Abstract
Raynaud’s phenomenon (RP) is used to describe a symptom complex caused by digital vascular compromise. RP is a clinical diagnosis. The typically episodic nature of RP has resulted in a reliance upon patient self-report for diagnosis. The term ‘primary RP’ is generally applied when no underlying pathology can be demonstrated. Whilst ‘primary RP’ is currently considered a distinct disorder, there is evidence that the term may comprise several entities that include a functional vasospastic disorder, a physiologically appropriate thermoregulatory response, subclinical atherosclerosis and ‘cold intolerance’. Optimal management may differ depending on cause. The term ‘secondary RP’ encompasses a broad range of rheumatological, haematological, endocrinological and vascular pathology. RP can range from relatively benign but intrusive vasospasm, to the progressive obliterative microangiopathy of systemic sclerosis (SSc), in which severe digital ischaemia can threaten tissue viability. SSc has formed the focus of much of the research into RP but, consistent with most medical symptom complexes, the aetiopathogenesis of RP varies greatly dependent on cause. Vasospasm within the digital macro- and microvasculature occurs in SSc, but digital ischaemia is further compounded by a progressive obliterative microangiopathy. Recent work exploring the patient experience of SSc-RP is challenging the ‘episodic’ paradigm of ‘Raynaud’s’, with important implications for clinical trials utilising diary-based patient-reported outcome instruments for assessing Raynaud’s symptoms. This review shall examine the causes, pathogenesis, clinical features, classification and management of RP. A practical approach to the evaluation and management of RP is outlined, highlighting important knowledge gaps and unmet research needs where applicable.
Key Points • Raynaud’s phenomenon is a symptom complex related to digital vascular compromise secondary to broad-ranging pathology. • Raynaud’s phenomenon, as currently classified, likely encompasses a number of aetiopathogenic processes. • Raynaud’s phenomenon causes significant disease-related morbidity in autoimmune rheumatic diseases such as systemic sclerosis. |




Similar content being viewed by others
References
Gasparyan AY, Ayvazyan L, Blackmore H, Kitas GD (2011) Writing a narrative biomedical review: considerations for authors, peer reviewers, and editors. Rheumatol Int 31:1409–1417
Barlow T (1862 and 1874). On local asphyxia and symmetrical gangrene of the extremities, and new research on the nature and treatment of local asphyxia of the extremities. Selected monographs. London: New Sydenham Society
Allen E, Brown G (1932) Raynaud’s disease: a critical review of minimal requisites for diagnosis. Am J M Sc 183:187–200
Maverakis E, Patel F, Kronenberg DG, Chung L, Fiorentino D, Allanore Y, Guiducci S, Hesselstrand R, Hummers LK, Duong C, Kahaleh B, Macgregor A, Matucci-Cerinic M, Wollheim FA, Mayes MD, Gershwin ME (2014) International consensus criteria for the diagnosis of Raynaud’s phenomenon. J Autoimmun 48-49:60–65
Maricq HR, Carpentier PH, Weinrich MC, Keil JE, Palesch Y, Biro C et al (1997) Geographic variation in the prevalence of Raynaud’s phenomenon: a 5 region comparison. J Rheumatol 24:879–889
LeRoy EC, Medsger TA (1992) Raynaud’s phenomenon: a proposal for classification. Clin Exp Rheumatol 10:485–488
