Abstract
Objectives
This study aimed to determine trends in the prevalence of chronic opioid users among patients with chronic gout in South Korea from 2002 to 2015 and to investigate the factors associated with chronic opioid use among patients with chronic gout.
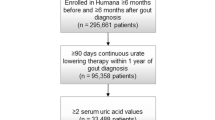
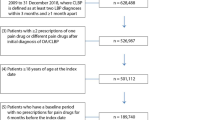
Methods
We performed a population-based cohort study and extracted data from the National Health Insurance Service database in South Korea. We included all adult patients (age ≥ 18 years) with a diagnostic code of M1A* (chronic gout) according to the International Classification of Disease (10th revision).
Results
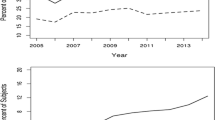
The prevalence of chronic opioid users among patients with chronic gout has gradually increased from 4.0% in 2002 to 19.4% in 2015. After excluding the patients who had a history of cancer or other rheumatic diseases, a total of 18,042 patients with chronic gout were included in this cross-sectional cohort study in 2015, of which 993 (5.5%) were long-term opioid users. In a multivariable model, older age, female sex, Charlson Comorbidity Index > 2, long-term use of other analgesics, such as pregabalin, gabapentin, paracetamol, and glucocorticoids, and the use of other gout medication (colchicine) were independently associated with higher rates of long-term opioid use among patients with chronic gout.
Conclusion
Chronic opioid users among patients with chronic gout increased from 2002 to 2015 in South Korea. Female sex, older age, comorbid status, and the use of other non-opioid analgesics were independently associated with higher rates of long-term opioid use among patients with chronic gout.
Key Points • Chronic opioid users among patients with chronic gout have increased from 2002 to 2015 in South Korea. • Among patients with chronic gout, 5.5% were long-term opioid users. • Female sex, older age, comorbid status, and the use of other non-opioid analgesics were associated with higher rates of long-term opioid use. |

Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Ragab G, Elshahaly M, Bardin T (2017) Gout: an old disease in new perspective - a review. J Adv Res 8(5):495–511. https://doi.org/10.1016/j.jare.2017.04.008
Kim KY, Ralph Schumacher H, Hunsche E, Wertheimer AI, Kong SX (2003) A literature review of the epidemiology and treatment of acute gout. Clin Ther 25(6):1593–1617. https://doi.org/10.1016/s0149-2918(03)80158-3
Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, Gabriel S, Hirsch R, Hochberg MC, Hunder GG, Jordan JM, Katz JN, Kremers HM, Wolfe F, National Arthritis Data W (2008) Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum 58(1):26–35. https://doi.org/10.1002/art.23176
Kuo CF, Grainge MJ, Zhang W, Doherty M (2015) Global epidemiology of gout: prevalence, incidence and risk factors. Nat Rev Rheumatol 11(11):649–662. https://doi.org/10.1038/nrrheum.2015.91
Richette P, Bardin T (2010) Gout. Lancet 375(9711):318–328. https://doi.org/10.1016/S0140-6736(09)60883-7
Xia Y, Wu Q, Wang H, Zhang S, Jiang Y, Gong T, Xu X, Chang Q, Niu K, Zhao Y (2019) Global, regional and national burden of gout, 1990-2017: a systematic analysis of the Global Burden of Disease Study. Rheumatology (Oxford). https://doi.org/10.1093/rheumatology/kez476
Singh JA, Cleveland JD (2019) Gout and chronic pain in older adults: a Medicare claims study. Clin Rheumatol 38(7):1953–1960. https://doi.org/10.1007/s10067-019-04526-0
Shekelle PG, Newberry SJ, FitzGerald JD, Motala A, O'Hanlon CE, Tariq A, Okunogbe A, Han D, Shanman R (2017) Management of Gout: a systematic review in support of an American College of Physicians Clinical Practice Guideline. Ann Intern Med 166(1):37–51. https://doi.org/10.7326/M16-0461
