Abstract
Objectives
To explore the clinical features and associated factors of cryptococcosis in patients with connective tissue disease (CTD) from Southern China.
Methods
Demographic and clinical data were collected between 2007 and 2018. Associated factors were analyzed by logistic regression analysis.
Results
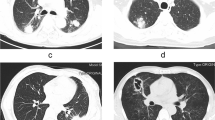
A total of 6809 inpatients with CTD were included. Cryptococcosis was diagnosed in 30 patients (prevalence, 0.4%). Cryptococcosis was predominant in patients with ANCA-associated vasculitis (AAV) (prevalence, 6/530, 1.1%). Lung was commonly involved (18/30, 60.0%), followed by meninges (6/30, 20.0%), blood stream (5/30, 16.7%), and disseminated cryptococcosis (involved blood stream and meninges) (1/30, 3.3%). Infiltrates (10/18, 55.6%) and small nodules (8/18, 44.4%) were the main radiographic manifestation of pulmonary cryptococcosis (PC). The positive rate of serum cryptococcal antigen (CrAg) in patients with PC was 88.2%. Cryptococcus spp. were found in 75% (3/4) patients who underwent lung biopsy. Most of the patients with cryptococcal meningitis (CM) had elevated cerebrospinal fluid (CSF) opening pressure (6/7, 85.7%) and decreased CSF glucose level (5/7, 71.4%). Positive blood culture confirmed the diagnosis of cryptococcal sepsis (CS). Three patients died (10.0%), including one with CM and two with PC. Multivariate logistic regression analysis showed that accumulated dose of glucocorticoid (GC) [odds ratio (OR) = 1.42, 95% confidence interval (CI) 1.04–1.93, P = 0.03] was associated with cryptococcosis in patients with CTD.
Conclusions
Cryptococcosis develops in various organs. Typical radiological manifestation accompanied with positive serum CrAg provides helpful clues for the diagnosis. Lumbar puncture is a critical diagnostic method to distinguish CM. The accumulated dose of GC is associated with cryptococcosis in patients with CTD.
Key Points • Pulmonary cryptococcosis is suspected if pulmonary nodules adjacent to the pleura are present, with serum CrAg positive. • Cryptococcal meningitis has insidious onset and the diagnosis mainly depends on lumber puncture. • Cryptococcal sepsis is not rare and needs timely blood culture in suspected patients. |


Similar content being viewed by others
References
Goldblatt F, Chambers S, Rahman A, Isenberg DA (2009) Serious infections in British patients with systemic lupus erythematosus: hospitalisations and mortality. Lupus 18:682–689. https://doi.org/10.1177/0961203308101019
Yang L, Xie H, Liu Z, Chen Y, Wang J, Zhang H, Ge Y, Hu W (2018) Risk factors for infectious complications of ANCA-associated vasculitis: a cohort study. BMC Nephrol 19:138. https://doi.org/10.1186/s12882-018-0933-2
Lao M, Wang X, Ding M, Yang Z, Chen H, Liang L, Zhan Z, Chen D (2019) Invasive fungal disease in patients with systemic lupus erythematosus from Southern China: a retrospective study. Lupus 28:77–85. https://doi.org/10.1177/0961203318817118
Lao M, Zhan Z, Su F, Li H, Yang Z, Chen H, Liang L, Chen D (2019) Invasive mycoses in patients with connective tissue disease from Southern China: clinical features and associated factors. Arthritis Res Ther 21:71. https://doi.org/10.1186/s13075-019-1851-9
Maziarz EK, Perfect JR (2016) Cryptococcosis. Infect Dis Clin N Am 30:179–206. https://doi.org/10.1016/j.idc.2015.10.006
Wang LR, Barber CE, Johnson AS, Barnabe C (2014) Invasive fungal disease in systemic lupus erythematosus: a systematic review of disease characteristics, risk factors, and prognosis. Semin Arthritis Rheum 44:325–330. https://doi.org/10.1016/j.semarthrit.2014.06.001
Fang W, Chen M, Liu J, Hagen F, Ms A, Al H, Zhang P, Guo Y, Boekhout T, Deng D, Xu J, Pan W, Liao W (2016) Cryptococcal meningitis in systemic lupus erythematosus patients: pooled analysis and systematic review. Emerg Microbes Infect 5:e95. https://doi.org/10.1038/emi.2016.93
Liao TL, Chen YM, Chen DY (2016) Risk factors for cryptococcal infection among patients with rheumatoid arthritis receiving different immunosuppressive medications. Clin Microbiol Infect 22:815.e811–815.e813. https://doi.org/10.1016/j.cmi.2016.05.030
Buchta V, Prasil P, Vejsova M, Mottl R, Kutova R, Drahosova M, Plisek S (2014) Cryptococcus neoformans meningoencephalitis in a patient with polyarteritis nodosa. Folia Microbiol (Praha) 59:515–521. https://doi.org/10.1007/s12223-014-0328-0
Iwazu K, Iwazu Y, Takeda S, Akimoto T, Yumura W, Takahashi H, Ito C, Kanai K, Taniguchi N, Hirai Y, Kusano E (2012) Successful treatment of serial opportunistic infections including disseminated nocardiosis and cryptococcal meningitis in a patient with ANCA-associated vasculitis. Intern Med 51:3051–3056. https://doi.org/10.2169/internalmedicine.51.7886
