Abstract
Early diagnosis and treatment of giant cell arteritis (GCA) is crucial for preventing ischemic complications. Multiple serological markers have been identified; however, there is a distinct lack of predicting markers for GCA relapse and complications. Our main objective was to identify serological parameters in a large cohort of treatment-naïve GCA patients, which could support clinicians in evaluating the course of the disease. Clinical data was gathered, along with analyte detection using Luminex technology, ELISA, and nephelometry, among others. Unsupervised hierarchical clustering and principal component analysis of analyte profiles were performed to determine delineation of GCA patients and healthy blood donors (HBDs). Highest, significantly elevated analytes in GCA patients were SAA (83-fold > HBDs median values), IL-23 (58-fold), and IL-6 (11-fold). Importantly, we show for the first time significantly changed levels of MARCO, alpha-fetoprotein, protein C, resistin, TNC, TNF RI, M-CSF, IL-18, and IL-31 in GCA versus HBDs. Changes in levels of SAA, CRP, haptoglobin, ESR, MMP-1 and MMP-2, and TNF-alpha were found associated with relapse and visual disturbances. aCL IgG was associated with limb artery involvement, even following adjustment for multiple testing. Principal component analysis revealed clear delineation between HBDs and GCA patients. Our study reveals biomarker clusters in a large cohort of patients with GCA and emphasizes the importance of using groups of serological biomarkers, such as acute phase proteins, MMPs, and cytokines (e.g. TNF-alpha) that could provide crucial insight into GCA complications and progression, leading to a more personalized disease management.
Similar content being viewed by others
Introduction
Giant cell arteritis (GCA) is characterized by general symptoms, such as fatigue and weight loss, and ischemic symptoms, such as severe headaches, vision disturbances, and jaw claudication [1]. The five 1990 ACR classification criteria for GCA include age over 50 (at disease presentation), newly experienced headache, temporal artery abnormality, elevated erythrocyte sedimentation rate (ESR) and positive artery biopsy. Presence of at least three criteria yields a diagnostic sensitivity of 93% and a specificity of 91% for GCA [2]. Temporal artery biopsy (TAB) represented until recently a gold standard for GCA confirmation; nonetheless, a negative biopsy cannot exclude the diagnosis. Presently, clinicians are relying more on ultrasound results of cranial and extracranial arteries, showing better sensitivity in comparison to TAB [3]. The most urgent conditions in GCA are visual disturbances, which could be, as a consequence of ischemic optic neuropathy, transient or permanent and may lead to partial or even complete vision loss. GCA remains one of the main causes of blindness in elderly people in Western countries [4]. Permanent visual loss can be prevented if GCA is treated promptly with glucocorticoids [5,6,7]. However, high doses of glucocorticoids may exhibit a variety of side effects and even though a slow tapering regiment (treatment duration usually over 2 years) is applied, relapses often occur [5]. The clinical course of GCA is highly variable from patient to patient, although generally, there is improvement with an overall disease resolution following treatment. The number of patients diagnosed with GCA by 2050 is projected to be over 3 million in Europe, North America, and Oceania, representing a significant clinical and financial challenge [8]. Several previous reports have described potential serological markers for GCA [9,10,11,12,13,14,15,16,17,18], among them cytokines, chemokines, growth factors, cell adhesion molecules, and matrix metalloproteinases (MMPs). In 2000, Weyand et al. emphasized that interleukin (IL)-6 may act as a biological marker of GCA activity in untreated and treated GCA patients [19]. Cid et al. reported that presence of a strong acute phase response defined a subgroup of patients with very low risk of developing visual loss and cranial ischemic complications in GCA [20]. In line with this report, Hocevar et al. confirmed the negative association between high levels of acute phase proteins and visual loss and exposed a novel positive association between acute phase proteins and relapse in GCA patients [5]. A current comprehensive review on serological markers in GCA [21] highlights and confirms IL-6, as significantly and prevalently elevated in sera of GCA patients, and acute phase parameters (e.g., C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), serum amyloid A (SAA), haptoglobin and fibrinogen) as an added value for distinguishing subgroups of GCA patients with visual disturbances and predicting relapses. Elevated IL-6, along with acute phase proteins, may help preserve luminal patency or have a compensatory role by inducing angiogenesis in vasculopathies, such as GCA [22]. On the other hand, indicators of an enhanced systemic inflammatory response may lead to an earlier diagnosis and timely treatment, thus preventing ischemic complications [23]. There have been reports indicating the usefulness of serological acute phase (ESR and CRP) and inflammatory markers (IL-6) for the course during therapy of GCA [17, 19, 24]. However, there is still a paucity of valid serological markers strongly needed for monitoring GCA relapse and complications [21, 24,25,26]. Therefore, we set out to measure and analyze serological analytes in a large cohort of clinically well-characterized untreated GCA patients that could help clinicians evaluate the course of the disease, including relapse/complications.
Material and methods
Subjects’ diagnosis, symptoms and comorbidities
The diagnosis of GCA was based on the 1990 ACR classification criteria, and a positive TAB or the presence of the halo sign on TA color Doppler sonography (CDS). In cases of suspected large vessel GCA (lvGCA), CDS of the large arteries (carotid, vertebral, subclavian, axillary, and brachial arteries) or PET/CT or both were performed [1]. Ninety-eight treatment-naïve GCA patients were consecutively enrolled in the study between the years 2011 and 2015. The recorded symptoms, signs, and comorbidities are included (Table 1). Only complete patient cases (n = 97) were used for further analysis (one patient was omitted due to missing data).
Blood of healthy blood donors (HBDs, n = 53) was obtained from the National Blood Transfusion Center of Slovenia. Six HBDs were excluded, as their SAA values measured over 6.4 μg/ml (n = 47) and one HBD was omitted due to missing data (n = 46). The cut-off reference value for SAA was set on a population with normal CRP serum levels (95th percentile = 5.0 mg/L, n = 483), with the 95th percentile for N Latex SAA found to be 6.4 mg/L (N Latex SAA protocol data sheet, Siemens, BN Prospec System).