Brennan P, Silman A, Black C, Bernstein R, Coppock J, Maddison P, et al. (1993) Validity and reliability of three methods used in the diagnosis of Raynaud’s phenomenon. The UK Scleroderma Study Group. Br J Rheumatol 32:357–361
Garner R, Kumari R, Lanyon P, Doherty M, Zhang W (2015) Prevalence, risk factors and associations of primary Raynaud’s phenomenon: systematic review and meta-analysis of observational studies. BMJ Open 5:e006389–e006389
Hutchinson J (1901) Raynaud’s phenomenon. Med Press Circ 128:403–405
Hadler N (1998) “Primary Raynaud’s” is not a disease or even a disorder; it’s a trait. J Rheumatol 25:2291–2294
Allen E, Brown G (1932) Raynaud’s disease: a clinical study of one hundred and forty-seven cases. J Am Med Assoc 99:1472–1478
Bayle O, Consoli SM, Baudin M, Vayssairat M, Fiessinger JN, Housset E (1990) Idiopathic and secondary Raynaud’s phenomenon. A comparative psychosomatic approach. Presse Med 19:741–745
Vaerøy H, Helle R, Førre O, Kåss E, Terenius L (1998) Elevated CSF levels of substance P and high incidence of Raynaud phenomenon in patients with fibromyalgia: new features for diagnosis. Pain 32:21–26
Wolfe F, Petri M, Alarcon G, Goldman J, Chakravarty E, Katz R et al (2009) Fibromyalgia, systemic lupus erythematosus (SLE), and evaluation of SLE activity. J Rheumatol 36:82–88
Scolnik M, Vasta B, Hart DJ, Shipley JA, McHugh NJ, Pauling JD (2016) Symptoms of Raynaud’s phenomenon (RP) in fibromyalgia syndrome are similar to those reported in primary RP despite differences in objective assessment of digital microvascular function and morphology. Rheumatol Int 36:1371–1377
Nietert PJ, Shaftman SR, Silver RM, Wolf BJ, Egan BM, Hunt KJ, Smith EA (2015) Raynaud phenomenon and mortality: 20+ years of follow-up of the Charleston Heart Study cohort. Clin Epidemiol 7:161–168
Pizzorni C, Sulli A, Smith V, Ruaro B, Trombetta AC, Cutolo M, Paolino S (2017) Primary Raynaud’s phenomenon and nailfold videocapillaroscopy: age-related changes in capillary morphology. Clin Rheumatol 36:1637–1642
Spencer-Green G (1998) Outcomes in primary Raynaud phenomenon: a meta-analysis of the frequency, rates, and predictors of transition to secondary diseases. Arch Intern Med 158:595–600
Walker UA, Tyndall A, Czirják L, Denton C, Farge-Bancel D, Kowal-Bielecka O et al (2007) Clinical risk assessment of organ manifestations in systemic sclerosis: a report from the EULAR scleroderma trials and research group database. Ann Rheum Dis 2007:754–763
Delisle VC, Hudson M, Baron M, Thombs BD, And The Canadian Scleroderma Research Group A (2014) Sex and time to diagnosis in systemic sclerosis: an updated analysis of 1,129 patients from the Canadian scleroderma research group registry. Clin Exp Rheumatol 32:S-10–S-14
Koenig M, Joyal F, Fritzler MJ, Roussin A, Abrahamowicz M, Boire G, Goulet JR, Rich É, Grodzicky T, Raymond Y, Senécal JL (2008) Autoantibodies and microvascular damage are independent predictive factors for the progression of Raynaud’s phenomenon to systemic sclerosis: a twenty-year prospective study of 586 patients, with validation of proposed criteria for early systemic sclerosis. Arthritis Rheum 58:3902–3912
Schneeberger D, Tyndall A, Kay J, Søndergaard KH, Carreira PE, Morgiel E et al (2012) Systemic sclerosis without antinuclear antibodies or Raynaud’s phenomenon: a multicentre study in the prospective EULAR Scleroderma Trials and Research (EUSTAR) database. Rheumatology (Oxford) 52:560–567