Dalal DS, Mbuyi N, Shah I, Reinert S, Hilliard R, Reginato A (2019) Prescription opioid use among acute gout patients discharged from the emergency department. Arthritis Care Res (Hoboken). https://doi.org/10.1002/acr.23928
Ray WA, Chung CP, Murray KT, Hall K, Stein CM (2016) Prescription of long-acting opioids and mortality in patients with chronic noncancer pain. JAMA 315(22):2415–2423. https://doi.org/10.1001/jama.2016.7789
Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M, Initiative S (2007) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med 4(10):e297. https://doi.org/10.1371/journal.pmed.0040297
Lee J, Lee JS, Park SH, Shin SA, Kim K (2017) Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol 46(2):e15. https://doi.org/10.1093/ije/dyv319
Jiang X, Orton M, Feng R, Hossain E, Malhotra NR, Zager EL, Liu R (2017) Chronic opioid usage in surgical patients in a large academic center. Ann Surg 265(4):722–727. https://doi.org/10.1097/SLA.0000000000001780
Pereira J, Lawlor P, Vigano A, Dorgan M, Bruera E (2001) Equianalgesic dose ratios for opioids. A critical review and proposals for long-term dosing. J Pain Symptom Manag 22(2):672–687
De Meulemeester M, Mateus E, Wieberneit-Tolman H, Betteridge N, Ireland L, Petersen G, Maske NJ, Jansen TL, Perez-Ruiz F (2020) Understanding the patient voice in gout: a quantitative study conducted in Europe. BJGP Open. https://doi.org/10.3399/bjgpopen20X101003
Brook RA, Forsythe A, Smeeding JE, Lawrence Edwards N (2010) Chronic gout: epidemiology, disease progression, treatment and disease burden. Curr Med Res Opin 26(12):2813–2821. https://doi.org/10.1185/03007995.2010.533647
Oh TK, Jeon YT, Choi JW (2019) Trends in chronic opioid use and association with five-year survival in South Korea: a population-based cohort study. Br J Anaesth 123(5):655–663. https://doi.org/10.1016/j.bja.2019.08.012
Oh TK, Song IA, Lee JH, Lim C, Jeon YT, Bae HJ, Jo YH, Jee HJ (2019) Preadmission chronic opioid usage and its association with 90-day mortality in critically ill patients: a retrospective cohort study. Br J Anaesth 122(6):e189–e197. https://doi.org/10.1016/j.bja.2019.03.032
Fam AG (1998) Gout in the elderly. Clinical presentation and treatment. Drugs Aging 13(3):229–243. https://doi.org/10.2165/00002512-199813030-00006
Bolzetta F, Veronese N, Manzato E, Sergi G (2013) Chronic gout in the elderly. Aging Clin Exp Res 25(2):129–137
De Souza A, Fernandes V, Ferrari AJ (2005) Female gout: clinical and laboratory features. J Rheumatol 32(11):2186–2188
Park YB, Park YS, Song J, Lee WK, Suh CH, Lee SK (2000) Clinical manifestations of Korean female gouty patients. Clin Rheumatol 19(2):142–146. https://doi.org/10.1007/s100670050033
Khanna PP, Gladue HS, Singh MK, FitzGerald JD, Bae S, Prakash S, Kaldas M, Gogia M, Berrocal V, Townsend W Treatment of acute gout: a systematic review. In: Seminars in arthritis and rheumatism, 2014. vol 1. Elsevier, pp 31–38
Choi HK, Atkinson K, Karlson EW, Willett W, Curhan G (2004) Alcohol intake and risk of incident gout in men: a prospective study. Lancet 363(9417):1277–1281. https://doi.org/10.1016/S0140-6736(04)16000-5
Neogi T, Jansen TL, Dalbeth N, Fransen J, Schumacher HR, Berendsen D, Brown M, Choi H, Edwards NL, Janssens HJ, Liote F, Naden RP, Nuki G, Ogdie A, Perez-Ruiz F, Saag K, Singh JA, Sundy JS, Tausche AK, Vaquez-Mellado J, Yarows SA, Taylor WJ (2015) 2015 gout classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis 74(10):1789–1798. https://doi.org/10.1136/annrheumdis-2015-208237
Code availability
Not applicable.