Sample processing
All routinely processed serum samples were measured immediately following blood collection and centrifugation 3000×g for 5 min. Specifically, 17 parameters (leukocytes, thrombocytes, hemoglobin, albumin, anti-β2 glycoprotein I (aβ2GPI) IgG, aβ2-GPI IgM, anti-cardiolipin antibodies (aCL) IgG, aCL IgM, aPS/PT IgA, aPS/PT IgG, aPS/PT IgM, CRP, ESR, ferritin, fibrinogen, haptoglobin, and LA) were measured using standard operational procedures, quality controls, and calibration curves.
All non-routinely measured serum samples were collected following blood clotting and centrifugation 3000×g for 5 min, aliquoted and stored at − 80 °C, until subjected to further analysis. Forty-eight markers were determined in the same series of measurements (same lot no. of reagents) using standard calibration curves.
Laboratory methodology for serological parameters
Overall, 65 laboratory parameters were assessed (Supplementary Table I). The strategy for evaluating serological parameters is provided (Supplemental Fig. 1). Seventeen analytes were measured routinely in up to 98 GCA patients. Out of the remaining 48 parameters, 4 were measured in a lower number of patients and HBDs (alpha-1-acid glycoprotein (AGP), hemopexin, BAFF, and MARCO), while 27 analytes were measured in the main, complete cohort (97 GCA patients and 46 HBDs) (Supplemental Fig. 1).
Specifically, the following parameters were measured: complete blood count (Siemens Advia 120, including leukocytes and thrombocytes), ESR (WesternGreen method, 1 h), CRP and albumin (ADVIA 1800 CRP and albumin assay, respectively), fibrinogen (Siemens BCS XP with reagent Multifibren U), ferritin (ADVIA Centaur by direct chemiluminometric technology), haptoglobin, AGP, hemopexin, and serum amyloid A (SAA) were determined using immunonephelometry (BN Prospec System, Siemens) and immunoserology using in-house enzyme-linked immunosorbent assay (ELISA) aCL IgG, IgM, aβ2GPI IgG, IgM, and anti-phosphatidylserine-dependent prothrombin antibodies (aPS/PT) IgG, IgM, and IgA). IL-6 serum protein levels were measured by human IL-6 ELISA (Invitrogen, Belgium) following manufacturer’s instructions. Lupus anti-coagulant activity was determined by the Siemens BCS XP LA clotting test. In addition, macrophage receptor with collagenous structure (MARCO) and B cell activating factor (BAFF) were detected using sandwich ELISAs (Invitrogen, UK).
Luminex xMAP technology
For the measurement of 42 serum analyte levels, an AtheNa Multi-Lyte analyzer was used (Luminex xMAP Technology, Luminex Inc., Austin, TX, USA). The calibration curve for each molecule was analyzed with a five-parameter logistic curve (Milliplex Analyst, Merck).
Data preprocessing and statistical analysis
The analysis of the data generated by Luminex xMAP Technology, ELISA, and nephelometry was performed in R version 3.2.3 [27]. Differences in the analyte levels, between the two groups, were calculated using the non-parametric Mann-Whitney U test and the resulting p values were adjusted for multiple testing with the Benjamini-Hochberg method [28]. p values ≤ 0.05 were considered as statistically significant. Heatmaps and the biplot (PCA analysis) were performed on log2 transformed and scaled data and generated with the R packages gplots, corrplot, and ggbiplot, respectively. Hierarchical clustering with Euclidean distance and Ward linkage was performed and visualized as a heatmap. The correlation matrix was generated with Spearman’s correlation using the pairwise complete method and visualized as a heatmap with hierarchical clustering order using the R package corrplot. Principal component analysis (PCA) was performed and the first two principal components were visualized as a biplot. The database of known and predicted protein interactions STRING 10.5 [29] was used for analysis of interactions between all the proteins tested in the unsupervised hierarchical clustering, and the connecting line thickness between nodes specifies the strength of data support for interaction of proteins (data used were from experimentally determined and predicted interactions). Additional STRING analysis was performed separately for the three clusters resulting from unsupervised hierarchical clustering and analytes associated with assigned Gene Ontology (GO) annotations. Associations of the 48 measured parameters and age, with the 8 clinical complications, were calculated using the non-parametric Mann-Whitney U test, and the resulting p values were adjusted for multiple testing with the Benjamini-Hochberg method [28]. By applying binomial logistic regression using generalized linear models in R, we assessed the association of various combinations of five autoantibodies with evaluated visual disturbances.
Ethical approval and consent to participate
Ethical approval no. 99/04/15 for the Giant Cell Arteritis study was obtained from the Slovenian National Medical Ethics Committee. All patients provided written informed consent to participate in the study. We confirm that all experiments were performed in accordance with relevant guidelines and regulations.
Results
Patient characteristics
The demographic, clinical, and routine laboratory parameters, and comorbidities of GCA patients (n = 98) are provided in Table 1. There were 67% females and the median (Q25–Q75) patient age was 74.1 (67.3–78.8). HBDs comprised of 27 females (58.7%) and 19 males (41.3%) with median (Q25–Q75) age of 50.8 (35.5–55.1). Thirty-eight percent of GCA patients were smokers, 14% had diabetes, and 53% of GCA patients had hypertension. Patients were included in the study after a median (Q25–Q75) duration of symptoms of 30 days (20–90), and most common clinical signs were general symptoms (fatigue, sweating, fever, or loss of weight; 77%), new headache onset (66%), and clinically changed temporal artery (63%). Eighty-two percent of patients (n = 79/98) fulfilled ACR classification criteria [1], including 31 out of 44 patients with lvGCA. Eleven patients did not fulfill ACR classification criteria; their diagnosis was based on the result of the CDS of large arteries (n = 10/11) and/or PET/CT (n = 1/11). All patients underwent an ultrasound examination and the halo sign was found in 78% (76/98). Temporal artery biopsy (performed in 81/98) was positive in 64 (79%) GCA patients examined. Ultrasound of branches of the aortic arch (including subclavian, axillary, vertebral, and carotid arteries) was performed in 76% (74/98) GCA patients (with 42% confirmed with extracranial involvement). At suspicion of large extracranial vessel involvement, PET/CT was performed, in addition to ultrasound in 16/98 cases (16%). Among these, 75% (12/16) showed enhanced vascular 18-FDG uptake consistent with vasculitis.
