Abstract
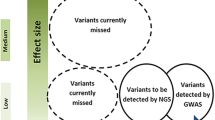
In the last two decades, migraine research has greatly advanced our current knowledge of the genetic contributions and the pathophysiology of this common and debilitating disorder. Nonetheless, this knowledge still needs to grow further and to translate into more effective treatments. To date, several genes involved in syndromic and monogenic forms of migraine have been identified, allowing the generation of animal models which have significantly contributed to current knowledge of the mechanisms underlying these rare forms of migraine. Common forms of migraine are instead posing a greater challenge, as they may most often stem from complex interactions between multiple common genetic variants, with environmental triggers. This paper reviews our current understanding of migraine genetics, moving from syndromic and monogenic forms to oligogenic/polygenic migraines most recently addressed with some success through genome-wide association studies. Methodological issues in study design and future perspectives opened by biomarker research will also be briefly addressed.
Similar content being viewed by others
References
Headache Classification Committee of the International Headache Society (IHS) (2013) The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 33:629–808
Bigal ME, Lipton RB (2009) The epidemiology, burden, and comorbidities of migraine. Neurol Clin 27:321–334
Robbins MS, Lipton RB (2010) The epidemiology of primary headache disorders. Semin Neurol 30:107–109
Noseda R, Burstein R (2013) Migraine pathophysiology: anatomy of the trigeminovascular pathway and associated neurological symptoms, CSD, sensitization and modulation of pain. Pain 154(Suppl 1)
Eikermann-Haerter K, Moskowitz MA (2008) Animal models of migraine headache and aura. Curr Opin Neurol 21:294–300
Mulder EJ, van Baal C, Gaist D et al (2003) Genetic and environmental influences on migraine: a twin study across six countries. Twin Res 6:422–431
Svensson DA, Larsson B, Waldenlind E, Pedersen NL (2003) Shared rearing environment in migraine: results from twin reared apart and twin reared together. Headache 43:235–244
Cologno D, Pascale AD, Manzoni GC (2003) Familial occurrence of migraine with aura in a population-based study. Headache 43:231–234
Schürks M, Rist PM, Kurth T (2010) Sex hormone receptor gene polymorphisms and migraine: a systematic review and meta-analysis. Cephalalgia 30:1306–1328
Russel MB, Iselius L, Olesen J (1996) Migraine without aura and migraine with aura are inherited disorders. Cephalalgia 16:305–309
Lemos C, Alonso I, Barros J et al (2012) Assessing risk factors for migraine: differences in gender transmission. PLoS One 7:e50626
Peltonen L, GenomEUtwin (2003) GenomEUtwin: a strategy to identify genetic influences on health and disease. Twin Res 6:354–360
Friedman DI, De ver Dye T (2009) Migraine and the environment. Headache 49:941–952
Eising E, Datson NA, van den Maagdenberg AMJM, Ferrari MD (2013) Epigenetic mechanisms in migraine: a promising avenue? BMC Med 11:26–32
Diener HC, Kuper M, Kurth T (2008) Migraine-associated risks and comorbidity. J Neurol 255:1290–1301
Bellini B, Arruda M, Cescut A et al (2013) Headache and comorbidity in children and adolescents. J Headache Pain 14:79–86
Hung CI, Liu CY, Juang YY, Wang SJ (2006) The impact of migraine on patients with major depressive disorder. Headache 46:469–477
Tietjen GE, Brandes JL, Digre KB et al (2007) High prevalence of somatic symptoms and depression in women with disabling chronic headache. Neurology 68:134–140
Joutel A, Corpechot C, Ducros A et al (1996) Notch-3 mutations in CADASIL, a hereditary adult-onset condition causing stroke and dementia. Nature 383:707–710
Federico A, Bianchi S, Dotti MT (2005) The spectrum of mutations for CADASIL diagnosis. Neurol Sci 26:117–124
Ungaro C, Mazzei R, Conforti FL et al (2009) CADASIL: extended polymorphisms and mutational analysis of the NOTCH3 gene. J Neurosci Res 87:1162–1167
Mosca L, Marazzi R, Ciccone A et al (2011) NOTCH3 gene mutations in subjects clinically suspected of CADASIL. J Neurol Sci 307:144–148
Ragno M, Fabrizi GM, Cacchiò G et al (2006) Two novel Italian CADASIL families from Central Italy with mutation CGC-TGC at codon 1006 in the exon 19 Notch3 gene. Neurol Sci 27:252–256
