Abstract
Objectives
The pro-inflammatory interleukin (IL)-17A serum has been characterized in several systemic autoimmune diseases, but not in antisynthetase syndrome (ASS). Therefore, the present study aims firstly to assess the serum level of the IL-17A in patients with ASS, comparing with healthy individuals, and secondly to analyze prospectively this IL in patients with refractory ASS undergoing rituximab treatment.
Materials and methods
A cross-sectional, single-center study that included 64 patients with ASS who were age-, gender-, and ethnicity-matched to 64 healthy individuals. Disease status was measured by the International Myositis Assessment and Clinical Studies Group (IMACS) set scores. Secondarily, the patients with refractory disease treated with rituximab were prospectively followed for 12 months. The IL-17A was assessed by the ELISA method.
Results
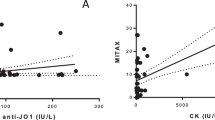
The mean age of the patients was 44.8 ± 11.8 years, with a predominance of female gender and Caucasian. The median serum IL-17A level was higher in ASS patients compared with healthy individuals: 9.7 (9.1–10.4) vs. 7.7 (5.7–9.0) pg/mL, respectively, and P < 0.001. However, the demographical, clinical, and laboratory data indicates that disease status did not correlate with serum levels of the IL-17A in ASS patients. Prospectively, 16 patients received rituximab, and there was a drop of IL-17A serum level over the first year of treatment in these patients: from 9.7 (9.1–10.6) to 9.0 (8.2–9.7) pg/mL (P = 0.01).
Conclusions
Our study demonstrated that patients with ASS have increased serum levels of the IL-17A compared with healthy controls. In addition, the patients with refractory ASS treated with rituximab showed a reduction of the serum levels of the IL-17A.
Key Points | |
• Patients with ASS have increased serum levels of the IL-17A. | |
• Patients with refractory ASS treated with rituximab showed a reduction of the serum levels of the IL-17A. |

Similar content being viewed by others
References
Gallay L, Gayed C, Hervier B (2018) Antisynthetase syndrome pathogenesis: knowledge and uncertainties. Curr Opin Rheumatol 30:664–673
Araujo PAO, Silva MG, Borba EF, Shinjo SK (2018) High prevalence of metabolic syndrome in antisynthetase syndrome. Clin Exp Rheumatol 36:241–247
Connors GR, Christopher-Stine L, Oddis CV, Danoff SK (2010) Interstitial lung disease associated with the idiopathic inflammatory myopathies: what progress has been made in the past 35 years? Chest 138:1464–1474
Lega JC, Fabien N, Reynaud Q, Durieu I, Durupt S, Dutertre M, Cordier JF, Cottin V (2014) The clinical phenotype associated with myositis-specific and associated autoantibodies: a meta-analysis revisiting the so-called antisynthetase syndrome. Autoimmun Rev 13:883–891
Roşu A, Mǎrgǎritescu C, Stepan A, Muşetescu A, Ene M (2012) IL-17 patterns in synovium, serum and synovial fluid from treatment-naïve, early rheumatoid arthritis patients. Romanian J Morphol Embryol 53:73–80
Iwakura Y, Ishigame H, Saijo S, Nakae S (2011) Functional specialization of interleukin-17 family members. Immunity 34:149–162
Monin L, Gaffen SL (2018) Interleukin 17 family cytokines: signaling and therapeutic implications. Cold Spring Harb Perspect Biol 10:A028522
Mitsdoerffer M, Lee Y, Jäger A, Kim HJ, Korn T, Kolls JK et al (2010) Pro-inflammatory T helper type 17 cells are effective B-cell helpers. Proc Natl Acad Sci U S A 107:14292–14297
Reed AM, Crowson CS, Hein M, De Padilla CL, Olazagasti JM, Aggarwal R et al (2015) Biologic predictors of clinical improvement in rituximab-treated refractory myositis clinical rheumatology and osteoporosis. BMC Musculoskelet Disord 16:257
Van De Veerdonk FL, Lauwerys B, Marijnissen RJ, Timmermans K, DI Padova F, Koenders MI et al (2011) The anti-CD20 antibody rituximab reduces the Th17 cell response. Arthritis Rheum 63:1507–1516
Alunno A, Carubbi F, Bistoni O, Caterbi S, Bartoloni E, Di Benedetto P et al (2016) Interleukin (IL)-17-producing pathogenic T lymphocytes co-express CD20 and are depleted by rituximab in primary Sjögren’s syndrome: a pilot study. Clin Exp Immunol 184:284–292
Tabarkiewicz J, Pogoda K, Karczmarczyk A, Pozarowski P, Giannopoulos K (2015) The role of IL-17 and Th17 lymphocytes in autoimmune diseases. Arch Immunol Ther Exp 63:435–449
Chen XQ, Yu YC, Deng HH, Sun JZ, Dai Z, Wu YW et al (2010) Plasma IL-17A is increased in new-onset SLE patients and associated with disease activity. J Clin Immunol 30:221–225
Zhang LW, Zhou PR, Wei P, Cong X, Wu LL, Hua H (2018) Expression of interleukin-17 in primary Sjögren’s syndrome and the correlation with disease severity: a systematic review and meta-analysis. Scand J Immunol 87:e12649
Silva MG, Oba-Shinjo SM, Marie SKN, Shinjo SK (2018) Serum interleukin-17A level is associated with disease activity of adult patients with dermatomyositis and polymyositis. Clin Exp Rheumatol 37:656–662