Patients that were followed up for at least 1 year after diagnosis (n = 85) were included in evaluation of relapses. Among the group, 41% (35 patients) experienced relapse.
Analysis of biomarker profiles
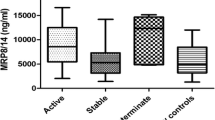
Out of 48 laboratory parameters tested in GCA patients and HBDs (Supplemental Fig. 1), 17 parameters did not show significant differences: ICAM-1, IP-10, IL-1 alpha, IL-1 R, IL-4, IL-12p70, IL-22, IL-33, L-selectin, leptin, LIF, MMP3, MMP-12, MCP-1, MIG, uPA, and uPAR. Out of the selected 31 analytes (Table 2), 27 showed significant changes between the groups. Analytes found to be statistically significantly increased in GCA patients were CHI3L1, IFN-gamma, IL-1 beta, IL-6, IL-8, IL-10, IL-18, IL-23, IL-27, IL-31, M-CSF, MMP-1, MMP-9, protein C, resistin, SAA, tenascin C (TNC), TNF R1, VCAM-1, and VEGF. The highest increases in serum median levels of GCA patients vs. HBDs were observed for SAA (83-fold change), IL-23 (58-fold), IL-6 (11-fold), and IL-8 (8-fold). Three analytes, alpha-fetoprotein, IL-13, and MMP-2, were found to be decreased in sera of GCA patients as compared to HBDs. Some analytes, such as IFN-gamma, IL-1 beta, IL-10, and IL-31, were found at very low levels (and still showed significant changes between GCA vs. HBDs), while IL-2, IL-9, IL-17A, and TNF-alpha did not show significant changes. Four analytes (hemopexin, AGP, BAFF, and MARCO) were measured in a lower number of GCA patients and HBDs but exhibited significantly increased levels in GCA vs. HBDs (Table 2).
In order to investigate the relationship between the individual analytes, correlations were calculated for 97 GCA patients and 46 HBDs, separately (Fig. 1). The analytes exhibited a higher relationship with each other in the HBDs than in GCA patients. Correlation values were clustered, thereby identifying smaller groups of closely correlated analytes. In HBDs, two positively correlated clusters (G1 and G2) and one negatively correlated cluster (G3) were observed, while in GCA patients, only one positively correlated cluster (G4) remained, resembling to some extent, the second positively correlated cluster in the HBD. Mainly weak positive correlations were observed in the GCA patients. The highest positively correlated analytes in HBDs were IL-8 with IL-6, IL-27 with IL-13, as well as IL-27, protein C, and IL-13 with alpha-fetoprotein (Spearman’s correlation coefficient ≥ 0.8). In the GCA patients, two of these positive correlations held up (IL-27 and protein C with alpha-fetoprotein) with a Spearman’s correlation coefficient > 0.65. Negative correlations were profoundly less pronounced in both, HDBs and GCA, with the two most closely negatively correlated markers in HBDs (IL-6 and IL-23) having a Spearman’s correlation coefficient of − 0.56.
Serum biomarker correlations for GCA (27 analytes, bottom panel) and HBD (25 analytes, top panel). Individual cytokines are listed on the axes with boxes indicating selected groups of highly correlated cytokines. Spearman’s correlation was applied to calculate associations between serum biomarkers. The color indicates the type of correlation (red—positive, blue—negative), and its shade reflects the strength of correlation between pairs of cytokines, irrespective of absolute serum levels. IL-9 and IL-17A had to be excluded from the HBD analysis because they did not exhibit any variation. Two clusters of positive correlations (G1 and G2) and one cluster of negative correlations (G3) were noted primarily in HBDs (n = 46), among the analytes. GCA patients (n = 97) exhibit only a cluster of positive correlations (G4)
To further explore the biomarker dataset, we performed hierarchical clustering of subjects and analytes. The 27 analytes clearly delineate GCA patients from HBDs, as reflected in the heatmap (Fig. 2a). Only two GCA patients fall into the cluster of HBDs (G47 and G54). Furthermore, analytes are clustered into three groups (C1, C2, and C3) comprising (C1) MMP-9, MMP-2, protein C, MMP-1, CHI3L1, VEGF, TNC, resistin, VCAM-1, TNF R1, and SAA; (C2) TNF-alpha, IL-8, IL-1 beta, IFN-gamma, IL-31, IL-17A, IL-9, IL-23, IL-18, and IL-6; and (C3) IL-10, IL-27, IL-2, IL-13, M-CSF, alpha-fetoprotein. IL-1 beta, IL-9, IL-17A, and IL-31 present in the second cluster all measured around their limit of detection (LoD), with only few patients showing elevated levels. Analytes generally had higher values in GCA patients than HBDs, except for alpha-fetoprotein and IL-13, which both fall into the third cluster, as well as MMP-2, which falls into the first cluster, along with MMP-1 and MMP-9.
Heatmap and STRING analysis of serum levels for 27 analytes. a Hierarchical clustering of biomarkers and patients in cytokine dataset. Analytes (n = 27) are represented by shades of blue to red in the heatmap, with lowest values in dark blue and the highest in red. In this unsupervised cluster analysis, healthy subjects (n = 46) are indicated in light gray and GCA patients (n = 97) in dark gray, with only two patients found within the HBD group, and all analytes are clustered in three subgroups C1, C2, and C3. GCA (n = 97, prefix G), HBDs (n = 46, prefix H). b–e STRING network analysis for the 27 analytes. b All analytes used for hierarchical clustering of GCA and HBD were examined for existing interactions with thickness of connecting line indicating the strength of data support. c–e Evaluation of GO annotations of analytes in each cluster was gathered from experimental data unsupervised hierarchical clustering with associations with specific GO terms. FDR, false discovery rate
Using STRING analysis (Fig. 2b–e), we found that the strongest GO term assigned to analytes from cluster C2 was positive regulation of cytokine production (false discovery rate [FDR]: 4.8 × 10−7), T cell proliferation (FDR 8.6 × 10−7) (Fig. 2d), while weaker associations were found for C1 with leukocyte migration (FDR 1.1 × 10−5) (Fig. 2c) and C3 with mononuclear cell proliferation (Fig. 2e).
