Abstract
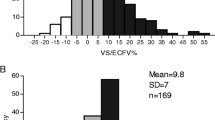
The distribution volume of uric acid is affected by the amount of extracellular water (ECW), while urea distribution volume can be considered as total body water (TBW). Thus, the ratio of distribution volumes of uric acid and urea can be paralleled to and be considered as the proxy of ECW/TBW. A total of 108 patients at our facility was included. The uric acid and urea distribution volume ratio (UUVdR) calculated from the single-pool model, which was measured within 1 month of the time when the bioimpedance index was measured. ECW/TBW at the end of the HD session was measured by InBody S10. We investigated the association between the UUVdR and the ECW/TBW values and the factors affecting the residuals of the regression equation. We also evaluated the predictive ability of overhydration or dehydration in randomly selected two groups, i.e., the training group and the validation group. ECW/TBW correlated highly with UUVdR. Multivariate analysis demonstrated that only creatinine and ECW/TBW were significantly associated with regression residuals. The cutoff values of UUVdR for overhydration and dehydration were 0.666 and 0.579, respectively, in the training group. Their AUC were 0.872 and 0.898, respectively. The sensitivity and specificity values in the validation group were 0.571 and 0.868 for overhydration, and 0.444 and 0.953 for dehydration, respectively. UUVdR might be a proxy of hydration status in hemodialysis patients. It may be possible to predict hydration status without dedicated devices in the epidemiological study.






Similar content being viewed by others
Data availability
The data that support the findings of this study are not publicly available due to the decision by the ethics committee of our facility.
References
Foley RN, Herzog CA, Collins AJ. Blood pressure and long-term mortality in United States hemodialysis patients: USRDS Waves 3 and 4 Study. Kidney Int. 2002;62:1784–90.
Hirakata H, Nitta K, Inaba M, Shoji T, Fujii H, Kobayashi S, et al. Japanese Society for Dialysis Therapy guidelines for management of cardiovascular diseases in patients on chronic hemodialysis. Ther Apher Dial. 2012;16:387–435.
Kotanko P, Levin NW, Zhu F. Current state of bioimpedance technologies in dialysis. Nephrol Dial Transplant. 2008;23:808–12.
Di Iorio BR, Scalfi L, Terracciano V, Bellizzi V. A systematic evaluation of bioelectrical impedance measurement after hemodialysis session. Kidney Int. 2004;65:2435–40.
Descombes E, Perriard F, Fellay G. Diffusion kinetics of urea, creatinine and uric acid in blood during hemodialysis. Clinical implications. Clin Nephrol. 1993;40:286–95.
Daugirdas JT, Depner TA. Creatinine generation from kinetic modeling with or without postdialysis serum creatinine measurement: results from the HEMO study. Nephrol Dial Transplant. 2017;32:1926–33.
Raimann JG, Zhu F, Wang J, Thijssen S, Kuhlmann MK, Kotanko P, et al. Comparison of fluid volume estimates in chronic hemodialysis patients by bioimpedance, direct isotopic, and dilution methods. Kidney Int. 2014;85:898–908.
Shinzato T, Nakai S, Ito T, Shibata K, Matsuoka T, Kato S, et al. Uric acid distribution volume calculated by kinetic modeling and extracellular volume predicted by bioimpedance method. Int J Artif Organs. 2020. https://doi.org/10.1177/0391398820909835.
Langsdorf LJ, Zydney AL. Effect of uremia on the membrane transport characteristics of red blood cells. Blood. 1993;81:820–7.
Nongnuch A, Campbell N, Stern E, El-Kateb S, Fuentes L, Davenport A. Increased postdialysis systolic blood pressure is associated with extracellular overhydration in hemodialysis outpatients. Kidney Int. 2015;87:452–7.
Acknowledgements
We thank nurses and clinical engineers in charge of patients for their delivering dialysis treatments.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
YK, and NH contributed to the research idea and study design; YK, and NH contributed to data acquisition, analysis, or interpretation; YK, and NH performed statistical analysis and wrote the paper; and KT contributed to supervision or mentorship. YK, NH, SS, MM, NT, KI, and KT have critically reviewed the manuscript and approved the final version.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Statement of ethics
The study protocol was reviewed and approved by the Ethics Committee of Tokyo Women’s Medical University, approval number 4822-2R. Written informed consents were waived due to the nature of this study and patients who did not want to participate in this study expressed their options by opting-out from the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kawaguchi, Y., Hanafusa, N., Sakurai, S. et al. The uric acid–urea distribution volume ratio is a potential marker of hydration status in patients on hemodialysis. J Artif Organs 26, 316–325 (2023). https://doi.org/10.1007/s10047-022-01377-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-022-01377-6