Valenti R, Bianchi S, Pescini F et al (2011) First report of a pathogenic mutation on exon 24 of the NOTCH3 gene in a CADASIL family. J Neurol 258:1632–1636
Razvi SS, Davidson R, Bone I, Muir KW (2005) The prevalence of cerebral autosomal dominant arteriopathy with subcortical infarcts and leucoencephalopathy (CADASIL) in the west of Scotland. J Neurol Neurosurg Psychiatry 76:739–741
Narayan SK, Gorman G, Kalaria RN et al (2012) The minimum prevalence of CADASIL in Northeast England. Neurology 78:1025–1027
Iso T, Hamamori Y, Kedes L (2003) Notch signaling in vascular development. Arterioscler Thromb Vasc Biol 23:543–553
Alva JA, Iruela-Arispe ML (2004) Notch signaling in vascular morphogenesis. Curr Opin Hematol 11:278–283
Ishiko A, Shimizu A, Nagata E et al (2006) Notch3 ectodomain is a major component of granular osmiophilic material (GOM) in CADASIL. Acta Neuropathol 112:333–339
Liem MK, Oberstein SA, van der Grond J et al (2010) CADASIL and migraine: a narrative review. Cephalalgia 30:1284–1289
Dichgans M, Mayer M, Uttner I et al (1998) The phenotypic spectrum of CADASIL: clinical findings in 102 cases. Ann Neurol 44:731–739
Kaufmann P, Engelstad K, Wei Y et al (2011) Natural history of MELAS associated with mitochondrial DNA m.3243A > G genotype. Neurology 77:1965–1971
Finsterer J (2012) Inherited mitochondrial disorders. Adv Exp Med Biol 942:187–213
Federico A, Di Donato I, Bianchi S et al (2012) Hereditary cerebral small vessel diseases: a review. J Neurol Sci 322:25–30
Ophoff RA, DeYoung J, Service SK et al (2001) Hereditary vascular retinopathy, cerebroretinal vasculopathy, and hereditary endotheliopathy with retinopathy, nephropathy, and stroke map to a single locus on chromosome 3p21.1-p21.3. Am J Hum Genet 69:447–453
Bersano A, Debette S, Zanier ER et al (2012) The genetics of small-vessel disease. Curr Med Chem 19:4124–4141
Storimans CW, Van Schooneveld MJ, Oosterhuis JA, Bos PJ (1991) A new autosomal dominant vascular retinopathy syndrome. Eur J Ophthalmol 1:73–78
Terwindt GM, Haan J, Ophoff RA et al (1998) Clinical and genetic analysis of a large Dutch family with autosomal dominant vascular retinopathy, migraine and Raynaud's phenomenon. Brain 121(Pt 2):303–316
Jen J, Cohen AH, Yue Q et al (1997) Hereditary endotheliopathy with retinopathy, nephropathy, and stroke (HERNS). Neurology 49:1322–1330
Winkler DT, Lyrer P, Probst A et al (2008) Hereditary systemic angiopathy (HSA) with cerebral calcifications, retinopathy, progressive nephropathy, and hepatopathy. J Neurol 255:77–88
Di Francesco JC, Novara F, Zuffardi O, et al. (2014) TREX1 C-terminal frameshift mutations in the systemic variant of retinal vasculopathy with cerebral leukodystrophy. Neurol Sci
Gould DB, Phalan FC, Breedved GJ et al (2005) Mutations in COL4A1 cause perinatal cerebral hemorrhage and porencephaly. Science 308:1167–1171
Breedved G, de Coo IF, Lequin MH et al (2006) Novel mutations in three families confirms a major role of COL4A1 in hereditary porencephaly. J Med Genet 43:490–495
Van Der Knaap MS, Smit LM, Barkhof F et al (2006) Neonatal porencephaly and adult stroke related to mutations in collagen IV A1. Ann Neurol 59:504–511
Lanfranconi S, Markus HS (2010) COL4A1 mutations as a monogenic cause of cerebral small vessel disease: a systematic review. Stroke 41:e513–e518
Vahedi K, Massin P, Guichard JP et al (2003) Hereditary infantile hemiparesis, retinal arteriolar tortuosity, and leukoencephalopathy. Neurology 60:57–63
Ebisawa T (2007) Circadian rhythms in the CNS and peripheral clock disorders: human sleep disorders and clock genes. J Pharmacol Sci 103:150–154
Vanselow K, Vanselow JT, Westermark PO et al (2006) Differential effects of PER2 phosphorylation: molecular basis for the human familial advanced sleep phase syndrome (FASPS). Genes Dev 20:2660–2672
Brennan KC, Bates EA, Shapiro RE et al (2013) Casein kinase I mutations in familial migraine and advanced sleep phase. Sci Transl Med 5(183ra56):1–11
Xu Y, Padiath QS, Shapiro RE et al (2005) Functional consequences of a CKIδ mutation causing familial advanced sleep phase syndrome. Nature 434:640–644
Hansen JM (2010) Familial hemiplegic migraine. Dan Med Bull 57:B4183