Fiorentino DF, Kuo K, Chung L, Zaba L, Li S, Casciola-Rosen L (2015) Distinctive cutaneous and systemic features associated with antitranscriptional intermediary factor-1γ antibodies in adults with dermatomyositis. J Am Acad Dermatol 72:449–455
Carpintero MF, Martinez L, Fernandez I, Romero ACG, Mejia C, Zang YJ, Hoffman RW, Greidinger EL (2015) Diagnosis and risk stratification in patients with anti-RNP autoimmunity. Lupus 24:1057–1066
Arroyo-Ávila M, Santiago-Casas Y, McGwin G, Cantor RS, Petri M, Ramsey-Goldman R, Reveille JD, Kimberly RP, Alarcón GS, Vilá LM, Brown EE (2015) Clinical associations of anti-Smith antibodies in PROFILE: a multi-ethnic lupus cohort. Clin Rheumatol 34:1217–1223
Nakano M, Ohuchi Y, Hasegawa H, Kuroda T, Ito S, Gejyo F (2000) Clinical significance of anticentromere antibodies in patients with systemic lupus erythematosus. J Rheumatol 27:1403–1407
Kuramoto N, Ohmura K, Ikari K, Yano K, Furu M, Yamakawa N, Hashimoto M, Ito H, Fujii T, Murakami K, Nakashima R, Imura Y, Yukawa N, Yoshifuji H, Taniguchi A, Momohara S, Yamanaka H, Matsuda F, Mimori T, Terao C (2017) Anti-centromere antibody exhibits specific distribution levels among anti-nuclear antibodies and may characterize a distinct subset in rheumatoid arthritis. Sci Rep 7:6911
Lee K-E, Kang J-H, Lee J-W, Wen L, Park D-J, Kim T-J, Park YW, Lee SS (2015) Anti-centromere antibody-positive Sjögren’s syndrome: a distinct clinical subgroup? Int J Rheum Dis 18:776–782
Tsukamoto M, Suzuki K, Takeuchi T (2018) Clinical and immunological features of anti-centromere antibody-positive primary Sjögren’s syndrome. Rheumatol Ther 5:499–505
Hebbar M, Lassalle P, Delneste Y, Hatron PY, Devulder B, Tonnel AB, Janin A (1997) Assessment of anti-endothelial cell antibodies in systemic sclerosis and Sjögren’s syndrome. Ann Rheum Dis 56:230–234
Li M-T, Ai J, Tian Z, Fang Q, Zheng W-J, Zeng X-J, Zeng XF (2010) Prevalence of anti-endothelial cell antibodies in patients with pulmonary arterial hypertension associated with connective tissue diseases. Chin Med Sci J 25:27–31
Riemekasten G, Philippe A, Näther M, Slowinski T, Müller DN, Heidecke H et al (2011) Involvement of functional autoantibodies against vascular receptors in systemic sclerosis. Ann Rheum Dis 70:530–536
Shah AA, Montagne J, Oh S-Y, Wigley FM, Casciola-Rosen L (2015) Pilot study to determine whether transient receptor potential melastatin type 8 (TRPM8) antibodies are detected in scleroderma. Clin Exp Rheumatol 33:S123–S126
Maricq HR, Weinrich MC (1998) Diagnosis of Raynaud’s phenomenon assisted by color charts. J Rheumatol 15:454–459
Wollersheim H, Thien T (1990) The diagnostic value of clinical signs and symptoms in patients with Raynaud’s phenomenon. A cross-sectional study. Neth J Med 37:171–182
Ingegnoli F, Gualtierotti R, Orenti A, Schioppo T, Marfia G, Campanella R et al (2015) Uniphasic blanching of the fingers, abnormal capillaroscopy in nonsymptomatic digits, and autoantibodies: expanding options to increase the level of suspicion of connective tissue diseases beyond the classification of Raynaud’s phenomenon. J Immunol Res 2015:371960
Pauling JD, Reilly E, Smith T, Frech TM. Evolving symptoms of Raynaud’s phenomenon in systemic sclerosis are associated with physician and patient-reported assessments of disease severity. Arthritis Care Res (Hoboken) 2018. doi:https://doi.org/10.1002/acr.23729.