Finally, we investigated the variation patterns in the biomarker dataset using principal component analysis (PCA) and visualized principal components 1 and 2, which explain 21 and 13.4% of the total variance, respectively (Fig. 3). PC1 and PC2 clearly separate the GCA patients from the HBDs with PC1 mainly contributing to the separation; however, GCA patients G2 and G47 represent exceptions, which exhibit analyte profiles more similar to those of HBDs. TNF R1, CHI3L1, TNC, IL-1 beta, IL-18, and MMP-2 were the main contributors to the separation, as they exhibited the highest correlation with PC1. Higher levels of MMP-2, IL-13, and alpha-fetoprotein were characteristic for HBDs, with MMP-2 opposing the rest of the analytes and strongly pointing towards HBDs. Patient G2 was a different patient outlier in the PCA analysis (Fig. 3), as compared to hierarchical clustering (Fig. 2a), although patient G47 appeared as an outlier in both analyses.
Principal component analysis for GCA and HBDs using 27 analytes. Principal component analysis (PCA) was used to evaluate the delineation of the GCA patients (in light blue) and HBDs (in black) based on 27 analytes. GCA patients and HBDs can be well separated by principal components 1 and 2, which explain 21.0 and 13.4% of the total variance, respectively. The labels reflect the scores of the subjects and the red vectors the loadings of the analytes GCA patients G2 and G47 represent exceptions, which exhibit an analyte profile more similar to that of HBDs. Samples of a group are enclosed by a concentration ellipse with 68% probability. GCA (n = 97, prefix G), HBDs (n = 46, prefix H)
Associations of measured parameters with clinical complications
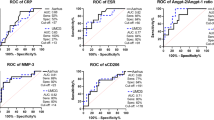
To identify specific parameters associated with clinical complications, we tested 48 serological parameters and age, with 8 clinical symptoms or complications. The 48 serological parameters were alpha-fetoprotein, CHI3L1, IFN-gamma, IL-1beta, IL-2, IL-6, IL-8, IL-9, IL-10, IL-13, IL-17A, IL-18, IL-23, IL-27, IL-31, M-CSF, MMP-1, MMP-2, MMP-9, protein C, resistin, TNC, TNF-alpha, TNF RI, VCAM-1, VEGF, AGP, hemopexin, MARCO, BAFF, ESR, CRP, SAA, leukocytes, hemoglobin, thrombocytes, albumin, fibrinogen, ferritin, haptoglobin, aCL IgG in IgM, aβ2 GPI (IgG, IgM, IgA), and aPS/PT (IgG, IgM, IgA). Nineteen parameters showed statistically significant association to a variety of GCA complications (Table 3). Older age and decreased IFN-gamma serum levels were found associated with general symptoms, while older age and higher levels of MMP-1 were linked to PMR. For acute visual disturbances, all acute phase parameters tested, such as SAA, CRP, haptoglobin, ESR, and thrombocyte numbers, were all found significantly decreased. In addition, MMP-1 was decreased in the GCA group with visual disturbances, while TNF-alpha was increased. Of all tested parameters, age was the only one that showed significant association to permanent visual loss, with older patients being more frequently affected. SAA, CRP, and ESR were all found to be positively associated with relapse, while MMP-2 was found negatively associated. Furthermore, serum levels of MARCO were significantly higher in cases of jaw claudication and lower in limb artery involvement. The only statistically significant marker after multiple testing was aCL IgG, found to be associated with limb artery involvement (Table 3).
When autoantibody combinations of aCL IgG, IgM, aβ2GPI IgG, IgM, and LA were analyzed using binomial linear regression, we could not determine significant associations with any of the evaluated visual disturbances (all visual disturbances, amaurosis fugax, and permanent visual loss).
Discussion
In our study, we focused on providing the most optimal serum analytes that would allow us to characterize treatment-naïve GCA patients and shed light on their different clinical manifestations. Importantly, we show for the first time significantly changed levels of MARCO, alpha-fetoprotein, protein C, resistin, TNC, TNF RI, M-CSF, IL-18, and IL-31 in GCA patients vs. HBDs. The three most highly elevated analytes found in our GCA patients (SAA, IL-23, and IL-6) already represent good therapeutical targets. In fact, a recent anti-IL-6 receptor therapy trial has indicated tocilizumab as an effective glucocorticoid sparing agent [30]. Tocilizumab monotherapy was reported to result in normalization of immune-inflammatory molecules, as defined by the healthy controls [31]. Additionally, serum levels of osteopontin could represent a suitable disease activity biomarker in tocilizumab-treated patients with GCA [32].
While a report from a 52-week trial indicated that anti-IL-23 ustekinumab may be effective for treatment of refractory GCA [33], an interventional ustekinumab clinical trial is still in progress (NCT02955147).
Current anti-SAA therapies are not yet available, even though SAA is 83-fold changed in GCA above HBD. A recent report on anti-SAA antibodies indicates that these naturally occurring IgG autoantibodies could decrease IL-6 protein levels released from SAA/SAA1α-treated peripheral blood mononuclear cells [34].