Thomsen LL, Kirchmann M, Bjornsson A et al (2007) The genetic spectrum of a population-based sample of familial hemiplegic migraine. Brain 130(Pt 2):346–356
Riant F, Ducros A, Ploton C et al (2010) De novo mutations in ATP1A2 and CACNA1A are frequent in early-onset sporadic hemiplegic migraine. Neurology 75:967–972
Ophoff RA, Terwindt GM, Vergouwe MN et al (1996) Familial hemiplegic migraine and episodic ataxia type-2 are caused by mutations in the Ca2+ channel gene CACNL1A4. Cell 87:543–552
Ambrosini A, D’Onofrio M, Grieco G et al (2005) Familial basilar migraine associated with a new mutation in ATP1A2 gene. Neurology 65:1826–1828
Todt U, Dichgans M, Jurkat-Rott K et al (2005) Rare missense variants in ATP1A2 in families with clustering of common forms of migraine. Hum Mutat 26:315–321
Vanmolkot KR, Babini E, de Vries B et al (2007) The novel pL1649Q mutation in the SCN1A epilepsy gene associated with familial hemiplegic migraine: genetic and functional studies. Hum Mutat 28:522
Cestèle S, Scalmani P, Rusconi R et al (2008) Self-limited hyperexcitability: functional effect of a familial hemiplegic migraine mutation of the Nav1.1 (SCN1A) Na+ channel. J Neurosci 28:7273–7283
Dale RC, Gardiner A, Antony J, Hulden H (2012) Familial PRRT2 mutation with heterogeneous paroxysmal disorders including paroxysmal torticollis and hemiplegic migraine. Dev Med Child Neurol 54:958–960
Suzuki M, Van Paesschen W, Stalmans I et al (2010) Defective membrane expression of the Na(+)-HCO3(−) cotrasporter NBCe1 is associated with familial migraine. Proc Natl Acad Sci U S A 107:15963–15968
Jen JC, Wan J, Palos TP et al (2005) Mutation in the glutamate transporter EAAT1 causes episodic ataxia, hemiplegia, and seizures. Neurology 65:529–534
de Vries B, Mamsa H, Stam AH et al (2009) Episodic ataxia associated with EAAT1 mutation C186S affecting glutamate reuptake. Arch Neurol 66:97–101
Frosk P, Mhanni AA, Rafay MF (2013) SCN1A mutation associated with intractable myoclonic epilepsy and migraine headache. J Child Neurol 28:389–391
Gargus JJ, Tournay A (2007) Novel mutation confirms seizure locus SCN1A is also familial hemiplegic migraine locus FHM3. Pediatr Neurol 37:407–410
O'Roak BJ, Deriziotis P, Lee C et al (2011) Exome sequencing in sporadic autism spectrum disorders identifies severe de novo mutations. Nat Genet 43:585–589
Barros J, Ruano L, Domingos J et al (2014) The prevalence of familial hemiplegic migraine with cerebellar ataxia and spinocerebellar ataxia type 6 in Portugal. Headache 54:911–915
Bürk K, Kaiser FJ, Tennstedt S et al (2014) A novel missense mutation in CACNA1A evaluated by in silico protein modeling is associated with non-episodic spinocerebellar ataxia with slow progression. Eur J Med Genet 57:207–211
Star TV, Pristay W, Snutch TP (1991) Primary structure of a calcium channel that is highly expressed in the rat cerebellum. Proc Natl Acad Sci U S A 88:5621–5625
Westenbroek RE, Sakurai T, Elliot EM (1995) Immunochemical identification and subcellular distribution of the alpha 1A subunits of brain calcium channels. J Neurosci 15:6403–6418
Cohen-Kutner M, Nachmanni D, Atlas D (2010) CaV2.1 (P/Q channel) interaction with synaptic proteins is essential for depolarization-evoked release. Channels (Austin) 4:266–277
Van Den Magdemberg AM, Pietrobon D, Pizzorusso T et al (2004) A Cacna1A knockin migraine mouse model with increased susceptibility to cortical spreading depression. Neuron 41:701–710
Eikermann-Haerter K, Yuzawa I, Qin T et al (2011) Enhanced subcortical spreading depression in familial hemiplegic migraine type 1 mutant mice. J Neurosci 31:5755–5763
Eikermann-Haerter K, Dileköz E, Kudo C et al (2009) Genetic and hormonal factors modulate spreading depression and transient hemiparesis in mouse models of familial hemiplegic migraine type 1. J Clin Invest 119:99–109
Hedrich UB, Liautard C, Kirschenbaum D et al (2014) Impaired action potential initiation in GABAergic interneurons causes hyperexcitable networks in an epileptic mouse model carrying a human NaV1.1 mutation. J Neurosci 34:14874–14889
Escayg A, Goldin AL (2010) Sodium channel SCN1A and epilepsy: mutations and mechanisms. Epilepsia 51:1650–1658
Maher BH, Griffiths LR (2011) Identification of molecular genetic factors that influence migraine. Mol Genet Genomics 285:433–446
