Abstract
Objective
To study prognostic factors in different types of idiopathic inflammatory myopathies (IIM) associated with interstitial lung disease (ILD).
Patients and methods
Multicenter retrospective study of a Spanish cohort of patients diagnosed with IIM. Patients were classified into four categories: polymyositis (PM), dermatomyositis (DM), antisynthetase syndrome (ASS), and overlap myositis (OM). Sociodemographic data, clinical characteristics, antibodies, and treatments were collected. Cox regression models were calculated to identify factors associated with mortality, the necessity for long-term oxygen therapy (LTOT), and deterioration in respiratory function tests (RFT).
Results
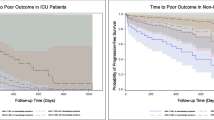
The number of patients included was 478, of whom 112 (23.4%) suffered from ILD: 17% PM, 16% DM, 45% ASS, and 22% OM. Factors associated with mortality in the multivariate analysis were clinically meaningful progression of ILD after 3 months (CMP 3m) (hazard ratio (HR) 9.48, p = 0.005), severe infections (HR 6.41, p = 0.016), heliotrope erythema (HR 31.1, p = 0.002), delay in diagnosis (HR 1.29; p = 0.011), and Raynaud’s phenomenon (HR 11.9, p = 0.007). However, being female (HR 0.19, p = 0.044) and positivity solely for ANAs (HR 0.08, p = 0.008) presented a protective effect. CMP 3m (HR 22.7, p = 0.027) was associated with the need for LTOT, while basal aldolase (HR 0.90; p = 0.049) had a protective effect. Likewise, joint manifestations (HR 0.04, p = 0.034) were shown to reduce risk of deterioration in RFT.
Conclusions
CMP 3m, severe infections, delay in diagnosis, heliotrope erythema, and Raynaud’s phenomenon were identified as factors of poor prognosis in different IIM associated with ILD.

Similar content being viewed by others
References
Hallowell RW, Ascherman DP, Danoff SK (2014) Pulmonary manifestations of polymyositis/dermatomyositis. Seminars in respiratory and critical care medicine 35(2):239–248
Nuno-Nuno L, Joven BE, Carreira PE et al (2017) Mortality and prognostic factors in idiopathic inflammatory myositis: a retrospective analysis of a large multicenter cohort of Spain. Rheumatol Int 37(11):1853–1861
Yamasaki Y, Yamada H, Ohkubo M et al (2011) Longterm survival and associated risk factors in patients with adult-onset idiopathic inflammatory myopathies and amyopathic dermatomyositis: experience in a single institute in Japan. J Rheumatol 38(8):1636–1643
Dobloug GC, Svensson J, Lundberg IE, Holmqvist M (2018) Mortality in idiopathic inflammatory myopathy: results from a Swedish nationwide population-based cohort study. Ann Rheum Dis 77(1):40–47
Tanizawa K, Handa T, Nakashima R, Kubo T, Hosono Y, Aihara K, Ikezoe K, Watanabe K, Taguchi Y, Hatta K, Oga T, Chin K, Nagai S, Mimori T, Mishima M (2013) The prognostic value of HRCT in myositis-associated interstitial lung disease. Respir Med 107(5):745–752
Moghadam-Kia S, Oddis CV, Sato S, Kuwana M, Aggarwal R (2016) Anti-melanoma differentiation-associated gene 5 is associated with rapidly progressive lung disease and poor survival in US patients with amyopathic and myopathic dermatomyositis. Arthritis care & research 68(5):689–694
Fujisawa T, Hozumi H, Kono M, Enomoto N, Hashimoto D, Nakamura Y, Inui N, Yokomura K, Koshimizu N, Toyoshima M, Shirai T, Yasuda K, Hayakawa H, Suda T (2014) Prognostic factors for myositis-associated interstitial lung disease. PLoS One 9(6):e98824
Kurita T, Yasuda S, Amengual O, Atsumi T (2015) The efficacy of calcineurin inhibitors for the treatment of interstitial lung disease associated with polymyositis/dermatomyositis. Lupus 24(1):3–9
Isoda K, Takeuchi T, Kotani T et al (2014) Pre-treatment ferritin level and alveolar-arterial oxygen gradient can predict mortality rate due to acute/subacute interstitial pneumonia in dermatomyositis treated by cyclosporine a/glucocorticosteroid combination therapy: a case control study [corrected]. PLoS One 9(2):e89610
