Abstract
Objective
The etiologies of acute respiratory failure in patients with systemic rheumatic diseases (SRDs) requiring intensive care remain unknown. This study was undertaken to investigate the etiologies and outcomes.
Methods
A medical records review study was performed of 259 adult SRDs patients with respiratory failure admitted to medical ICU across a 5-year period. The etiologies were classified as infection, SRD exacerbation, and undetermined. The factors associated with ICU mortality were identified with multivariate logistic regression analysis.
Results
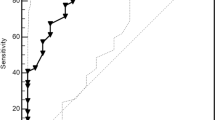
The etiologies of respiratory failure included infection (n = 209, 80.7%), SRD exacerbation (n = 71, 27.4%), and undetermined (n = 21, 8.1%). The most common pathogen was Pneumocystis jirovecii (39.8%), followed by Aspergillus spp. (33.2%), and cytomegalovirus (23.2%). The ICU mortality rate was 59.8%. A high acute physiology and chronic health evaluation II score (OR 1.118, 95% CI 1.054 to 1.186, p < 0.001), a PaO2/FiO2 ratio < 100 mmHg (OR 3.918, 95% CI 2.199 to 6.892, p < 0.001), and a diagnosis of dermatomyositis/polymyositis (OR 4.898, 95% CI 1.949 to 12.309, p = 0.001), vasculitis (OR 3.007, 95% CI 1.237 to 7.309, p = 0.015), and Pneumocystis pneumonia (OR 2.345, 95% CI 1.168 to 4.705, p = 0.016) were associated with increased mortality.
Conclusions
Opportunistic infections and SRD exacerbation were the most common etiologies of acute respiratory failure in patients with SRDs requiring ICU admission, with high ICU mortality. Development of a standard protocol for differential diagnosis in this population might help initiate definitive therapy and improve clinical outcome.
Key Points • Infections, especially with opportunistic infections, were the leading cause of acute respiratory failure in critically ill rheumatology patients, with high mortality. • Severity of illness, certain types of rheumatic diseases, and opportunistic fungal infections were associated with increased mortality. • Using a comprehensive diagnostic workup might help to confirm the infective etiology and improve outcome. |

Similar content being viewed by others
Data availability
All data supporting the conclusions of this article are included in this article and its supplementary file.
References
Janssen NM, Karnad DR, Guntupalli KK (2002) Rheumatologic diseases in the intensive care unit: epidemiology, clinical approach, management, and outcome. Crit Care Clin 18:729–748
Papiris SA, Manali ED, Kolilekas L, Kagouridis K, Maniati M, Filippatos G, Bouros D (2016) Acute respiratory events in connective tissue disorders. Respiration 91:181–201
Dumas G, Géri G, Montlahuc C, Chemam S, Dangers L, Pichereau C, Brechot N, Duprey M, Mayaux J, Schenck M, Boisramé-Helms J, Thomas G, Baboi L, Mouthon L, Amoura Z, Papo T, Mahr A, Chevret S, Chiche JD, Azoulay E (2015) Outcomes in critically ill patients with rheumatic disease: a multicenter study. Chest 148:927–935
Camargo JF, Tobón GJ, Fonseca N, Diaz JL, Uribe M, Molina F, Anaya JM (2005) Autoimmune rheumatic diseases in the intensive care unit: experience from a tertiary referral hospital and review of the literature. Lupus 14:315–320
Moreels M, Mélot C, Leeman M (2005) Prognosis of patients with systemic rheumatic diseases admitted to the intensive care unit. Intensive Care Med 31:591–593
Cavallasca JA, Del Rosario Maliandi M, Sarquis S, Nishishinya MB, Schvartz A, Capdevila A et al (2010) Outcome of patients with systemic rheumatic diseases admitted to a medical intensive care unit. J Clin Rheumatol 16:400–402