Pauling JD, Domsic RT, Saketkoo LA, Almeida C, Withey J, Jay H, Frech TM, Ingegnoli F, Dures E, Robson J, McHugh NJ, Herrick AL, Matucci-Cerinic M, Khanna D, Hewlett S (2018) A multi-national qualitative research study exploring the patient experience of Raynaud’s phenomenon in systemic sclerosis. Arthritis Care Res 70:1373–1384
Pauling JD, Saketkoo LA, Domsic RT (2018) Patient perceptions of the Raynaud’s condition score diary provide insight into its performance in clinical trials of Raynaud’s phenomenon: comment on the article by Denton et al. Arthritis Rheum 70:973–974
Pauling JD, Saketkoo LA, Matucci-Cerinic M, Ingegnoli F, Khanna D (2019) The patient experience of Raynaud’s phenomenon in systemic sclerosis. Rheumatology (Oxford) 58:18–26
Pauling JD, Frech TM, Hughes M, Gordon JK, Domsic RT, Anderson ME, Ingegnoli F, McHugh NJ, Johnson SR, Hudson M, Boin F, Ong VH, Matucci-Cerinic M, Altorok N, Scolnik M, Nikpour M, Shah A, Pope JE, Khanna D, Herrick AL (2018) Patient-reported outcome instruments for assessing Raynaud’s phenomenon in systemic sclerosis: a SCTC vascular working group report. J Scleroderma Relat Disord 3:249–252
Pauling JD, Shipley JA, Hart DJ, McGrogan A, McHugh NJ (2015) Use of laser speckle contrast imaging to assess digital microvascular function in primary Raynaud phenomenon and systemic sclerosis: a comparison using the Raynaud condition score diary. J Rheumatol 42:1163–1168
Wilkinson JD, Leggett SA, Marjanovic EJ, Moore TL, Allen J, Anderson ME, Britton J, Buch MH, del Galdo F, Denton CP, Dinsdale G, Griffiths B, Hall F, Howell K, MacDonald A, McHugh NJ, Manning JB, Pauling JD, Roberts C, Shipley JA, Herrick AL, Murray AK (2018) A multicenter study of the validity and reliability of responses to hand cold challenge as measured by laser speckle contrast imaging and thermography: outcome measures for systemic sclerosis-related Raynaud’s phenomenon. Arthritis Rheum 70:903–911
Pauling JD, Reilly EE, Smith T, Frech TM (2019) Factors influencing Raynaud’s condition score diary outcomes in systemic sclerosis. J Rheumatol. https://doi.org/10.3899/jrheum.180818
Hughes M, Snapir A, Wilkinson J, Snapir D, Wigley FM, Herrick AL (2015) Prediction and impact of attacks of Raynaud’s phenomenon, as judged by patient perception. Rheumatol 54:1443–1447
Watson HR, Robb R, Belcher G, Belch JJ (1999) Seasonal variation of Raynaud’s phenomenon secondary to systemic sclerosis. J Rheumatol 26:1734–1737
Freedman RR, Ianni P (1983) Role of cold and emotional stress in Raynaud’s disease and scleroderma. Br Med J (Clin Res Ed) 287:1499–1502
Sandqvist G, Wollmer P, Scheja A, Wildt M, Hesselstrand R (2018) Raynaud’s phenomenon and its impact on activities in daily life during one year of follow-up in early systemic sclerosis. Scand J Rheumatol 47:206–209
Pauling J, Nagaraja V, Khanna D Insight into the contrasting findings of therapeutic trials of digital ischaemic manifestations of systemic sclerosis. Curr Treat Opinions in Rheum 5:85–103
Chikura B, Moore T, Manning J, Vail A, Herrick AL (2010) Thumb involvement in Raynaud’s phenomenon as an indicator of underlying connective tissue disease. J Rheumatol 37:783–786
Bassel M, Hudson M, Taillefer SS, Schieir O, Baron M, Thombs BD (2011) Frequency and impact of symptoms experienced by patients with systemic sclerosis: results from a Canadian National Survey. Rheumatology (Oxford) 50:762–767