Corominas R, Sobrido MJ, Ribasés M et al (2010) Association study of the serotoninergic system in migraine in the Spanish population. Am J Med Genet B Neuropsychiatr Genet 153B:177–184
Ishii M, Shimizu S, Sakairi Y et al (2012) MAOA, MTHFR, and TNF-β genes polymorphisms and personality traits in the pathogenesis of migraine. Mol Cell Biochem 363:357–366
Borroni B, Brambilla C, Liberini P et al (2005) Functional serotonin 5-HTTLPR polymorphism is a risk factor for migraine with aura. J Headache Pain 6:182–184
Bayerer B, Engelbergs J, Savidou I et al (2010) Single nucleotide polymorphisms of the serotonin transporter gene in migraine—an association study. Headache 50:319–322
Lea RA, Dohy A, Jordan K et al (2000) Evidence for allelic association of the dopamine beta-hydroxylase gene (DBH) with susceptibility to typical migraine. Neurogenetics 3:35–40
Fernandez F, Lea RA, Colson NJ, Bellis C et al (2006) Association between a 19 bp deletion polymorphism at the dopamine beta-hydroxylase (DBH) locus and migraine with aura. J Neurol Sci 251:118–123
Fernandez F, Colson N, Quinlan S et al (2009) Association between migraine and a functional polymorphism at the dopamine beta-hydroxylase locus. Neurogenetics 10:199–208
Todt U, Netzer C, Toliat M et al (2009) New genetic evidence for involvement of the dopamine system in migraine with aura. Hum Genet 125:265–279
Corominas R, Ribases M, Camina M et al (2009) Two-stage case control association study of dopamine-related genes and migraine. BMC Med Genet 10:95
Ghosh J, Pradhan S, Mittal B (2011) Role of dopaminergic gene polymorphisms (DBH 19 bp indel and DRD2 Nco I) in genetic susceptibility to migraine in North Indian population. Pain Med 12:1109–1111
Ghosh J, Pradhan S, Mittal B (2013) Identification of a novel ANKK1 and other dopaminergic (DRD2 and DBH) gene variants in migraine susceptibility. Neuromol Med 15:61–73
Mochi M, Cevoli S, Cortelli P et al (2003) A genetic association study of migraine with dopamine receptor 4, dopamine transporter and dopamine-beta-hydroxylase genes. Neurol Sci 23:301–305
Formicola D, Aloia A, Sampaolo S et al (2010) Common variants in the regulative regions of GRIA1 and GRIA3 receptor genes are associated with migraine susceptibility. BMC Med Genet 25:103
Maher BH, Lea RA, Follett J et al (2013) Association of a GRIA3 gene polymorphism with migraine in an Australian case–control cohort. Headache 53:1245–1249
Paterna S, Di Pasquale P, Cottone C et al (1997) Migraine without aura and ACE-gene deletion polymorphism: is there a correlation? Preliminary findings. Cardiovasc Drugs Ther 11:603–604
Kowa H, Fusayasu E, Ijiri T et al (2005) Association of the insertion/deletion polymorphism of the angiotensin I-converting enzyme gene in patients of migraine with aura. Neurosci Lett 374:129–131
Joshi G, Pradhan S, Mittal B (2009) Role of the ACE ID and MTHFR C677T polymorphisms in genetic susceptibility of migraine in a north Indian population. J Neurol Sci 277:133–137
Kowa H, Yasui K, Takeshima T et al (2000) The homozygous C677T mutation in the methylenetetrahydrofolate reductase gene is a genetic risk factor for migraine. Am J Med Genet 96:762–764
Kara I, Sazci A, Ergul E et al (2003) Association of the C677T and A1298C polymorphisms in the 5, 10 methylenetetrahydrofolate reductase gene in patients with migraine risk. Brain Res Mol Brain Res 111:84–90
Oterino A, Valle N, Bravo Y et al (2004) MTHFR T677 homozygosis influences the presence of aura in migraineurs. Cephalalgia 24:491–494
Lea RA, Ovcaric M, Sundholm J et al (2005) Genetic variants of angiotensin converting enzyme and methylenetetrahydrofolate reductase may act in combination to increase migraine susceptibility. Brain Res Mol Brain Res 136:112–117
Samaan Z, Gaysina D, Cohen-Woods S et al (2011) Methylenetetrahydrofolate reductase gene variant (MTHFR C677T) and migraine: a case control study and meta-analysis. BMC Neurol 11:66
An XK, Lu CX, Ma QL et al (2013) Association of MTHFR C677T polymorphism with susceptibility to migraine in the Chinese population. Neurosci Lett 549:78–81
Bahadir A, Eroz R, Dikici S (2013) Investigation of MTHFR C677T gene polymorphism, biochemical and clinical parameters in Turkish migraine patients: association with allodynia and fatigue. Cell Mol Neurobiol 33(8):1055–1063