Author information
Authors and Affiliations
Contributions
TKO and IAS contributed to the study design and methodology, analyzed the data, and drafted the first manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Disclosures
None.
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Board of Seoul National University Bundang Hospital (no. X-1905-541-902) and the Health Insurance Review and Assessment Service (NHIS-2019-2-160).
Consent for publication
Not applicable.
Consent to participate
Informed consent was waived because data analyses were performed retrospectively with anonymous data derived from the South Korean National Health Insurance Service (NHIS) database.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix. ICD-10 codes
Appendix. ICD-10 codes
The ICD-10 codes used by comorbidity to compute the Charlson comorbidity index are as follows:
○ Myocardial infarction: I21.x, I22.x, I25.2
○ Congestive heart failure: I09.9, I11.0, I13.0, I13.2, I25.5, I42.0, I42.5–I42.9, I43.x, I50.x, P29.0
○ Peripheral vascular disease: I70.x, I71.x, I73.1, I73.8, I73.9, I77.1, I79.0, I79.2, K55.1, K55.8, K55.9, Z95.8, Z95.9
○ Cerebrovascular disease: G45.x, G46.x, H34.0, I60.x–I69.x
○ Dementia: F00.x–F03.x, F05.1, G30.x, G31.1
○ Chronic pulmonary disease: I27.8, I27.9, J40.x–J47.x, J60.x–J67.x, J68.4, J70.1, J70.3
○ Rheumatic disease: M05.x, M06.x, M31.5, M32.x–M34.x, M35.1, M35.3, M36.0
○ Peptic ulcer disease: K25.x–K28.x
○ Mild liver disease: B18.x, K70.0–K70.3, K70.9, K71.3–K71.5, K71.7, K73.x, K74.x, K76.0, K76.2–K76.4, K76.8, K76.9, Z94.4
○ Diabetes without chronic complication: E10.0, E10.1, E10.6, E10.8, E10.9, E11.0, E11.1, E11.6, E11.8, E11.9, E12.0, E12.1, E12.6, E12.8, E12.9, E13.0, E13.1, E13.6, E13.8, E13.9, E14.0, E14.1, E14.6, E14.8, E14.9
○ Diabetes with chronic complication: E10.2–E10.5, E10.7, E11.2–E11.5, E11.7, E12.2–E12.5, E12.7, E13.2–E13.5, E13.7, E14.2–E14.5, E14.7
○ Hemiplegia or paraplegia: G04.1, G11.4, G80.1, G80.2, G81.x, G82.x, G83.0–G83.4, G83.9
○ Renal disease: I12.0, I13.1, N03.2–N03.7, N05.2–N05.7, N18.x, N19.x, N25.0, Z49.0–Z49.2, Z94.0, Z99.2
○ Any malignancy, including lymphoma and leukemia, except malignant neoplasm of skin: C00.x–C26.x, C30.x–C34.x, C37.x–C41.x, C43.x, C45.x–C58.x, C60.x–C76.x, C81.x–C85.x, C88.x, C90.x–C97.x
○ Moderate or severe liver disease: I85.0, I85.9, I86.4, I98.2, K70.4, K71.1, K72.1, K72.9, K76.5, K76.6, K76.7
○ Metastatic solid tumor: C77.x–C80.x
○ AIDS/HIV: B20.x–B22.x, B24.x
Rights and permissions
About this article
Cite this article
Oh, T.K., Song, IA. Long-term opioid use among patients with chronic gout: a cross-sectional study of a sample cohort in South Korea. Clin Rheumatol 39, 3033–3039 (2020). https://doi.org/10.1007/s10067-020-05085-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05085-5