Acute phase parameters (e.g., SAA, CRP, ESR) are important in GCA [5], which is a highly inflammatory disease [22]. O’Neill et al. previously reported on comparable levels of SAA in sera of 16 GCA patients [35]. Furthermore, studies of acute phase proteins revealed that, in particular, when comparing GCA to their disease control patients (initially suspected to have GCA, but later not confirmed), SAA, CRP, and haptoglobin may serve as a distinguishing, significantly upregulated group of analytes [36]. The current work confirms our previous results [5] that reported negatively correlated SAA, CRP, ESR, and haptoglobin to visual disturbances and positively correlated SAA, CRP, and ESR with relapse in untreated GCA patients (Table 3).
Predominant Th-1/Th-17 responses were reported in cells/tissues of GCA patients [37,38,39]. Their distinct cytokines IL-1 beta, IL-17A, TNF-alpha, and IFN-gamma were however found in low levels in sera of the GCA patients tested in the current study (Table 2); therefore, their determination using high-sensitivity assays could provide more information on whether they could be relevant serum analytes to test in the future. They could serve as markers for subgroups of patients with certain symptoms or complications, as TNF-alpha was found to be associated with visual disturbances. Other groups reported on elevated IL-17; however, they utilized high-sensitivity assays [37] or cell stimulation tests [40] to measure IL-17 concentrations in sera and supernatants, respectively.
IL-12 and IL-23 are cytokines involved in Th-1 and Th-17 polarization [41]. IL-12, a described stimulator of Th-1 response, is absent in sera of the GCA patients in the current study, while IL-23, an activator of Th-17 response, is one of the most highly elevated analytes. However, 29/97 patients showed levels of IL-23 below LoD; thus, a more personalized approach to interpreting serological data is advisable. Interestingly, both IL-12 and IL-23 share a common subunit (p40), allowing ustekinumab to target both cytokines, and in theory, disrupt the Th-1 and Th-17 responses [42]. Typical Th-2 cytokines, such as IL-4, IL-5, and IL-10, were consistently below LoD in our assays.
Previous reports emphasized the importance of MMPs in GCA, especially in tissue- and cell-based studies, while relatively few serological studies were reported. In our preliminary study, we tested MMP-1, MMP-2, MMP-3, MMP-9, and MMP-12, with only MMP-1, MMP-2, and MMP-9 showing significantly changed levels in GCA patients as compared to HBDs, on which we conducted further analysis. Interestingly, the gelatinases (MMP-2 and MMP-9) are oppositely regulated in GCA with MMP-9 elevated and MMP-2 decreased compared to HBDs (Table 2). We also confirmed this at the mRNA expression level from TAB tissue [16]. MMPs could play important roles in GCA vasculopathy progression, however are also beneficial players in angiogenesis, wound healing, and regeneration in aortic aneurysms, as well as in neointimal hyperplasia [43]. This complexity is reflected in our data, as MMP-2 shows positive association with jaw claudication and negative association with relapse (Table 3) [16]. A solid role of MMPs in GCA patients is indicated by the following: (a) protein C, a potential activator of gelatinases, is itself upregulated in GCA (Table 2); (b) MMP-9 is positioned within the same cluster as MMP-1 and MMP-2 (Fig. 2a); and (c) MMP-2 is positioning directly opposite all other analytes in PCA (Fig. 3).
We also report on significantly elevated levels of chitinase-3-like protein 1 (CHI3L1) and tenascin C (TNC), an extracellular matrix glycoprotein (Table 2), located within the same cluster in the heatmap (Fig. 2a). They could, alongside with MMPs, shed light on matrix restructuring of vessels in GCA. Johansen et al. characterized CHI3L1 in GCA, with elevated serum concentrations in 19 GCA patients and gene expression found in CD68+ giant cells and mononuclear cells in the media [44]. TNC is especially interesting due to the following reasons: (a) the large isoform of TNC was found to contain alternatively spliced domains with cleavage sites for MMPs, making TNC their natural substrate [45]; (b) MMPs were reported to be linked to induction of TNC [45]; and (c) TNC could be capable of activating TLR-4, potentially conveying signals from the missing “unknown infectious agent” in GCA.
Additionally, we measured serum levels of macrophage receptor with collagenous structure (MARCO), reported by Rodríguez-Pla et al. [46] as exhibiting elevated gene expression levels in the TAB of a GCA patient. Our findings suggest a positive association of MARCO serum levels in GCA patients with jaw claudication and negative association of MARCO with limb artery involvement (Table 3).
Until now, there have been few reports on serological studies using multiplex analysis in GCA vs. HBD [17, 40]. Van der Geest et al. [17] showed significantly changed levels of CXCL9, IL-6, IL-10, sIL-2R, CCL2, and CCL11 between 12 GCA patients and 13 HBDs, while Terrier et al. [40] reported on significantly changed levels of M-CSF, IL-1 beta, IL-6, IL-12, IFN-gamma, TNF-alpha, and IL-17A in GCA vs. HBDs. Both groups measured a small number of analytes in relatively few patients and HBDs.
We considered the 27 analytes measured in our cohort as a dynamic network and observed their interconnections. Evident and distinct physiological clustering was shown for GCA patients and HBDs, with the former showing just one positively associated cluster, while the latter showed two positive and one negative cluster (Fig. 1). Partitioning the analytes based on maximizing within-group similarities in unsupervised hierarchical clustering yielded a clear separation of GCA patients and HBDs, resulting in three distinct analyte clusters (Fig. 2a). A STRING search (which reports on interactions from the literature and experimental data) on the 27 analytes showed evidence of closer interactions between those analytes, which were grouped together in our cluster analysis (Fig. 2b). Further individual analysis of the analytes in the three clusters (Fig. 2c–e) revealed important common processes between analytes in each cluster, namely strongest association to positive regulation of cytokine production and T cell proliferation in cluster C2, as an example (Fig. 2d). The different patterns found between unsupervised hierarchical clustering (Fig. 2a) and PCA (Fig. 3) are due to the fact that the clustering algorithm divides samples into homogenous groups with largest within-group similarity, while PCA filters data with weakest signals discarded in order to obtain patterns encoding the highest variance. Importantly, the three GCA patients, who fell into the HBD cluster (Fig. 2a) and/or exhibited analyte profiles more similar to those of HBDs (Fig. 3), will be monitored closely for future signs of either remission or milder course of the disease.