Schwaag S, Evers S, Schirmacher A et al (2006) Genetic variants of the NOTCH3 gene in migraine—a mutation analysis and association study. Cephalalgia 26:158–161
Menon S, Cox HC, Kuwahata M et al (2010) Association of a Notch 3 gene polymorphism with migraine susceptibility. Cephalalgia 31:264–270
Tikka-Klemola P, Kaunisto MA, Hamalainen E et al (2009) Genetic association study of endothelin-1 and its receptors EDNRA and EDNRB in migraine with aura. Cephalalgia 29:1224–1231
Joshi G, Pradhan S, Mittal B (2011) Vascular gene polymorphisms (EDNRA −231 G > A and APOE HhaI) and risk for migraine. DNA Cell Biol 30:577–584
Lemos C, Neto JL, Pereira-Monteiro J et al (2011) A role for endothelin receptor type A in migraine without aura susceptibility? A study in Portuguese patients. Eur J Neurol 18:649–655
Tzourio C, El Amrani M, Poirier O et al (2001) Association between migraine and endothelin type A receptor (ETA −231 A/G) gene polymorphism. Neurology 56:1273–1277
Jia S, Ni J, Chen S et al (2011) Association of the pentanucleotide repeat polymorphism in NOS2 promoter region with susceptibility to migraine in a Chinese population. DNA Cell Biol 30:117–122
de OS Mansur T, Goncalves FM, Martins-Oliveira A et al (2012) Inducible nitric oxide synthase haplotype associated with migraine and aura. Mol Cell Biochem 364:303–308
Borroni B, Rao R, Liberini P et al (2006) Endothelial nitric oxide synthase (Glu298Asp) polymorphism is an independent risk factor for migraine with aura. Headache 46:1575–1579
Rainero I, Grimaldi LM, Salani G et al (2004) Association between the tumor necrosis factor-alpha −308 G/A gene polymorphism and migraine. Neurology 62:141–143
Mazaheri S, Hajilooi M, Rafiei A (2006) The G-308A promoter variant of the tumor necrosis factor-alpha gene is associated with migraine without aura. J Neurol 253:1589–1593
Ghosh J, Joshi G, Pradhan S, Mittal B (2010) Investigation of TNFA 308G > A and TNFB 252G > A polymorphisms in genetic susceptibility to migraine. J Neurol 257:898–904
Yilmaz IA, Ozge A, Erdal ME et al (2010) Cytokine polymorphism in patients with migraine: some suggestive clues of migraine and inflammation. Pain Med 11:492–497
Ates O, Kurt S, Altinisik J et al (2011) Genetic variations in tumor necrosis factor alpha, interleukin-10 genes, and migraine susceptibility. Pain Med 12:1464–1469
Trabace S, Brioli G, Lulli P et al (2002) Tumor necrosis factor gene polymorphism in migraine. Headache 42:341–345
Lee KA, Jang SY, Sohn KM et al (2007) Association between a polymorphism in the lymphotoxin-a promoter region and migraine. Headache 47:1056–1062
Asuni C, Stochino ME, Cherchi A et al (2009) Migraine and tumour necrosis factor gene polymorphism. An association study in a Sardinian sample. J Neurol 256:194–197
Dong W, Jia S, Ye X, Ni J (2012) Association analysis of TNFRSF1B polymorphism with susceptibility for migraine in the Chinese Han population. J Clin Neurosci 19:750–752
Rainero I, Fasano E, Rubino E et al (2005) Association between migraine and HLA-DRB1 gene polymorphisms. J Headache Pain 6:185–187
Dasdemir S, Cetinkaya Y, Gencer M et al (2013) Cox-2 gene variants in migraine. Gene 518:292–295
Lafrenière RG, Rouleau GA (2012) Identification of novel genes involved in migraine. Headache 52:107–110
Scher AI, Eiriksdottir G, Garcia M et al (2013) Lack of association between the MTHFR C677T variant and migraine with aura in an older population: could selective survival play a role? Cephalalgia 33:308–315
Liu R, Geng P, Ma M et al (2014) MTHFR C677T polymorphism and migraine risk: a meta-analysis. J Neurol Sci 336:68–73
Rubino E, Ferrero M, Rainero I et al (2009) Association of the C677T polymorphism in the MTHFR gene with migraine: a meta-analysis. Cephalalgia 29:818–825
MacClellan LR, Howard TD, Cole JW et al (2009) Relation of candidate genes that encode for endothelial function to migraine and stroke: the Stroke Prevention in Young Women study. Stroke 40:e550–e557
Pizza V, Bisogno A, Lamaida E et al (2010) Migraine and coronary artery disease: an open study on the genetic polymorphism of the 5,10 methylenetetrahydrofolate (MTHFR) and angiotensin I-converting enzyme (ACE) genes. Cent Nerv Syst Agents Med Chem 10:91–96