Shi J, Li S, Yang H, Zhang Y, Peng Q, Lu X, Wang G (2017) Clinical profiles and prognosis of patients with distinct antisynthetase autoantibodies. J Rheumatol 44(7):1051–1057
Zamora AC, Hoskote SS, Abascal-Bolado B, White D, Cox CW, Ryu JH, Moua T (2016) Clinical features and outcomes of interstitial lung disease in anti-Jo-1 positive antisynthetase syndrome. Respir Med 118:39–45
Bohan A, Peter JB (1975) Polymyositis and dermatomyositis (first of two parts). N Engl J Med 292(7):344–347
Bohan A, Peter JB (1975) Polymyositis and dermatomyositis (second of two parts). N Engl J Med 292(8):403–407
Tanimoto K, Nakano K, Kano S et al (1995) Classification criteria for polymyositis and dermatomyositis. J Rheumatol 22(4):668–674
Arnett FC, Edworthy SM, Bloch DA et al (1998) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31(3):315–324
(1980) Preliminary criteria for the classification of systemic sclerosis (scleroderma). Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee. Arthritis Rheum 23(5):581–590
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40(9):1725
Alarcon-Segovia D, Cardiel MH (1989) Comparison between 3 diagnostic criteria for mixed connective tissue disease. Study of 593 patients. The Journal of rheumatology 16(3):328–334
Fox RI, Robinson CA, Curd JG, Kozin F, Howell FV (1986) Sjogren's syndrome. Proposed criteria for classification. Arthritis Rheum 29(5):577–585
Nuno L, Joven B, Carreira P et al (2017) Multicenter registry on inflammatory myositis from the Rheumatology Society in Madrid, Spain: descriptive analysis. Reumatologia clinica 13(6):331–337
Khanna D, Mittoo S, Aggarwal R, Proudman SM, Dalbeth N, Matteson EL, Brown K, Flaherty K, Wells AU, Seibold JR, Strand V (2015) Connective tissue disease-associated interstitial lung diseases (CTD-ILD) - report from OMERACT CTD-ILD working group. J Rheumatol 42(11):2168–2171
Zhang L, Wu G, Gao D, Liu G, Pan L, Ni L, Li Z, Wang Q (2016) Factors associated with interstitial lung disease in patients with polymyositis and dermatomyositis: a systematic review and meta-analysis. PLoS One 11(5):e0155381
Fujisawa T, Hozumi H, Kono M, Enomoto N, Nakamura Y, Inui N, Nakashima R, Imura Y, Mimori T, Suda T (2017) Predictive factors for long-term outcome in polymyositis/dermatomyositis-associated interstitial lung diseases. Respir Investig 55(2):130–137
Tada Y, Suematsu E, Ueda A et al (2012) Clinical factors to predict a poor prognosis and refractory disease in patients with polymyositis and dermatomyositis associated with interstitial lung disease. Clin Exp Rheumatol 30(3):450
Sugiyama Y, Yoshimi R, Tamura M, Takeno M, Kunishita Y, Kishimoto D, Yoshioka Y, Kobayashi K, Takase-Minegishi K, Watanabe T, Hamada N, Nagai H, Tsuchida N, Soejima Y, Nakano H, Kamiyama R, Uehara T, Kirino Y, Sekiguchi A, Ihata A, Ohno S, Nagaoka S, Nakajima H (2018) The predictive prognostic factors for polymyositis/dermatomyositis-associated interstitial lung disease. Arthritis research & therapy 20(1):7
Cavagna L, Nuno L, Scire CA et al (2015) Clinical spectrum time course in anti Jo-1 positive antisynthetase syndrome: results from an international retrospective multicenter study. Medicine 94(32):e1144
Obert J, Freynet O, Nunes H, Brillet PY, Miyara M, Dhote R, Valeyre D, Naccache JM (2016) Outcome and prognostic factors in a French cohort of patients with myositis-associated interstitial lung disease. Rheumatol Int 36(12):1727–1735
Trallero-Araguas E, Grau-Junyent JM, Labirua-Iturburu A et al (2016) Clinical manifestations and long-term outcome of anti-Jo1 antisynthetase patients in a large cohort of Spanish patients from the GEAS-IIM group. Semin Arthritis Rheum 46(2):225–231