As this is an exploratory analysis, correction for multiple testing would not strictly be required [47]. Nevertheless, in our study, aCL IgG was the only statistically significant analyte after multiple testing and was found associated with limb artery involvement (Table 3). It will be relevant to monitor aCL IgG in a larger group of GCA patients (replication cohort) and follow their clinical progression, along with complications.
Taken together, serological markers for GCA will be sought after, since non-invasive diagnostics is becoming more prevalent. We highlight the importance of using groups of serological analytes, specifically acute phase parameters (e.g., SAA, CRP, haptoglobin, ESR), MMPs (MMP-1 and MMP-2), and cytokines (TNF-alpha) for predicting GCA complications, such as relapse and visual disturbances. PCA analysis revealed TNF R1, CHI3L1, TNC, IL-1 beta, IL-18, and MMP-2 to be the main contributors to the separation of GCA patients from HBDs, rendering them also promising biomarker candidates. The study needs to be further validated and confirmed. In the future, it will be crucial to continue monitoring GCA patients in long term and build prediction models for GCA relapses and complications, contributing substantially to personalized disease management.
References
Hunder GG, Bloch DA, Michel BA, Stevens MB, Arend WP, Calabrese LH, Edworthy SM, Fauci AS, Leavitt RY, Lie JT (1990) The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum 33(8):1122–1128
Nesher G (2008) Giant cell arteritis. In: Shoenfeld Y, Cervera R, Gershwin ME (eds) Diagnostic criteria in autoimmune diseases. Humana Press, Totowa, pp 73–76. https://doi.org/10.1007/978-1-60327-285-8_13
Luqmani R, Lee E, Singh S, Gillett M, Schmidt WA, Bradburn M, Dasgupta B, Diamantopoulos AP, Forrester-Barker W, Hamilton W, Masters S, McDonald B, McNally E, Pease C, Piper J, Salmon J, Wailoo A, Wolfe K, Hutchings A (2016) The role of ultrasound compared to biopsy of temporal arteries in the diagnosis and treatment of giant cell arteritis (TABUL): a diagnostic accuracy and cost-effectiveness study. Health Technol Assess 20(90):1–238. https://doi.org/10.3310/hta20900
González-Gay MA, Pina T, Prieto-Peña D, Calderon-Goercke M, Blanco R, Castañeda S (2018) Current and emerging diagnosis tools and therapeutics for giant cell arteritis. Expert Rev Clin Immunol 14:593–605. https://doi.org/10.1080/1744666X.2018.1485491
Hocevar A, Rotar Z, Jese R, Semrl SS, Pizem J, Hawlina M, Tomsic M (2016) Do early diagnosis and glucocorticoid treatment decrease the risk of permanent visual loss and early relapses in giant cell arteritis: a prospective longitudinal study. Medicine (Baltimore) 95(14):e3210. https://doi.org/10.1097/MD.0000000000003210
Diamantopoulos AP, Haugeberg G, Lindland A, Myklebust G (2016) The fast-track ultrasound clinic for early diagnosis of giant cell arteritis significantly reduces permanent visual impairment: towards a more effective strategy to improve clinical outcome in giant cell arteritis? Rheumatology (Oxford) 55(1):66–70. https://doi.org/10.1093/rheumatology/kev289
Patil P, Williams M, Maw WW, Achilleos K, Elsideeg S, Dejaco C, Borg F, Gupta S, Dasgupta B (2015) Fast track pathway reduces sight loss in giant cell arteritis: results of a longitudinal observational cohort study. Clin Exp Rheumatol 33(2 Suppl 89):S-103–S-106
De Smit E, Palmer AJ, Hewitt AW (2015) Projected worldwide disease burden from giant cell arteritis by 2050. J Rheumatol 42(1):119–125. https://doi.org/10.3899/jrheum.140318
Hazleman B (2000) Laboratory investigations useful in the evaluation of polymyalgia rheumatica (PMR) and giant cell arteritis (GCA). Clin Exp Rheumatol 18(4 Suppl 20):S29–S31
Coll-Vinent B, Vilardell C, Font C, Oristrell J, Hernández-Rodríguez J, Yagüe J, Urbano-Márquez A, Grau JM, Cid MC (1999) Circulating soluble adhesion molecules in patients with giant cell arteritis. Correlation between soluble intercellular adhesion molecule-1 (sICAM-1) concentrations and disease activity. Ann Rheum Dis 58(3):189–192
Weyand CM, Goronzy JJ (2003) Medium- and large-vessel vasculitis. N Engl J Med 349(2):160–169. https://doi.org/10.1056/NEJMra022694
Remahl AI, Bratt J, Möllby H, Nordborg E, Waldenlind E (2008) Comparison of soluble ICAM-1, VCAM-1 and E-selectin levels in patients with episodic cluster headache and giant cell arteritis. Cephalalgia 28(2):157–163. https://doi.org/10.1111/j.1468-2982.2007.01487.x
Visvanathan S, Rahman MU, Hoffman GS, Xu S, García-Martínez A, Segarra M, Lozano E, Espígol-Frigolé G, Hernández-Rodríguez J, Cid MC (2011) Tissue and serum markers of inflammation during the follow-up of patients with giant-cell arteritis—a prospective longitudinal study. Rheumatology (Oxford) 50(11):2061–2070. https://doi.org/10.1093/rheumatology/ker163
Baldini M, Maugeri N, Ramirez GA, Giacomassi C, Castiglioni A, Prieto-González S, Corbera-Bellalta M, Comite GD, Papa I, Dell'antonio G, Ammirati E, Cuccovillo I, Vecchio V, Mantovani A, Rovere-Querini P, Sabbadini MG, Cid MC, Manfredi AA (2012) Selective up-regulation of the soluble pattern-recognition receptor pentraxin 3 and of vascular endothelial growth factor in giant cell arteritis: relevance for recent optic nerve ischemia. Arthritis Rheum 64(3):854–865. https://doi.org/10.1002/art.33411