Frantz C, Avouac J, Distler O, Amrouche F, Godard D, Kennedy AT, Connolly K, Varga J, Matucci-Cerinic M, Allanore Y (2016) Impaired quality of life in systemic sclerosis and patient perception of the disease: a large international survey. Semin Arthritis Rheum 46:115–123
Kwakkenbos L, Sanchez TA, Turner KA, Mouthon L, Carrier M-E, Hudson M et al (2018) The association of sociodemographic and disease variables with hand function: a scleroderma patient-centered intervention network cohort study. Clin Exp Rheumatol 36:88–94
Merkel PA, Herlyn K, Martin RW, Anderson JJ, Mayes MD, Bell P, Korn JH, Simms RW, Csuka ME, Medsger TA Jr, Rothfield NF, Ellman MH, Collier DH, Weinstein A, Furst DE, Jiménez SA, White B, Seibold JR, Wigley FM, for the Scleroderma Clinical Trials Consortium (2002) Measuring disease activity and functional status in patients with scleroderma and Raynaud’s phenomenon. Arthritis Rheum 46:2410–2420
Herrick AL (2012) The pathogenesis, diagnosis and treatment of Raynaud phenomenon. Nat Rev Rheumatol 8:469–479
Giurgea G-A, Mlekusch W, Charwat-Resl S, Mueller M, Hammer A, Gschwandtner ME et al (2015) Relationship of age and body mass index to skin temperature and skin perfusion in primary Raynaud’s phenomenon. Arthritis Rheumatol (Hoboken, NJ) 67:238–242
Munir S, Freidin MB, Brain S, Williams FMK (2018) Association of Raynaud’s phenomenon with a polymorphism in the NOS1 gene. PLoS One 2018;13:e0196279
Wigley FM (2002) Raynaud’s phenomenon. N Engl J Med 347:1001–1008
Hughes M, Baker A, Farrington S, Pauling JD (2019) Patient organisation-led initiatives can play an important role in raising awareness about Raynaud’s phenomenon and encourage earlier healthcare utilisation for high-risk groups. Ann Rheum Dis 78:439–441
Freedman RR, Mayes MD (1996) Familial aggregation of primary Raynaud’s disease. Arthritis Rheum 39:1189–1191
Frech T, Khanna D, Markewitz B, Mineau G, Pimentel R, Sawitzke A (2010) Heritability of vasculopathy, autoimmune disease, and fibrosis: a population-based study of systemic sclerosis. Arthritis Rheum 62:2109–2116
Pauling JD, Salazar G, Lu H, Betteridge ZE, Assassi S, Mayes MD, McHugh NJ (2018) Presence of anti-eukaryotic initiation factor-2B, anti-RuvBL1/2 and anti-synthetase antibodies in patients with anti-nuclear antibody negative systemic sclerosis. Rheumatology (Oxford) 57:712–717
Hughes M, Ong VH, Anderson ME, Hall F, Moinzadeh P, Griffiths B, Baildam E, Denton CP, Herrick AL (2015) Consensus best practice pathway of the UK scleroderma study group: digital vasculopathy in systemic sclerosis. Rheumatology (Oxford) 54:2015–2024
Cutolo M, Smith V (2013) State of the art on nailfold capillaroscopy: a reliable diagnostic tool and putative biomarker in rheumatology? Rheumatology (Oxford) 52:1933–1940
Smith V, Beeckman S, Herrick AL, Decuman S, Deschepper E, De Keyser F et al (2016) An EULAR study group pilot study on reliability of simple capillaroscopic definitions to describe capillary morphology in rheumatic diseases. Rheumatology (Oxford) 55:883–890
Kubo S, Smith V, Cutolo M, Tanaka Y (2018) The role of nailfold videocapillaroscopy in patients with systemic sclerosis. Immunol Med 4:113–119
Cutolo M, Melsens K, Wijnant S, Ingegnoli F, Thevissen K, De Keyser F et al (2018) Nailfold capillaroscopy in systemic lupus erythematosus: a systematic review and critical appraisal. Autoimmun Rev 7:344–352