Chen F, Wang D, Shu X, Nakashima R, Wang G (2012) Anti-MDA5 antibody is associated with a/SIP and decreased T cells in peripheral blood and predicts poor prognosis of ILD in Chinese patients with dermatomyositis. Rheumatol Int 32(12):3909–3915
Hoshino K, Muro Y, Sugiura K, Tomita Y, Nakashima R, Mimori T (2010) Anti-MDA5 and anti-TIF1-gamma antibodies have clinical significance for patients with dermatomyositis. Rheumatology (Oxford, England) 49(9):1726–1733
Fujikawa K, Kawakami A, Kaji K et al (2009) Association of distinct clinical subsets with myositis-specific autoantibodies towards anti-155/140-kDa polypeptides, anti-140-kDa polypeptides, and anti-aminoacyl tRNA synthetases in Japanese patients with dermatomyositis: a single-centre, cross-sectional study. Scand J Rheumatol 38(4):263–267
Labrador-Horrillo M, Martinez MA, Selva-O’Callaghan A et al (2014) Anti-MDA5 antibodies in a large Mediterranean population of adults with dermatomyositis. J Immunol Res 2014:290797
Mejia M, Herrera-Bringas D, Perez-Roman DI et al (2017) Interstitial lung disease and myositis-specific and associated autoantibodies: clinical manifestations, survival and the performance of the new ATS/ERS criteria for interstitial pneumonia with autoimmune features (IPAF). Respir Med 123:79–86
Ha YJ, Hur J, Go DJ, Kang EH, Park JK, Lee EY, Shin K, Lee EB, Song YW, Lee YJ (2018) Baseline peripheral blood neutrophil-to-lymphocyte ratio could predict survival in patients with adult polymyositis and dermatomyositis: a retrospective observational study. PLoS One 13(1):e0190411
Pinal-Fernandez I, Casal-Dominguez M, Huapaya JA, Albayda J, Paik JJ, Johnson C, Silhan L, Christopher-Stine L, Mammen AL, Danoff SK (2017) A longitudinal cohort study of the anti-synthetase syndrome: increased severity of interstitial lung disease in black patients and patients with anti-PL7 and anti-PL12 autoantibodies. Rheumatology (Oxford, England) 56(6):999–1007
Marie I, Hatron PY, Dominique S, Cherin P, Mouthon L, Menard JF, Levesque H, Jouen F (2012) Short-term and long-term outcome of anti-Jo1-positive patients with anti-Ro52 antibody. Semin Arthritis Rheum 41(6):890–899
Amaral Silva M, Cogollo E, Isenberg DA (2016) Why do patients with myositis die? A retrospective analysis of a single-centre cohort. Clin Exp Rheumatol 34(5):820–826
Airio A, Kautiainen H, Hakala M (2006) Prognosis and mortality of polymyositis and dermatomyositis patients. Clin Rheumatol 25(2):234–239
Huber AM, Mamyrova G, Lachenbruch PA, Lee JA, Katz JD, Targoff IN, Miller FW, Rider LG, for the Childhood Myositis Heterogeneity Collaborative Study Group (2014) Early illness features associated with mortality in the juvenile idiopathic inflammatory myopathies. Arthritis care & research 66(5):732–740
Tanizawa K, Handa T, Nakashima R, Kubo T, Hosono Y, Watanabe K, Aihara K, Ikezoe K, Sokai A, Nakatsuka Y, Taguchi Y, Hatta K, Noma S, Kobashi Y, Yoshizawa A, Oga T, Hirai T, Chin K, Nagai S, Izumi T, Mimori T, Mishima M (2017) The long-term outcome of interstitial lung disease with anti-aminoacyl-tRNA synthetase antibodies. Respir Med 127:57–64
Funding
This study was partially funded with a grant from MSD (MSD-SORCOM). The SORCOM and MSD had no role in the extraction and interpretation of data or in the draft of the manuscript. All authors had full access to all the data included in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None
Ethical approval
This study was approved by the ethics committees of the participant hospitals and carried out in compliance with the Helsinki Declaration.
Electronic supplementary material
ESM 1
(DOCX 32 kb)
Rights and permissions
About this article
Cite this article
Cobo-Ibáñez, T., López-Longo, FJ., Joven, B. et al. Long-term pulmonary outcomes and mortality in idiopathic inflammatory myopathies associated with interstitial lung disease. Clin Rheumatol 38, 803–815 (2019). https://doi.org/10.1007/s10067-018-4353-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-018-4353-2