Abstract
Introduction
The risk factors for systemic autoimmune diseases (SAD) in gastric disease patients with proton pump inhibitor (PPI) use are still unclear. This study discussed this relationship in an Asian population.
Methods
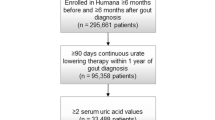
Patients without a prior history of SAD were identified from Taiwan’s National Health Insurance Research Database between January 1, 2000, and December 31, 2010. Cox regression models were applied to estimate the hazard ratio (HR) with 95% confidence interval [CI] of SAD. The cumulative PPI dosage was stratified by quartiles of defined daily doses and adjusted for baseline disease risk score which served as the primary variables compared against no PPI use.
Results
We analyzed the data of 51,291 participants aged 18 years or older and free of SAD at baseline. PPI users (n = 17,938) had a significantly increased risk of SAD over non-PPI users. There was a significantly higher risk of developing SAD in older age groups. A significant dose-dependent association was observed between cumulative PPI use and the risk of SAD. Female PPI users had significantly higher risk of developing SAD. In patients who received PPI, the autoimmune disease with significantly higher incidence was Sjögren syndrome (SjS) (adjusted HR [aHR] 1.82, 95% CI, 1.02–3.27) and rheumatoid arthritis (RA) (aHR, 2.19, 95% CI, 1.19–4.01).
Conclusion
This study found PPI users to be associated with an increased risk of SAD. Older age or cumulative PPI use was significantly associated with SAD, and the highest incidence was SjS and RA among gastric disease patients who received PPI.
Key Points • This nationwide long-term cohort study found PPI users to be associated with an increased risk of rheumatoid arthritis and Sjögren syndrome in Taiwan. • This finding may help with clinical risk evaluation and will inform further investigation of the pathogenesis between autoimmune diseases and PPI use. |



Similar content being viewed by others
References
Lerner A, Jeremias P, Matthias T (2015) The world incidence and prevalence of autoimmune diseases is increasing. IJCD 3(4):151–155. http://pubs.sciepub.com/ijcd/3/4/8/
Male D, Brostoff J, Roth D, Roitt I (2013) Immunology, 8th edn. Elsevier Ltd, Philadelphia, pp 323–327
Jakes RW, Bae SC, Louthrenoo W, Mok CC, Navarra SV, Kwon N (2012) Systematic review of the epidemiology of systemic lupus erythematosus in the Asia-Pacific region: prevalence, incidence, clinical features, and mortality. Arthritis Care Res 64(2):159–168. https://onlinelibrary.wiley.com/doi/full/10.1002/acr.20683
Xiao X, Chang C (2014) Diagnosis and classification of drug-induced autoimmunity. J Autoimmun 48-49:66–72. https://www.sciencedirect.com/science/article/pii/S0896841114000079?Via%3Dihub
Hollingworth S, Duncan EL, Martin JH (2010) Marked increase in proton pump inhibitors use in Australia. Pharmacoepidemiol Drug Saf 19:1019–1024. https://onlinelibrary.wiley.com/doi/abs/10.1002/pds.1969
Forgacs I, Loganayagam A (2008) Overprescribing proton pump inhibitors. BMJ 336:2–3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2174763/
Yu C, Gershwin ME, Chang C (2014) Diagnostic criteria for systemic lupus erythematosus: a critical review. J Autoimmun 48–49:10–13. https://www.sciencedirect.com/science/article/pii/S0896841114000067?via%3Dihub
Sandholdt LH, Laurinaviciene R, Bygum A (2014) Proton pump inhibitor-induced subacute cutaneous lupus erythematosus. Br J Dermatol 170(1):342–351. https://onlinelibrary.wiley.com/doi/full/10.1111/bjd.12699
Rubin RL (2005) Drug-induced lupus. Toxicology 209(2):135–147. https://www.sciencedirect.com/science/article/pii/S0300483X04007279?via%3Dihub
Biswas S, Benedict SH, Lynch SG, LeVine SM (2012) Potential immunological consequences of pharmacological suppression of gastric acid production in patients with multiple sclerosis. BMC Med 7:10–57. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3386885/
WHO Collaborating Centre for Drug Statistics Methodology. Defined daily dose: definition and general considerations [Internet]. 29 July 2014. https://www.who.int/medicines/regulation/medicines-safety/toolkit_ddd/en/
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Manfredo Vieira S, Hiltensperger M, Kumar V, Zegarra-Ruiz D, Dehner C, Khan N, Costa FRC, Tiniakou E, Greiling T, Ruff W, Barbieri A, Kriegel C, Mehta SS, Knight JR, Jain D, Goodman AL, Kriegel MA (2018) Translocation of a gut pathobiont drives autoimmunity in mice and humans. Science 359(6380):1156–1161. https://science.sciencemag.org/content/359/6380/1156.long
Imhann F, Bonder MJ, Vich Vila A, Fu J, Mujagic Z, Vork L, Tigchelaar EF, Jankipersadsing SA, Cenit MC, Harmsen HJ, Dijkstra G, Franke L, Xavier RJ, Jonkers D, Wijmenga C, Weersma RK, Zhernakova A (2016) Proton pump inhibitors affect the gut microbiome. Gut 65(5):740–748. https://gut.bmj.com/content/65/5/740.long