Corominas H, Ortiz-Santamaría V, Castellví I, Moreno M, Morlà R, Clavaguera T et al (2016) Nailfold capillaroscopic findings in primary Sjögren’s syndrome with and without Raynaud’s phenomenon and/or positive anti-SSA/Ro and anti-SSB/La antibodies. Rheumatol Int 36:365–369
Bukhari M, Herrick AL, Moore T, Manning J, Jayson MI (1996) Increased nailfold capillary dimensions in primary Raynaud’s phenomenon and systemic sclerosis. Br J Rheumatol 35:1127–1131
Sebastiani M, Triantafyllias K, Manfredi A, González-Gay MA, Palmou-Fontana N, Cassone G, Drott U, Delbrück C, Rojas-Serrano J, Bertolazzi C, Nuño L, Giannini M, Iannone F, Vicente EF, Castañeda S, Selva-O’Callaghan A, Trallero Araguas E, Emmi G, Iuliano A, Bauhammer J, Miehle N, Parisi S, Cavagna L, Codullo V, Montecucco C, Lopez-Longo FJ, Martínez-Barrio J, Nieto-González JC, Vichi S, Confalonieri M, Tomietto P, Bergner R, Sulli A, Bonella F, Furini F, Scirè CA, Bortoluzzi A, Specker C, Barsotti S, Neri R, Mosca M, Caproni M, Weinmann-Menke J, Schwarting A, Smith V, Cutolo M, The American and European Network of Antisynthetase Syndrome Collaborative Group (2019) Nailfold capillaroscopy characteristics of antisynthetase syndrome and possible clinical associations: results of a multicenter international study. J Rheumatol 46:279–284
Hughes M, Moore T, O’Leary N, Tracey A, Ennis H, Dinsdale G, Murray A, Roberts C, Herrick AL (2015) A study comparing videocapillaroscopy and dermoscopy in the assessment of nailfold capillaries in patients with systemic sclerosis-spectrum disorders. Rheumatol 54:1435–1442
Pauling JD, Flower V, Shipley JA, Harris ND, McHugh NJ (2011) Influence of the cold challenge on the discriminatory capacity of the digital distal-dorsal difference in the thermographic assessment of Raynaud’s phenomenon. Microvasc Res 82:364–368
Pauling JD (2018) The challenge of establishing treatment efficacy for cutaneous vascular manifestations of systemic sclerosis. Expert Rev Clin Immunol 14:431–442
Dziadzio M, Denton CP, Smith R, Howell K, Blann A, Bowers E, Black CM (1999) Losartan therapy for Raynaud’s phenomenon and scleroderma: clinical and biochemical findings in a fifteen-week, randomized, parallel-group, controlled trial. Arthritis Rheum 42:2646–2655
Coleiro B, Marshall SE, Denton CP, Howell K, Blann A, Welsh KI, Black CM (2001) Treatment of Raynaud’s phenomenon with the selective serotonin reuptake inhibitor fluoxetine. Rheumatology (Oxford) 40:1038–1043
Pauling JD, Shipley JA, Harris ND, McHugh NJ (2012) Use of infrared thermography as an endpoint in therapeutic trials of Raynaud’s phenomenon and systemic sclerosis. Clin Exp Rheumatol 30:S103–S115
Wilkinson JD, Leggett SA, Marjanovic EJ, Moore TL, Allen J, Anderson ME, Britton J, Buch MH, del Galdo F, Denton CP, Dinsdale G, Griffiths B, Hall F, Howell K, MacDonald A, McHugh NJ, Manning JB, Pauling JD, Roberts C, Shipley JA, Herrick AL, Murray AK (2018) A multicenter study of the validity and reliability of responses to hand cold challenge as measured by laser speckle contrast imaging and thermography. Arthritis Rheum 70:903–911
Daniels J, Pauling JD, Eccleston C (2018) Behaviour change interventions for the management of Raynaud’s phenomenon: a systematic literature review. BMJ Open 2018;8:e024528
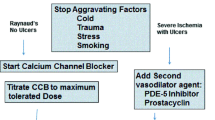
Denton C, Hughes M, Gak N, Vila J, Buch MH, Chakravarty K et al (2016) BSR and BHPR guideline for the treatment of systemic sclerosis. Rheumatology (Oxford) 55:1906–1910