Khairullah S, Sulaiman H, Yahya F, Jasmin R, Cheah TE, Sockalingam S, Bick J, Chin Teck NG (2014) Cryptococcal meningitis and SLE: a diagnostic and therapeutic challenge. Acta Reumatol Port 39:254–258
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725. https://doi.org/10.1002/art.1780400928
Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH (1992) Derivation of the SLEDAI. A disease activity index for lupus patients. The Committee on Prognosis Studies in SLE. Arthritis Rheum 35:630–640. https://doi.org/10.1002/art.1780350606
Jennette JC, Falk RJ, Andrassy K, Bacon PA, Churg J, Gross WL, Hagen EC, Hoffman GS, Hunder GG, Kallenberg CG et al (1994) Nomenclature of systemic vasculitides. Proposal of an international consensus conference. Arthritis Rheum 37:187–192. https://doi.org/10.1002/art.1780370206
Jennette JC (2013) Overview of the 2012 revised International Chapel Hill Consensus Conference nomenclature of vasculitides. Clin Exp Nephrol 17:603–606. https://doi.org/10.1007/s10157-013-0869-6
Luqmani RA, Bacon PA, Moots RJ, Janssen BA, Pall A, Emery P, Emery P, Savage C, Adu D (1994) Birmingham Vasculitis Activity Score (BVAS) in systemic necrotizing vasculitis. QJM 87:671–678
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS et al (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324. https://doi.org/10.1002/art.1780310302
Prevoo ML, van’t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL (1995) Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 38:44–48. https://doi.org/10.1002/art.1780380107
Bohan A, Peter JB (1975) Polymyositis and dermatomyositis (first of two parts). N Engl J Med 292:344–347. https://doi.org/10.1056/nejm197502132920706
(1980) Preliminary criteria for the classification of systemic sclerosis (scleroderma). Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee. Arthritis Rheum 23:581–590. https://doi.org/10.1002/art.1780230510
Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, Daniels TE, Fox PC, Fox RI, Kassan SS, Pillemer SR, Talal N, Weisman MH (2002) Classification criteria for Sjogren’s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis 61:554–558. https://doi.org/10.1136/ard.61.6.554
Sharp GC, Irvin WS, Tan EM, Gould RG, Holman HR (1972) Mixed connective tissue disease--an apparently distinct rheumatic disease syndrome associated with a specific antibody to an extractable nuclear antigen (ENA). Am J Med 52:148–159. https://doi.org/10.1016/0002-9343(72)90064-2
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, Pappas PG, Maertens J, Lortholary O, Kauffman CA, Denning DW, Patterson TF, Maschmeyer G, Bille J, Dismukes WE, Herbrecht R, Hope WW, Kibbler CC, Kullberg BJ, Marr KA, Munoz P, Odds FC, Perfect JR, Restrepo A, Ruhnke M, Segal BH, Sobel JD, Sorrell TC, Viscoli C, Wingard JR, Zaoutis T, Bennett JE (2008) Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 46:1813–1821. https://doi.org/10.1086/588660
Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M (2001) Age Standardization of Rates: a new WHO standard. World Health Organization, Geneva
Zhong Y, Li M, Liu J, Zhang W, Peng F (2015) Cryptococcal meningitis in Chinese patients with systemic lupus erythematosus. Clin Neurol Neurosurg 131:59–63. https://doi.org/10.1016/j.clineuro.2015.01.023
Chen S, Sorrell T, Nimmo G, Speed B, Currie B, Ellis D, Marriott D, Pfeiffer T, Parr D, Byth K (2000) Epidemiology and host- and variety-dependent characteristics of infection due to Cryptococcus neoformans in Australia and New Zealand. Australasian Cryptococcal Study Group. Clin Infect Dis 31:499–508. https://doi.org/10.1086/313992
McCarthy KM, Morgan J, Wannemuehler KA, Mirza SA, Gould SM, Mhlongo N, Moeng P, Maloba BR, Crewe-Brown HH, Brandt ME, Hajjeh RA (2006) Population-based surveillance for cryptococcosis in an antiretroviral-naive South African province with a high HIV seroprevalence. AIDS 20:2199–2206. https://doi.org/10.1097/QAD.0b013e3280106d6a
Zhu LP, Wu JQ, Xu B, Ou XT, Zhang QQ, Weng XH (2010) Cryptococcal meningitis in non-HIV-infected patients in a Chinese tertiary care hospital, 1997–2007. Med Mycol 48:570–579. https://doi.org/10.3109/13693780903437876
Chen YY, Lai CH (2011) Nationwide population-based epidemiologic study of cryptococcal meningitis in Taiwan. Neuroepidemiology 36:79–84. https://doi.org/10.1159/000323390
Mitchell TG, Perfect JR (1995) Cryptococcosis in the era of AIDS--100 years after the discovery of Cryptococcus neoformans. Clin Microbiol Rev 8:515–548