Lee J, Yim J, Yang S, Yoo C, Kim YW, Han SK, Lee EY, Lee EB, Song YW, Lee SM (2012) Outcomes of patients with connective tissue disease requiring intensive care for respiratory failure. Rheumatol Int 32:3353–3358
Faguer S, Ciroldi M, Mariotte E, Galicier L, Rybojad M, Canet E et al (2013) Prognostic contributions of the underlying inflammatory disease and acute organ dysfunction in critically ill patients with systemic rheumatic diseases. Eur J Intern Med 24(e):40–44
Wang M, Su S, Lv J, Zhou G, Wang Q, Guo C (2018) Analysis of clinical features and prognostic factors in Chinese patients with rheumatic diseases in an intensive care unit. Egypt Rheumatol 40:63–66
Weng L, Huang X, Chen L, Feng LQ, Jiang W, Hu XY et al (2016) Prognostic factors for severe Pneumocystis jiroveci pneumonia of non-HIV patients in intensive care unit: a bicentric retrospective study. BMC Infect Dis 16:528
Hsu CL, Chen KY, Yeh PS, Hsu YL, Chang HT, Shau WY, Yu CL, Yang PC (2005) Outcome and prognostic factors in critically ill patients with systemic lupus erythematosus: a retrospective study. Crit Care 9:R177–R183
Peng J, Du B, Wang Q, Weng L, Hu XY, Wu CY, Shi Y (2016) Dermatomyositis and polymyositis in the intensive care unit: a single-center retrospective cohort study of 102 patients. PLoS One 11:e0154441
Fauci A, Langford CA (2008) Allergy, clinical immunology and rheumatology. In: Fauci A (ed) Harrison’s principles of internal medicine, 17th edn. New York, McGraw-Hill Medical, pp 885–915
Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E et al (2012) Acute respiratory distress syndrome: the Berlin definition. JAMA 307:2526–2533
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H et al (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med 22:707–710
Shi Y, Rui X, Xie XL, Zhang XJ, Tang B, Liu Y, Zhao H (2013) Effect of diagnostic protocols on etiology and outcome in immunocompromised host with pulmonary infiltrate. Zhonghua Yi Xue Za Zhi 93:684–689
Bradley B, Branley HM, Egan JJ, Greaves MS, Hansell DM, Harrison NK et al (2008) Interstitial lung disease guideline: the British Thoracic Society in collaboration with the Thoracic Society of Australia and New Zealand and the Irish Thoracic Society. Thorax 63(Suppl 5):v1–v58
Cohen AL, Calfee D, Fridkin SK, Huang SS, Jernigan JA, Lautenbach E, Oriola S, Ramsey KM, Salgado CD, Weinstein RA, Society for Healthcare Epidemiology of America and the Healthcare Infection Control Practices Advisory Committee (2008) Society for Healthcare Epidemiology of America and the Healthcare Infection Control Practices Advisory Committee. Recommendations for metrics for multidrug-resistant organisms in healthcare settings: SHEA/HICPAC position paper. Infect Control Hosp Epidemiol 29:901–913
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T et al (2008) Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 46:1813–1821
Harigai M, Koike R, Miyasaka N, Pneumocystis Pneumonia under Anti-Tumor Necrosis Factor Therapy (PAT) Study Group (2007) Pneumocystis pneumonia associated with infliximab in Japan. N Engl J Med 357:1874–1876
Kotton CN, Kumar D, Caliendo AM, Huprikar S, Chou S, Danziger-Isakov L et al (2018) The Third International Consensus Guidelines on the management of cytomegalovirus in solid-organ transplantation. Transplantation 102:900–931
Anaya JM, Diethelm L, Ortiz LA, Gutierrez M, Citera G, Welsh RA, Espinoza LR (1995) Pulmonary involvement in rheumatoid arthritis. Semin Arthritis Rheum 24:242–254
Perez T, Remy-Jardin M, Cortet B (1998) Airways involvement in rheumatoid arthritis: clinical, functional, and HRCT findings. Am J Respir Crit Care Med 157:1658–1665
Doyle JJ, Eliasson AH, Argyros GJ, Dennis GJ, Finger DR, Hurwitz KM, Phillips YY (2000) Prevalence of pulmonary disorders in patients with newly diagnosed rheumatoid arthritis. Clin Rheumatol 19:217–221