Colson NJ, Lea RA, Quinlan S, Griffiths LR (2006) The role of vascular and hormonal genes in migraine susceptibility. Mol Genet Metab 88:107–113
Stuart S, Cox HC, Lea RA, Griffiths LR (2012) The role of the MTHFR gene in migraine. Headache 52:515–520
Schürks M, Rist PM, Kurth T (2010) MTHFR 677C > T and ACE D/I polymorphisms in migraine: a systematic review and meta-analysis. Headache 50:588–599
Colson N, Fernandez F, Griffiths L (2010) Genetics of menstrual migraine: the molecular evidence. Curr Pain Headache Rep 14:389–395
Colson NJ, Lea RA, Quinlan S et al (2004) The estrogen receptor 1 G594A polymorphism is associated with migraine susceptibility in two independent case/control groups. Neurogenetics 5:129–133
Oterino A, Pascual J, Ruiz de Alegria C et al (2006) Association of migraine and ESR1 G325C polymorphism. Neuroreport 17:61–64
Oterino A, Toriello M, Cayón A et al (2008) Multilocus analyses reveal involvement of the ESR1, ESR2, and FSHR genes in migraine. Headache 48:1438–1450
Joshi G, Pradhan S, Mittal B (2010) Role of the oestrogen receptor (ESR1 PvuII and ESR1 325 C- > G) and progesterone receptor (PROGINS) polymorphisms in genetic susceptibility to migraine in a North Indian population. Cephalalgia 30:311–320
Ghosh J, Joshi G, Pradhan S, Mittal B (2012) Potential role of aromatase over estrogen receptor gene polymorphisms in migraine susceptibility: a case control study from North India. PLoS One 7:e34828
Colson NJ, Lea RA, Quinlan S et al (2005) Investigation of hormone receptor genes in migraine. Neurogenetics 6:17–23
Rodriguez-Acevedo AJ, Maher BH, Lea RA et al (2013) Association of oestrogen-receptor gene (ESR1) polymorphisms with migraine in the large Norfolk Island pedigree. Cephalalgia 33:1139–1147
Levy D (2012) Endogenous mechanisms underlying the activation and sensitization of meningeal nociceptors: the role of immuno-vascular interactions and cortical spreading depression. Curr Pain Headache Rep 16:270–277
Thompson MD, Noble-Topham S, Percy ME et al (2012) Chromosome 1p36 in migraine with aura: association study of the 5HT(1D) locus. Neuroreport 23:45–48
Curtain RP, Lea RA, Tajouri L et al (2005) Analysis of chromosome 1 microsatellite markers and the FHM2-ATP1A2 gene mutations in migraine pedigrees. Neurol Res 27:647–652
Nyholt DR, Morley KI, Ferreira MA et al (2005) Genome wide significant linkage to migrainous headache on chromosome 5q21. Am J Hum Genet 77:500–512
Gardner K, Barmada MM, Ptacek LJ, Hoffman EP (1997) A new locus for hemiplegic migraine maps to chromosome 1q31. Neurology 49:1231–1238
Lea RA, Shepherd AG, Curtain RP et al (2002) A typical migraine susceptibility region localizes to chromosome 1q31. Neurogenetics 4:17–22
Ligthart L, Nyholt DR, Hottenga JJ et al (2008) A genome-wide linkage scan provides evidence for both new and previously reported loci influencing common migraine. Am J Med Genet B Neuropsychiatr Genet 147B:1186–1195
Lea RA, Nyholt DR, Curtain RP et al (2005) A genome-wide scan provides evidence for loci influencing a severe heritable form of common migraine. Neurogenetics 6:67–72
Björnsson A, Gudmundsson G, Gudfinnsson E et al (2003) Localization of a gene for migraine without aura to chromosome 4q21. Am J Hum Genet 73:986–993
Wessman M, Kallela M, Kaunisto MA et al (2002) A susceptibility locus for migraine with aura, on chromosome 4q24. Am J Hum Genet 70:652–662
Anttila V, Kallela M, Oswell G et al (2006) Trait components provide tools to dissect the genetic susceptibility of migraine. Am J Hum Genet 79:85–99
Carlsson A, Forsgren L, Nylander PO et al (2002) Identification of a susceptibility locus for migraine with and without aura on 6p12.2-p21.1. Neurology 59:1804–1807
Oterino A, Toriello M, Castillo J et al (2012) Family-based association study of chromosome 6p12.2-p21.1 migraine locus. Headache 52:393–399
Tikka-Kleemola P, Artto V, Vepsäläinen S et al (2010) A visual migraine aura locus maps to 9q21-q22. Neurology 74:1171–1177
Anttila V, Nyholt DR, Kallela M et al (2008) Consistently replicating locus linked to migraine on 10q22-q23. Am J Hum Genet 82:1051–1063
Del Zompo M, Cherchi A, Palmas MA et al (1998) Association between dopamine receptor genes and migraine without aura in a Sardinian sample. Neurology 51:781–786