van der Meulen TA, Harmsen HJM, Vila AV, Kurilshikov A, Liefers SC, Zhernakova A, Fu J, Wijmenga C, Weersma RK, de Leeuw K, Bootsma H, Spijkervet FKL, Vissink A, Kroese FGM (2019) Shared gut, but distinct oral microbiota composition in primary Sjögren’s syndrome and systemic lupus erythematosus. J Autoimmun 97:77–87. https://www.sciencedirect.com/science/article/pii/S0896841118305249?via%3Dihub
Wallace JL, Syer S, Denou E, de Palma G, Vong L, McKnight W, Jury J, Bolla M, Bercik P, Collins SM, Verdu E, Ongini E (2011) Proton pump inhibitors exacerbate NSAID-induced small intestinal injury by inducing dysbiosis. Gastroenterology 141:1314–1322. https://www.gastrojournal.org/article/S0016-5085(11)00926-7/fulltext?referrer=https%3A%2F%2Fwww.ncbi.nlm.nih.gov%2F
Rose NR, Bona C (1993) Defining criteria for autoimmune diseases (Witebsky’s postulates revisited). Immunol Today 14(9):426–430. https://www.sciencedirect.com/science/article/pii/016756999390244F?via%3Dihub
Hayter SM, Cook MC (2012) Updated assessment of the prevalence, spectrum and case definition of autoimmune disease. Autoimmun Rev 11(10):754–765. https://www.sciencedirect.com/science/article/abs/pii/S1568997212000225?via%3Dihub
Eriksson JK, Neovius M, Ernestam S, Lindblad S, Simard JF, Askling J (2013) Incidence of rheumatoid arthritis in Sweden: a nationwide population-based assessment of incidence, its determinants, and treatment penetration. Arthritis Care Res 65(6):870–878. https://onlinelibrary.wiley.com/doi/full/10.1002/acr.21900
Rubtsova K, Marrack P, Rubtsov AV (2015) Sexual dimorphism in autoimmunity. J Clin Invest 125(6):2187–2193. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4497744/
Helmick CG, Felson DT, Lawrence RC, Gabriel S, Hirsch R, Kwoh CK, Liang MH, Kremers HM, Mayes MD, Merkel PA, Pillemer SR, Reveille JD, Stone JH, Workgroup NAD (2008) Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I Arthritis Rheum 58(1):15–25. https://onlinelibrary.wiley.com/doi/full/10.1002/art.23177
Jarukitsopa S, Hoganson DD, Crowson CS, Sokumbi O, Davis MD, Michet CJ Jr, Matteson EL, Maradit Kremers H, Chowdhary VR (2015) Epidemiology of systemic lupus erythematosus and cutaneous lupus erythematosus in a predominantly white population in the United States. Arthritis Care Res 67(6):817–828. https://onlinelibrary.wiley.com/doi/full/10.1002/acr.22502
Hui M, Zhao J, Tian Z, Wang J, Qian J, Yang X, Wang Q, Li M, Zhao Y, Zeng X (2019) Red blood cell distribution width as a potential predictor of survival of pulmonary arterial hypertension associated with primary Sjogren’s syndrome: a retrospective cohort study. Clin Rheumatol 38(2):477–485. https://link.springer.com/article/10.1007%2Fs10067-018-4281-1
Aggarwal N (2016) Drug-induced subacute cutaneous lupus erythematosus associated with proton pump inhibitors. Drugs Real World Outcomes 3(2):145–154. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4914530/
Okon LG, Werth VP (2013) Cutaneous lupus erythematosus: diagnosis and treatment. Best Pract Res Clin Rheumatol 27(3):391–404. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3927537/
Gilkeson GS, James JA, Kamen DL, Knackstedt T, Maggi D, Meyer A, Ruth N (2011) The United States to Africa lupus prevalence gradient revisited. Lupus 20(10):1095–1103. https://journals.sagepub.com/doi/abs/10.1177/0961203311404915?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=lupa
Funding
This study is supported in part by the Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW108-TDU-B-212-133004); China Medical University Hospital, Academia Sinica Stroke Biosignature Project (BM10701010021); MOST Clinical Trial Consortium for Stroke (MOST 108-2321-B-039-003-); Tseng-Lien Lin Foundation, Taichung, Taiwan; and Katsuzo and Kiyo Aoshima Memorial Funds, Japan.
Author information
Authors and Affiliations
Contributions
Jiun-Jie Lin: revising the protocol for content and clarity; conception of the initial review; drafting the protocol; literature search; selecting, reading, and comparing titles, abstracts, and papers; drafting a data extraction sheet; data extraction; drafting the first review; reading and correcting the full review; and final approval.
Hung-Yi Chen and Bo Yang: building a database for data extraction, drafting a data extraction sheet, drafting the update review, and final approval.
Mei-Chen Lin and Management Office for health data Workgroup: data extraction and statistical analyses.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the China Medical University and China Medical University Hospital, Taiwan (CMUH104-REC2-115(CR-2)).
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, HY., Lin, JJ., Yang, B. et al. Risk of systemic autoimmune diseases in gastric disease patients with proton pump inhibitor use: a nationwide cohort study in Taiwan. Clin Rheumatol 39, 2773–2780 (2020). https://doi.org/10.1007/s10067-020-05012-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05012-8