Ward MM, Donald F (1999) Pneumocystis carinii pneumonia in patients with connective tissue diseases: the role of hospital experience in diagnosis and mortality. Arthritis Rheum 42:780–789
Wolfe RM, Peacock JE Jr (2017) Pneumocystis pneumonia and the rheumatologist: which patients are at risk and how can PCP be prevented? Curr Rheumatol Rep 19:35
Sowden E, Carmichael AJ (2004) Autoimmune inflammatory disorders, systemic corticosteroids and pneumocystis pneumonia: a strategy for prevention. BMC Infect Dis 4:42
Falagas ME, Manta KG, Betsi GI, Pappas G (2007) Infection-related morbidity and mortality in patients with connective tissue diseases: a systematic review. Clin Rheumatol 26:663–670
Bienvenu A-L, Traore K, Plekhanova I, Bouchrik M, Bossard C, Picot S (2016) Pneumocystis pneumonia suspected cases in 604 non-HIV and HIV patients. Int J Infect Dis 46:11–17
Morris A, Norris KA (2012) Colonization by Pneumocystis jirovecii and its role in disease. Clin Microbiol Rev 25:297–317
Boonsarngsuk V, Sirilak S, Kiatboonsri S (2009) Acute respiratory failure due to Pneumocystis pneumonia: outcome and prognostic factors. Int J Infect Dis 13:59–66
Kim SJ, Lee J, Cho YJ, Park YS, Lee CH, Yoon HI et al (2014) Prognostic factors of Pneumocystis jirovecii pneumonia in patients without HIV infection. J Inf Secur 69:88–95
Fujisawa T, Hozumi H, Kono M, Enomoto N, Hashimoto D, Nakamura Y et al (2014) Prognostic factors for myositis-associated interstitial lung disease. PLoS One 9:e98824
Won Huh J, Soon Kim D, Keun Lee C, Yoo B, Bum Seo J, Kitaichi M, Colby TV (2007) Two distinct clinical types of interstitial lung disease associated with polymyositis-dermatomyositis. Respir Med 101:1761–1769
Chen IJ, Tsai WP, Wu YJ, Luo SF, Ho HH, Liou LB, Chen JY, Kuo CF, Chang HC, Yang CH, Yu KH (2010) Infections in polymyositis and dermatomyositis: analysis of 192 cases. Rheumatology (Oxford) 49:2429–2437
Chen M, Tian X, Qin F, Zhou J, Liu J, Wang M et al (2015) Pneumocystis pneumonia in patients with autoimmune diseases: a retrospective study focused on clinical characteristics and prognostic factors related to death. PLoS One 10:e0139144
Roux A, Canet E, Valade S, Gangneux-Robert F, Hamane S, Lafabrie A, Maubon D, Debourgogne A, le Gal S, Dalle F, Leterrier M, Toubas D, Pomares C, Bellanger AP, Bonhomme J, Berry A, Durand-Joly I, Magne D, Pons D, Hennequin C, Maury E, Roux P, Azoulay É (2014) Pneumocystis jirovecii pneumonia in patients with or without AIDS, France. Emerg Infect Dis 20:1490–1497
Funding
This work was supported by the Clinical Research Special Fund of Wu Jieping Medical Foundation [grant number 320.6750.18428 to Y.S.] and CAMS Innovation Fund for Medical Sciences (CIFMS) from Chinese Academy of Medical Sciences [grant number 2016-I2 M-1-014 to B.D.]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Yan Shi, Jiu-liang Zhao, Bin Du, and Jin-min Peng. The first draft of the manuscript was written by Yan Shi, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Disclosures
None.
Ethics and consent
This study has been approved by the ethics committee of Peking Union Medical College Hospital. Given the retrospective design, informed consent was waived.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 48 kb)
Rights and permissions
About this article
Cite this article
Shi, Y., Du, B., Zhao, JL. et al. Etiologies and outcomes of rheumatology patients with acute respiratory failure requiring intensive care: a single-center medical records review study of 259 patients. Clin Rheumatol 39, 3479–3488 (2020). https://doi.org/10.1007/s10067-020-05080-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05080-w