Bratton EW, El Husseini N, Chastain CA, Lee MS, Poole C, Sturmer T, Juliano JJ, Weber DJ, Perfect JR (2012) Comparison and temporal trends of three groups with cryptococcosis: HIV-infected, solid organ transplant, and HIV-negative/non-transplant. PLoS One 7:e43582. https://doi.org/10.1371/journal.pone.0043582
Yu JQ, Tang KJ, Xu BL, Xie CM, Light RW (2012) Pulmonary cryptococcosis in non-AIDS patients. Braz J Infect Dis 16:531–539. https://doi.org/10.1016/j.bjid.2012.07.004
Davda S, Kowa XY, Aziz Z, Ellis S, Cheasty E, Cappocci S, Balan A (2018) The development of pulmonary aspergillosis and its histologic, clinical, and radiologic manifestations. Clin Radiol 73:913–921. https://doi.org/10.1016/j.crad.2018.06.017
Wake RM, Britz E, Sriruttan C, Rukasha I, Omar T, Spencer DC, Nel JS, Mashamaite S, Adelekan A, Chiller TM, Jarvis JN, Harrison TS, Govender NP (2018) High Cryptococcal Antigen Titers in Blood Are Predictive of Subclinical Cryptococcal Meningitis Among Human Immunodeficiency Virus-Infected Patients. Clin Infect Dis 66:686–692. https://doi.org/10.1093/cid/cix872
Sarkis RA, Mays M, Isada C, Ahmed M (2015) MRI findings in cryptococcal meningitis of the non-HIV population. Neurologist 19:40–45. https://doi.org/10.1097/NRL.0000000000000000
Li M, Chen Z, Xu L, Gan Z, Peng F, Liu J (2019) A Comparison of the Clinical Characteristics and Outcomes of Cryptococcal Meningitis in HIV-negative Individuals With and Without Immunosuppression. Neurologist 24:1–5. https://doi.org/10.1097/NRL.0000000000000221
Gonzalez-Duarte A, Saniger-Alba Mdel M, Higuera-Calleja J (2015) Cryptococcal meningitis in HIV-negative patients with systemic connective tissue diseases. Neurol Res 37:283–287. https://doi.org/10.1179/1743132814y.0000000452
Tanner DC, Weinstein MP, Fedorciw B, Joho KL, Thorpe JJ, Reller L (1994) Comparison of commercial kits for detection of cryptococcal antigen. J Clin Microbiol 32:1680–1684
Kambugu A, Meya DB, Rhein J, O’Brien M, Janoff EN, Ronald AR, Kamya MR, Mayanja-Kizza H, Sande MA, Bohjanen PR, Boulware DR (2008) Outcomes of cryptococcal meningitis in Uganda before and after the availability of highly active antiretroviral therapy. Clin Infect Dis 46:1694–1701. https://doi.org/10.1086/587667
Chen GL, Chen Y, Zhu CQ, Yang CD, Ye S (2012) Invasive fungal infection in Chinese patients with systemic lupus erythematosus. Clin Rheumatol 31:1087–1091. https://doi.org/10.1007/s10067-012-1980-x
Kim HJ, Park YJ, Kim WU, Park SH, Cho CS (2009) Invasive fungal infections in patients with systemic lupus erythematosus: experience from affiliated hospitals of Catholic University of Korea. Lupus 18:661–666. https://doi.org/10.1177/0961203309103081
Kim JM, Kim KJ, Yoon HS, Kwok SK, Ju JH, Park KS, Cho CS, Kim HY, Park SH (2011) Meningitis in Korean patients with systemic lupus erythematosus: analysis of demographics, clinical features and outcomes; experience from affiliated hospitals of the Catholic University of Korea. Lupus 20:531–536. https://doi.org/10.1177/0961203310384495
Acknowledgments
The authors would like to thank Dr. Meng Zhang for her technical assistance.
Funding
This project was supported by grants from the National Natural Science Foundation of China (81601403, 81603435), grants from the Natural Science Foundation of Guangdong Province (2018A0303130294), and grants from Guangdong Technology Project (2017A020215148).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
None.
Ethics approval
This study was approved by Institutional Review Board of the First Affiliated Hospital of Sun Yat-sen University (approval number 2019422). Written informed consent was deemed unnecessary by the Institutional Review Boards for human studies due to the retrospective nature of the data. Patients’ data were anonymized and kept confidential throughout this study. This work was conducted in compliance with the Declaration of Helsinki principles.
Availability of data and material
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The work should be attributed to: The First Affiliated Hospital of Sun Yat-sen University.
Electronic supplementary material
ESM 1
(DOCX 27 kb)
Appendix 1. ICD-10 coding for CTD and cryptococcosis
Appendix 1. ICD-10 coding for CTD and cryptococcosis
Rights and permissions
About this article
Cite this article
Lao, M., Gong, Y., Shen, C. et al. Infective patterns of cryptococcosis in patients with connective tissue disease: a retrospective study. Clin Rheumatol 39, 3071–3081 (2020). https://doi.org/10.1007/s10067-020-05068-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05068-6