Kowal-Bielecka O, Fransen J, Avouac J, Becker M, Kulak A, Allanore Y et al (2016) Update of EULAR recommendations for the treatment of systemic sclerosis. Ann Rheum Dis 76:1327–1339
Fernández-Codina A, Walker KM, Pope JE, Scleroderma Algorithm Group (2018) Treatment algorithms for systemic sclerosis according to experts. Arthritis Rheum 70:1820–1828
Rirash F, Tingey PC, Harding SE, Maxwell LJ, Tanjong Ghogomu E, Wells GA et al (2017) Calcium channel blockers for primary and secondary Raynaud’s phenomenon. Cochrane Database Syst Rev 12:CD000467
Roustit M, Blaise S, Allanore Y, Carpentier PH, Caglayan E, Cracowski J-L (2013) Phosphodiesterase-5 inhibitors for the treatment of secondary Raynaud’s phenomenon: systematic review and meta-analysis of randomised trials. Ann Rheum Dis 72:1696–1699
Denton CP, Hachulla É, Riemekasten G, Schwarting A, Frenoux J-M, Frey A, le Brun FO, Herrick AL, on behalf of the Raynaud Study Investigators (2017) Efficacy and safety of selexipag in adults with Raynaud’s phenomenon secondary to systemic sclerosis. Arthritis Rheum 69:2370–2379
Moinzadeh P, Riemekasten G, Siegert E, Fierlbeck G, Henes J, Blank N, Melchers I, Mueller-Ladner U, Frerix M, Kreuter A, Tigges C, Lahner N, Susok L, Guenther C, Zeidler G, Pfeiffer C, Worm M, Karrer S, Aberer E, Bretterklieber A, Genth E, Simon JC, Distler JHW, Hein R, Schneider M, Seitz CS, Herink C, Steinbrink K, Sárdy M, Varga R, Mensing H, Mensing C, Lehmann P, Neeck G, Fiehn C, Weber M, Goebeler M, Burkhardt H, Buslau M, Ahmadi-Simab K, Himsel A, Juche A, Koetter I, Kuhn A, Sticherling M, Hellmich M, Kuhr K, Krieg T, Ehrchen J, Sunderkoetter C, Hunzelmann N, The German Network for Systemic Scleroderma (2016) Vasoactive therapy in systemic sclerosis: real-life therapeutic practice in more than 3000 patients. J Rheumatol 43:66–74
Iorio ML, Masden DL, Higgins JP (2012) Botulinum toxin a treatment of Raynaud’s phenomenon: a review. Semin Arthritis Rheum 41:599–603
Momeni A, Sorice SC, Valenzuela A, Fiorentino DF, Chung L, Chang J (2015) Surgical treatment of systemic sclerosis-is it justified to offer peripheral sympathectomy earlier in the disease process? Microsurgery 35:441–446
Bello RJ, Cooney CM, Melamed E, Follmar K, Yenokyan G, Leatherman G, Shah AA, Wigley FM, Hummers LK, Lifchez SD (2017) The therapeutic efficacy of botulinum toxin in treating scleroderma-associated Raynaud’s phenomenon: a randomized, double-blind, placebo-controlled clinical trial. Arthritis Rheum 69:1661–1669
Author information
Authors and Affiliations
Contributions
JDP, MH and JEP conceived the idea for the manuscript, developed the search strategy and selection criteria. All authors contributed to the iterative drafting of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr Pauling has undertaken consultancy work and received speaker honoraria from Actelion pharmaceuticals. Dr Hughes has received speaker honoraria from Actelion pharmaceuticals. Dr Pope has undertaken consultancy work for AbbVie, Actelion, Baxter, Bayer, BMS, Lilly, Merck, Novartis, Pfizer, Roche, Sandoz, Sanofi and UCB.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pauling, J.D., Hughes, M. & Pope, J.E. Raynaud’s phenomenon—an update on diagnosis, classification and management. Clin Rheumatol 38, 3317–3330 (2019). https://doi.org/10.1007/s10067-019-04745-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-019-04745-5