Cader ZM, Noble-Topham S, Dyment DA et al (2003) Significant linkage to migraine with aura on chromosome 11q24. Hum Mol Genet 12:2511–2517
Nyholt DR, Curtain RP, Gaffney PT et al (1996) Migraine association and linkage analyses of the human 5-hydroxytryptamine (5HT2A) receptor gene. Cephalalgia 16:463–467
Soragna D, Vettori A, Carraro G et al (2003) A locus for migraine without aura maps on chromosome 14q21.2-q22.3. Am J Hum Genet 72:161–167
Russo L, Mariotti P, Sangiorgi E et al (2005) A new susceptibility locus for migraine with aura in the 15q11-q13 genomic region containing three GABA-A receptor genes. Am J Hum Genet 76:327–333
May A, Ophoff RA, Terwindt GM et al (1995) Familial hemiplegic migraine locus on 19p13 is involved in the common forms of migraine with and without aura. Hum Genet 96:604–608
Nyholt DR, Lea RA, Goadsby PJ et al (1998) Familial typical migraine: linkage to chromosome 19p13 and evidence for genetic heterogeneity. Neurology 50:1428–1432
Nyholt DR, Dawkins JL, Brimage PJ et al (1998) Evidence for an X-linked genetic component in familial typical migraine. Hum Mol Genet 7:459–463
Nyholt DR, Curtain RP, Griffiths LR (2000) Familial typical migraine: significant linkage and localization of a gene to Xq24-28. Hum Genet 107:18–23
Ducros A, Joutel A, Vahedi K et al (1997) Mapping of a second locus for familial hemiplegic migraine to 1q21-q23 and evidence of further heterogeneity. Ann Neurol 42:885–890
Cevoli S, Pierangeli G, Monari L et al (2002) Familial hemiplegic migraine: clinical features and probable linkage to chromosome 1 in an Italian family. Neurol Sci 23:7–10
Marconi R, De Fusco M, Aridon P et al (2003) Familial hemiplegic migraine type 2 is linked to 0.9 Mb region on chromosome 1q23. Ann Neurol 53:376–381
Fernandez DM, Hand CK, Sweeney BJ, Parfrey NA (2008) A novel ATP1A2 gene mutation in an Irish familial hemiplegic migraine kindred. Headache 48:101–108
Dichgans M, Freilinger T, Eckstein G et al (2005) Mutation in the neuronal voltage-gated sodium channel SCN1A in familial hemiplegic migraine. Lancet 366:371–377
Cuenca-León E, Corominas R, Montfort M et al (2009) Familial hemiplegic migraine: linkage to chromosome 14q32 in a Spanish kindred. Neurogenetics 10:191–198
Joutel A, Bousser MG, Biousse V et al (1994) Familial hemiplegic migraine. Localization of a responsible gene on chromosome 19. Rev Neurol (Paris) 150:340–345
Ahmed MA, Reid E, Cooke A et al (1996) Familial hemiplegic migraine in the west of Scotland: a clinical and genetic study of seven families. J Neurol Neurosurg Psychiatry 61:616–620
Lafrenière RG, Cader MZ, Poulin JF et al (2010) A dominant-negative mutation in the TRESK potassium channel is linked to familial migraine with aura. Nat Med 43:1157–1160
Lafrenière RG, Rouleau GA (2011) Role of the TRESK two-pore potassium channel. Int J Biochem Cell Biol 43:1533–1536
Andres-Enguix I, Shang L, Stansfeld PJ et al (2012) Functional analysis of missense variants in the TRESK (KCNK18) K channel. Sci Rep 2:237
Anttila V, Stefansson H, Kallela M, International Headache Genetics Consortium et al (2010) Genome-wide association study of migraine implicates a common susceptibility variant on 8q22.1. Nat Genet 42:869–873
Kang DC, Su ZZ, Sarkar D et al (2005) Cloning and characterization of HIV-1-inducible astrocyte elevated gene-1, AEG-1. Gene 353:8–15
Gasparini CF, Griffiths LR (2013) The biology of the glutamatergic system and potential role in migraine. Int J Biomed Sci 9:1–8
Chasman DI, Schürks M, Anttila V et al (2011) Genome-wide association study reveals three susceptibility loci for common migraine in the general population. Nat Genet 43:695–698
Proudfoot CJ, Garry EM, Cottrell DF et al (2006) Analgesia mediated by the TRPM8 cold receptor in chronic neuropathic pain. Curr Biol 16:1591–1605
Biondi DM (2006) Is migraine a neuropathic pain syndrome? Curr Pain Headache Rep 10:167–178
Lillis AP, Van Duyn LB, Murphy-Ullrich JE, Strickland DK (2008) LDL receptor-related protein 1: unique tissue-specific functions revealed by selective gene knockout studies. Physiol Rev 88:887–918
Arndt AK, Schafer S, Drenckhahn JD et al (2013) Fine mapping of the 1p36 deletion syndrome identifies mutation of PRDM16 as a cause of cardiomyopathy. Am J Hum Genet 93:67–77