van der Geest KS, Abdulahad WH, Chalan P, Rutgers A, Horst G, Huitema MG, Roffel MP, Roozendaal C, Kluin PM, Bos NA, Boots AM, Brouwer E (2014) Disturbed B cell homeostasis in newly diagnosed giant cell arteritis and polymyalgia rheumatica. Arthritis Rheumatol 66(7):1927–1938. https://doi.org/10.1002/art.38625
Lakota K, Tadeja K, Žigon P, Rotar Ž, Tomšič M, Čučnik S, SodinŠemrl S, Hočevar A (2015) Biomarkers in temporal artery biopsies and sera of patients with giant cell arteritis. Arthritis Rheumatol. https://acrabstracts.org/abstract/biomarkers-in-temporal-artery-biopsies-and-sera-of-patients-with-giant-cell-arteritis/. Accessed 17 August 2018
van der Geest KS, Abdulahad WH, Rutgers A, Horst G, Bijzet J, Arends S, Roffel MP, Boots AM, Brouwer E (2015) Serum markers associated with disease activity in giant cell arteritis and polymyalgia rheumatica. Rheumatology (Oxford) 54(8):1397–1402. https://doi.org/10.1093/rheumatology/keu526
Sorbi D, French DL, Nuovo GJ, Kew RR, Arbeit LA, Gruber BL (1996) Elevated levels of 92-kd type IV collagenase (matrix metalloproteinase 9) in giant cell arteritis. Arthritis Rheum 39(10):1747–1753
Weyand CM, Fulbright JW, Hunder GG, Evans JM, Goronzy JJ (2000) Treatment of giant cell arteritis: interleukin-6 as a biologic marker of disease activity. Arthritis Rheum 43(5):1041–1048. https://doi.org/10.1002/1529-0131(200005)43:5<1041::AID-ANR12>3.0.CO;2-7
Cid MC, Font C, Oristrell J, de la Sierra A, Coll-Vinent B, López-Soto A, Vilaseca J, Urbano-Márquez A, Grau JM (1998) Association between strong inflammatory response and low risk of developing visual loss and other cranial ischemic complications in giant cell (temporal) arteritis. Arthritis Rheum 41(1):26–32. https://doi.org/10.1002/1529-0131(199801)41:1<26::AID-ART4>3.0.CO;2-0
Burja B, Kuret T, Sodin-Semrl S, Lakota K, Rotar Ž, Ješe R, Mrak-Poljsak K, Žigon P, Thallinger GG, Feichtinger J, Čučnik S, Tomšič M, Praprotnik S, Hocevar A (2017) A concise review of significantly modified serological biomarkers in giant cell arteritis, as detected by different methods. Autoimmun Rev 17:188–194. https://doi.org/10.1016/j.autrev.2017.11.022
Hernández-Rodríguez J, Segarra M, Vilardell C, Sánchez M, García-Martínez A, Esteban MJ, Grau JM, Urbano-Márquez A, Colomer D, Kleinman HK, Cid MC (2003) Elevated production of interleukin-6 is associated with a lower incidence of disease-related ischemic events in patients with giant-cell arteritis: angiogenic activity of interleukin-6 as a potential protective mechanism. Circulation 107(19):2428–2434. https://doi.org/10.1161/01.CIR.0000066907.83923.32
Grossman C, Barshack I, Koren-Morag N, Ben-Zvi I, Bornstein G (2017) Risk factors for severe cranial ischaemic events in patients with giant cell arteritis. Clin Exp Rheumatol 35 Suppl 103(1):88–93
Ponte C, Rodrigues AF, O'Neill L, Luqmani RA (2015) Giant cell arteritis: current treatment and management. World J Clin Cases 3(6):484–494. https://doi.org/10.12998/wjcc.v3.i6.484
Ashima M, Eric ML (2012) Utility of C-reactive protein in the diagnosis of giant cell arteritis: better than the erythrocyte sedimentation rate? Int J Clin Rheumatol 7(3):1
Kermani TA, Warrington KJ, Cuthbertson D, Carette S, Hoffman GS, Khalidi NA, Koening CL, Langford CA, Maksimowicz-McKinnon K, McAlear CA, Monach PA, Seo P, Merkel PA, Ytterberg SR, Consortium VCR (2015) Disease relapses among patients with giant cell arteritis: a prospective, longitudinal cohort study. J Rheumatol 42(7):1213–1217. https://doi.org/10.3899/jrheum.141347
R Core Team (2017) A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc B (Methodol) 57:289–300
Szklarczyk D, Morris JH, Cook H, Kuhn M, Wyder S, Simonovic M, Santos A, Doncheva NT, Roth A, Bork P, Jensen LJ, von Mering C (2017) The STRING database in 2017: quality-controlled protein-protein association networks, made broadly accessible. Nucleic Acids Res 45(D1):D362–D368. https://doi.org/10.1093/nar/gkw937
Stone JH, Tuckwell K, Dimonaco S, Klearman M, Aringer M, Blockmans D, Brouwer E, Cid MC, Dasgupta B, Rech J, Salvarani C, Schett G, Schulze-Koops H, Spiera R, Unizony SH, Collinson N (2017) Trial of Tocilizumab in giant-cell arteritis. N Engl J Med 377(4):317–328. https://doi.org/10.1056/NEJMoa1613849
Gloor AD, Yerly D, Adler S, Reichenbach S, Kuchen S, Seitz M, Villiger PM (2018) Immuno-monitoring reveals an extended subclinical disease activity in tocilizumab-treated giant cell arteritis. Rheumatology (Oxford). https://doi.org/10.1093/rheumatology/key158
Prieto-González S, Terrades-García N, Corbera-Bellalta M, Planas-Rigol E, Miyabe C, Alba MA, Ponce A, Tavera-Bahillo I, Murgia G, Espígol-Frigolé G, Marco-Hernández J, Hernández-Rodríguez J, García-Martínez A, Unizony SH, Cid MC (2017) Serum osteopontin: a biomarker of disease activity and predictor of relapsing course in patients with giant cell arteritis. Potential clinical usefulness in tocilizumab-treated patients. RMD Open 3(2):e000570. https://doi.org/10.1136/rmdopen-2017-000570
