Abstract
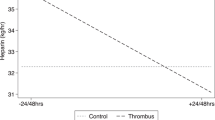
Critically ill pediatric patients supported on ventricular assist devices (VADs) are increasingly being anticoagulated on bivalirudin, but with difficulty monitoring anticoagulation. Activated partial thromboplastin time (aPTT) has recently been shown to poorly correlate with bivalirudin plasma concentrations, while dTT had excellent correlation. However, aPTT is the more common monitoring test and dTT testing is rarely used. In addition, effects of frequent clinical VAD scenarios (such as inflammation) on the accuracy of aPTT and dTT testing remains uncertain. We reviewed the effects of clinical scenarios (infection/inflammation, chylothorax, and steroids administration) on anticoagulation monitoring in 10 pediatric VAD patients less than 3 years at Cincinnati Children's Hospital Medical Center from 10/27/2020 to 5/6/2022 using bivalirudin for anticoagulation. There were 16 inflammation/infection, 3 chylothorax, and 6 steroids events. Correlation between dTT and aPTT was significantly lower after infection/inflammation, with dTT increasing prior to inflammation/infection while aPTT remained unchanged. In addition, steroids are administered to VAD patients to reduce inflammation and thus additionally stabilize anticoagulation. However, this anticoagulation stabilization effect was reflected more accurately by dTT compared to aPTT. In children requiring VAD support utilizing bivalirudin anticoagulation, inflammation/infection is a common occurrence resulting in anticoagulation changes that may be more accurately reflected by dTT as opposed to aPTT.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- VAD:
-
Ventricular assist device
- aPTT:
-
Activated partial thromboplastin time
- DTT:
-
Dilute thrombin time
References
Schweiger M, Hubler M, Albisetti M. Heparin anticoagulation monitoring in patients supported by ventricular assist devices. ASAIO J. 2015;61:487–8.
Huang JY, Monagle P, Massicotte MP, VanderPluym CJ. Antithrombotic therapies in children on durable ventricular assist devices: a literature review. Thromb Res. 2018;172:194–203.
Sylvia LM, Ordway L, Pham DT, DeNofrio D, Kiernan M. Bivalirudin for treatment of LVAD thrombosis: a case series. ASAIO J. 2014;60:744–7.
Burstein D, Kimmel S, Putt M, Rossano J, VanderPluym C. Cost-effectiveness of bivalirudin in pediatric ventricular assist devices. J Heart Lung Transplant. 2022. https://doi.org/10.1016/j.healun.2022.10.006.
Rimsans J, Sylvester KW, Connors JM. Direct thrombin inhibitor for LVAD thrombosis: a closer look. Clin Appl Thromb Hemost. 2017;23:405–9.
Ryerson LM, Balutis KR, Granoski DA, Nelson LR, Massicotte MP, Lequier LL, et al. Prospective exploratory experience with bivalirudin anticoagulation in pediatric extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2020;21:975–85.
Wong TE, Huang YS, Weiser J, Brogan TV, Shah SS. Antithrombin concentrate use in children: a multicenter cohort study. J Pediatr. 2013;163:1329-1334.e1.
Bates A, Buchholz H, Freed D, MacArthur R, Pi DT, Conway J. Bivalirudin experience in a heterogeneous ventricular assist device population. ASAIO J. 2020;66:677–82.
VanderPluym CJ, Cantor RS, Machado D, Boyle G, May L, Griffiths E, et al. Utilization and outcomes of children treated with direct thrombin inhibitors on paracorporeal ventricular assist device support. ASAIO J. 2020;66:939–45.
Puri K, Tunuguntla HP, Hensch LA, Loh J, Hui SK, Razavi A, et al. Bivalirudin or unfractionated heparin for anticoagulation in pediatric patients on continuous flow ventricular assist device support: single-center retrospective cohort study. Pediatr Crit Care Med. 2022;23:e465–75.
Zaleski KL, DiNardo JA, Nasr VG. Bivalirudin for pediatric procedural anticoagulation: a narrative review. Anesth Analg. 2019;128:43–55.
Teruya J, Hensch L, Bruzdoski K, Adachi I, Hui SR. Monitoring bivalirudin therapy in children on extracorporeal circulatory support devices: thromboelastometry versus routine coagulation testing. Thromb Res. 2020;186:54–7.
Molinaro RJ, Szlam F, Levy JH, Fantz CR, Tanaka KA. Low plasma fibrinogen levels with the clauss method during anticoagulation with bivalirudin. Anesthesiology. 2008;109:160–1.
Rabinowitz EJ, Ouyang A, Armstrong DR, Wallendorf M. Poor reliability of common measures of anticoagulation in pediatric extracorporeal membrane oxygenation. ASAIO J. 2021;68:850–8.
Engel ELM, Martin J, Palumbo J, Lorts A, Geer R, Luchtman-Jones L. Use of bivalirudin-specific monitoring assays in ventricular assist device patients. Blood. 2021;138:3236.
Teruya J, Bruzdoski K, Hensch L, Hui SR, Kostousov V. How to best monitor bivalirudin anticoagulant effect for ECMO and VAD-comparison of four assay methods. Int J Lab Hematol. 2022;44:589–94.
Adatya S, Uriel N, Yarmohammadi H, Holley CT, Feng A, Roy SS, et al. Anti-factor Xa and activated partial thromboplastin time measurements for heparin monitoring in mechanical circulatory support. JACC Heart Fail. 2015;3:314–22.
van Zaane B, Nur E, Squizzato A, Gerdes VE, Buller HR, Dekkers OM, et al. Systematic review on the effect of glucocorticoid use on procoagulant, anti-coagulant and fibrinolytic factors. J Thromb Haemost. 2010;8:2483–93.
Perry T, Bora K, Bakar A, Meyer DB, Sweberg T. Non-surgical risk factors for the development of chylothorax in children after cardiac surgery—does fluid matter? Pediatr Cardiol. 2020;41:194–200.
Buckley JR, Graham EM, Gaies M, Alten JA, Cooper DS. Clinical epidemiology and centre variation in chylothorax rates after cardiac surgery in children a report from the pediatric cardiac critical care consortium. Cardiol Young. 2017. https://doi.org/10.1017/S104795111700097X.
Bernet-Buettiker V, Waldvogel K, Cannizzaro V, Albisetti M. Antithrombin activity in children with chylothorax. Eur J Cardiothorac Surg. 2006;29:406–9.
Zuluaga MT. Chylothorax after surgery for congenital heart disease. Curr Opin Pediatr. 2012;24:291–4.
Acknowledgements
This work was conducted with support from the Heart Institute Research Core (HIRC) at Cincinnati Children’s Hospital.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by KB, AL, ZG, and TP. The first draft of the manuscript was written by KB and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
Angela Lorts is a consultant for Abbott, SynCardia, Medtronic, Abiomed and Berlin Heart Inc.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brandewie, K., Lorts, A., Luchtman-Jones, L. et al. Impact of inflammation and steroids on anti-coagulation in children supported on a ventricular assist device. J Artif Organs (2024). https://doi.org/10.1007/s10047-024-01442-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10047-024-01442-2