusky A (1987) Elevated serum uric acid--a facet of hyperinsulinaemia. Diabetologia 30(9):713–718. https://doi.org/10.1007/bf00296994
Author contribution statement
HL, YX, and YW conceived the study. HL, YX, and YW were responsible for conception of the study and drafted the manuscript. HL and YX were responsible for design of the study. ZY, JW, DX, and TY contributed to preparation and data analysis. HL and YX contributed to revision of the manuscript. HL and YX were accountable for all aspects of the work. All the authors contributed to the interpretation of the data and critically reviewed the manuscript for publication. All authors read and approved the final manuscript.
Funding
This work was funded by the National Natural Science Foundation of China (81601941, 81772413, 81702207, 81702206); the Key Research and Development Program of Hunan Province (2018SK2070); the Postdoctoral Science Foundation of Central South University (182130); the Young Investigator Grant of Xiangya Hospital, Central South University (2016Q03, 2016Q06); the Xiangya Clinical Big Data System Construction Project of Central South University (45); the Clinical Scientific Research Foundation of Xiangya Hospital, Central South University (2015L03); the Natural Science Foundation of Hunan Province (2017JJ3491, 2017JJ3492); and the innovation Foundation of the Central South University for Postgraduate (2018zzts045).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
None.
Ethical approval and informed consent
The study protocol had been approved by the Ethics Committee of Xiangya Hospital, Central South University (reference number: 201312459). All persons gave their informed consent prior to their inclusion in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Y., Yang, Z., Wu, J. et al. Associations of serum iron and ferritin with hyperuricemia and serum uric acid. Clin Rheumatol 39, 3777–3785 (2020). https://doi.org/10.1007/s10067-020-05164-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05164-7