Conway R, O'Neill L, Gallagher P, McCarthy GM, Murphy CC, Veale DJ, Fearon U, Molloy ES (2018) Ustekinumab for refractory giant cell arteritis: a prospective 52-week trial. Semin Arthritis Rheum. https://doi.org/10.1016/j.semarthrit.2018.04.004
Kuret T, Lakota K, Mali P, Čučnik S, Praprotnik S, Tomšič M, Sodin-Semrl S (2018) Naturally occurring antibodies against serum amyloid A reduce IL-6 release from peripheral blood mononuclear cells. PLoS One 13(4):e0195346. https://doi.org/10.1371/journal.pone.0195346
O'Neill L, Rooney P, Molloy D, Connolly M, McCormick J, McCarthy G, Veale DJ, Murphy CC, Fearon U, Molloy E (2015) Regulation of inflammation and angiogenesis in giant cell arteritis by acute-phase serum amyloid A. Arthritis Rheumatol 67(9):2447–2456. https://doi.org/10.1002/art.39217
Žigon P, Lakota K, Kuret T, Tomšič M, Čučnik S, Sodin-Šemrl S, Hočevar A (2016) Acute phase proteins and interleukin-6 are important in distinguishing between giant cell arteritis positive and negative patients. In: 10th international congress on autoimmunity, Leipzig. Autoimmunity
Deng J, Younge BR, Olshen RA, Goronzy JJ, Weyand CM (2010) Th17 and Th1 T-cell responses in giant cell arteritis. Circulation 121(7):906–915. https://doi.org/10.1161/CIRCULATIONAHA.109.872903
Weyand CM, Younge BR, Goronzy JJ (2011) IFN-γ and IL-17: the two faces of T-cell pathology in giant cell arteritis. Curr Opin Rheumatol 23(1):43–49. https://doi.org/10.1097/BOR.0b013e32833ee946
Samson M, Corbera-Bellalta M, Audia S, Planas-Rigol E, Martin L, Cid MC, Bonnotte B (2017) Recent advances in our understanding of giant cell arteritis pathogenesis. Autoimmun Rev 16:833–844. https://doi.org/10.1016/j.autrev.2017.05.014
Terrier B, Geri G, Chaara W, Allenbach Y, Rosenzwajg M, Costedoat-Chalumeau N, Fouret P, Musset L, Benveniste O, Six A, Klatzmann D, Saadoun D, Cacoub P (2012) Interleukin-21 modulates Th1 and Th17 responses in giant cell arteritis. Arthritis Rheum 64(6):2001–2011. https://doi.org/10.1002/art.34327
Annunziato F, Romagnani C, Romagnani S (2015) The 3 major types of innate and adaptive cell-mediated effector immunity. J Allergy Clin Immunol 135(3):626–635. https://doi.org/10.1016/j.jaci.2014.11.001
Samson M, Ghesquière T, Berthier S, Bonnotte B (2017) Ustekinumab inhibits Th1 and Th17 polarisation in a patient with giant cell arteritis. Ann Rheum Dis 77:e6. https://doi.org/10.1136/annrheumdis-2017-211622
Siefert SA, Sarkar R (2012) Matrix metalloproteinases in vascular physiology and disease. Vascular 20(4):210–216. https://doi.org/10.1258/vasc.2011.201202
Johansen JS, Baslund B, Garbarsch C, Hansen M, Stoltenberg M, Lorenzen I, Price PA (1999) YKL-40 in giant cells and macrophages from patients with giant cell arteritis. Arthritis Rheum 42(12):2624–2630. https://doi.org/10.1002/1529-0131(199912)42:12<2624::AID-ANR17>3.0.CO;2-K
Midwood KS, Hussenet T, Langlois B, Orend G (2011) Advances in tenascin-C biology. Cell Mol Life Sci 68(19):3175–3199. https://doi.org/10.1007/s00018-011-0783-6
Rodríguez-Pla A, Martínez-Murillo F, Savino PJ, Eagle RC, Seo P, Soloski MJ (2009) MMP-12, a novel matrix metalloproteinase associated with giant cell arteritis. Rheumatology (Oxford) 48(11):1460–1461. https://doi.org/10.1093/rheumatology/kep271
Bender R, Lange S (2001) Adjusting for multiple testing—when and how? J Clin Epidemiol 54(4):343–349
Acknowledgements
This work was supported by the Slovenian Research Agency for the National Research Program P3-0314 to SSS and from the Austrian Ministry of Science, Research and Economy (HSRSM project OMICS Center Graz to GGT). We would like to acknowledge Biomedica Gruppe/Biomedis MB for kindly providing the AtheNa Multi-Lyte Luminex xMAP Technology needed to perform the Luminex experiments. The authors thank the laboratory staff of the Immunology Laboratory and the nursing staff of the Clinical Department of Rheumatology, University Medical Center Ljubljana, for their continual support. None of the authors have any competing interests, and all of the authors have read the journal’s policy on conflict of interest and journal’s authorship agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval no. 99/04/15 for the Giant Cell Arteritis study was obtained from the Slovenian National Medical Ethics Committee. All patients provided written informed consent to participate in the study. We confirm that all experiments were performed in accordance with relevant guidelines and regulations.
Disclosures
None.
Additional information
Rheumatology in Slovenia: Clinical practice and translational research
Electronic supplementary material
Supplementary Table I
(PDF 297 kb)
Supplementary Figure 1
(DOCX 128 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Burja, B., Feichtinger, J., Lakota, K. et al. Utility of serological biomarkers for giant cell arteritis in a large cohort of treatment-naïve patients. Clin Rheumatol 38, 317–329 (2019). https://doi.org/10.1007/s10067-018-4240-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-018-4240-x