Bjork BC, Turbe-Doan A, Prysak M et al (2010) Prdm16 is required for normal palatogenesis in mice. Hum Mol Genet 19:774–789
Fan X, Wang J, Fan W et al (2014) Replication of migraine GWAS susceptibility loci in Chinese Han population. Headache 54:709–715
Esserlind AL, Christensen AF, Le H et al (2013) Replication and meta-analysis of common variants identifies a genome-wide significant locus in migraine. Eur J Neurol 20:765–772
Ligthart L, de Vries B, Smith AV et al (2011) Meta-analysis of genome-wide association for migraine in six population-based European cohorts. Eur J Hum Genet 19:901–907
Freilinger T, Anttila V, de Vries B, International Headache Genetics Consortium et al (2012) Genome-wide association analysis identifies susceptibility loci for migraine without aura. Nat Genet 44:777–782
Shalizi A, Gaudillière B, Yuan Z et al (2006) A calcium-regulated MEF2 sumoylation switch controls postsynaptic differentiation. Science 311:1012–1017
Flavell SW, Cowan CW, Kim TK et al (2006) Activity-dependent regulation of MEF2 transcription factors suppresses excitatory synapse number. Science 311:1008–1012
Ferrari MD, Odink J, Bos KD et al (1990) Neuroexcitatory plasma amino acids are elevated in migraine. Neurology 40:1582–1586
Lin HY, Wang XF, Ng-Eaton E et al (1992) Expression cloning of the TGF-beta type II receptor, a functional transmembrane serine/threonine kinase. Cell 68:775–785
Law C, Bunyan D, Castle B et al (2006) Clinical features in a family with an R460H mutation in transforming growth factor beta receptor 2 gene. J Med Genet 43:908–916
Cox HC, Lea RA, Bellis C et al (2012) A genome-wide analysis of 'Bounty’ descendants implicates several novel variants in migraine susceptibility. Neurogenetics 13:261–266
Anttila V, Winsvold BS, Gormley P, et al.; North American Brain Expression Consortium; UK Brain Expression Consortium; International Headache Genetics Consortium (2013) Genome-wide meta-analysis identifies new susceptibility loci for migraine. Nat Genet 45:912–917
Russell MB, Olesen J (1995) Increased familial risk and evidence of genetic factor in migraine. BMJ 311:541–544
Persico AM, Napolioni V (2013) Autism genetics. Behav Brain Res 251:95–112
Rudkjobing LA, Esserlind A-L, Olesen J (2012) Future possibilities in migraine genetics. J Headache Pain 13:505–511
Gottesman II, Gould TD (2003) The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry 160:636–645
Ruggeri B, Sarkans U, Schumann G, Persico AM (2014) Biomarkers in autism spectrum disorder: the old and the new. Psychopharmacology (Berl) 231:1201–1216
Durham P, Papapetropoulos S (2013) Biomarkers associated with migraine and their potential role in migraine management. Headache 53:1262–1277
Ligthart L, Hottenga JJ, Lewis CM et al (2014) Genetic risk score analysis indicates migraine with and without comorbid depression are genetically different disorders. Hum Genet 133:173–186
De Felice M, Ossipov MH, Wang R et al (2010) Triptan-induced enhancement of neuronal nitric oxide synthase in trigeminal ganglion dural afferents underlies increased responsiveness to potential migraine triggers. Brain 133:2475–2488
Acknowledgments
The authors are grateful to Drs. Maria Dora Morgante, Anna Crapulli, and to the personnel of the library at UCBM for their assistance in collecting the literature reviewed in the present article.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Other research by the authors is supported through the Italian Ministry for University, Scientific Research and Technology (PRIN n.2006058195 and n.2008BACT54_002), the Italian Ministry of Health (RFPS-2007-5-640174 and RF-2011-02350537), the Fondazione Gaetano e Mafalda Luce (Milan, Italy), Autism Speaks (Princeton, NJ), the Autism Research Institute (San Diego, CA), and the Innovative Medicines Initiative Joint Undertaking (EU-AIMS, n. 115300).
Conflict of interest
The authors declare that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Persico, A.M., Verdecchia, M., Pinzone, V. et al. Migraine genetics: current findings and future lines of research. Neurogenetics 16, 77–95 (2015). https://doi.org/10.1007/s10048-014-0433-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10048-014-0433-x