Notarnicola A, Lapadula G, Natuzzi D, Lundberg IE, Iannone F (2015) Correlation between serum levels of IL-15 and IL-17 in patients with idiopathic inflammatory myopathies. Scand J Rheumatol 44:224–228
Tournadre A, Miossec P (2012) Interleukin-17 in inflammatory myopathies. Curr Rheumatol Rep 14:252–256
Shen H, Xia L, Lu J, Xiao W (2011) Interleukin-17 and interleukin-23 in patients with polymyositis and dermatomyositis. Scand J Rheumatol 40:217–220
Moran EM, Mastaglia FL (2014) The role of interleukin-17 in immune-mediated inflammatory myopathies and possible therapeutic implications. Neuromuscul Disord 24:943–952
Chevrel G, Page G, Granet C, Streichenberger N, Varennes A, Miossec P (2003) Interleukin-17 increases the effects of IL-1 h on muscle cells : arguments for the role of T cells in the pathogenesis of myositis. J Neuro-Oncol 137:125–133
Rider LG, Aggarwal R, Pistorio A, Bayat N, Erman B, Feldman BM, Huber AM, Cimaz R, Cuttica RJ, de Oliveira SK, Lindsley CB, Pilkington CA, Punaro M, Ravelli A, Reed AM, Rouster-Stevens K, van Royen-Kerkhof A, Dressler F, Saad Magalhaes C, Constantin T, Davidson JE, Magnusson B, Russo R, Villa L, Rinaldi M, Rockette H, Lachenbruch PA, Miller FW, Vencovsky J, Ruperto N, International Myositis Assessment and Clinical Studies Group and the Paediatric Rheumatology International Trials Organisation (2017) 2016 American College of Rheumatology/European League against rheumatism criteria for minimal, moderate, and major clinical response in juvenile dermatomyositis. Ann Rheum Dis 76:782–791
Rider LLG, Koziol D, Giannini EEH, Jain MS, Smith MR, Whitney-Mahoney K, Feldman BM, Wright SJ, Lindsley CB, Pachman LM, Villalba ML, Lovell DJ, Bowyer SL, Plotz PH, Miller FW, Hicks JE (2010) Validation of manual muscle testing and a subset of eight muscles for adult and juvenile idiopathic inflammatory myopathies. Arthritis Care Res 62:465–472
Bruce B, Fries JF (2003) The Stanford health assessment questionnaire: dimensions and practical applications. Health Qual Life Outcomes 1:1–6
Miller FW, Rider LG, Chung YL, Cooper R, Danko K, Farewell V et al (2001) Proposed preliminary core set measures for disease outcome assessment in adult and juvenile idiopathic inflammatory myopathies. Rheumatology 40:1462–1473
Cruellas MG, Dos Santos VV, Levy-Neto M, Souza FHC, Shinjo SK (2013) Myositis-specific and myositis-associated autoantibody profiles and their clinical associations in a large series of patients with polymyositis and dermatomyositis. Clinics 68:909–914
Souza FHC, Araújo DB, Vilela VS, Bezerra MC, Simões RS, Bernardo WM et al (2019) Guidelines of the Brazilian Society of Rheumatology for the treatment of systemic autoimmune myopathies. Adv Rheumatol 59:6
Dugar M, Cox S, Limaye V, Blumbergs P, Roberts-Thomson PJ (2011) Clinical heterogeneity and prognostic features of South Australian patients with anti-synthetase autoantibodies. Intern Med J 41:674–679
Shi J, Li S, Yang H, Zhang Y, Peng Q, Lu X et al (2017) Clinical profiles and prognosis of patients with distinct antisynthetase autoantibodies. J Rheumatol 44:1051–1057
Pinal-Fernandez I, Casal-Dominguez M, Huapaya JA, Albayda J, Paik JJ, Johnson C et al (2017) A longitudinal cohort study of the anti-synthetase syndrome: increased severity of interstitial lung disease in black patients and patients with anti-PL7 and anti-PL12 autoantibodies. Rheumatology (Oxford) 56:999–1007
Souza FHC, Cruellas MGP, Levy-Neto M, Shinjo SK (2013) Síndrome antissintetase: Anti-PL-7, anti-PL-12 and anti-EJ. Rev Bras Reumatol 53:352–357
Hervier B, Benveniste O (2013) Clinical heterogeneity and outcomes of antisynthetase syndrome. Curr Rheumatol Rep 15:349
Mahler M, Miller FW, Fritzler MJ (2014) Idiopathic inflammatory myopathies and the anti-synthetase syndrome: a comprehensive review. Autoimmun Rev 13:367–371
Sem M, Molber Ø, Lund MB, Gran JT (2009) Rituximab treatment of the anti-synthetase syndrome - a retrospective case series. Rheumatology 48:968–971
Souza FHC, Miossi R, De Moraes JCB, Bonfá E, Shinjo SK (2018) Favorable rituximab response in patients with refractory idiopathic inflammatory myopathies. Adv Rheumatol 58:31
Vigna-Perez M, Hernández-Castro B, Paredes-Saharopulos O, Portales-Pérez D, Baranda L, Abud-Mendoza C et al (2006) Clinical and immunological effects of rituximab in patients with lupus nephritis refractory to conventional therapy: a pilot study. Arthritis Res Ther 8:R83
Funding
This study is funded by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) (#2014/09079-1), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (#303379/2018-9), and Faculdade de Medicina da USP–SP to SKS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Behrens Pinto, G.L., Carboni, R.C.d., de Souza, F.H.C. et al. A prospective cross-sectional study of serum IL-17A in antisynthetase syndrome. Clin Rheumatol 39, 2763–2771 (2020). https://doi.org/10.1007/s10067-020-05013-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05013-7