Abstract
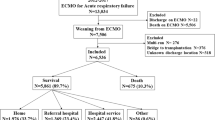
Veno-venous extracorporeal membrane oxygenation (VV-ECMO) is a reliable and effective extracorporeal life support during lung transplantation (LTx). However, the clinical benefit of delayed VV-ECMO weaning remains unclear. The current study aims to investigate whether delayed weaning of VV-ECMO is more beneficial to the rehabilitation for lung transplant patients. Patients who underwent LTx with VV-ECMO between January 2017 and January 2019 were included. Enrollment of patients was suitable for weaning off ECMO immediately after surgery. Randomization was performed in the operating room. Postoperative outcomes were compared between the two groups. Besides, univariate and multivariable logistic regressions were performed to estimate risk of postoperative complications. Compared to VV-ECMO weaning immediately after LTx, delayed weaning was associated with shorter hospital length of stay (days, 31 vs. 46; P < 0.05), lower incidence of noninvasive ventilation (4.3% vs. 24.4%; P < 0.05), primary graft dysfunction (PGD) (6.4% vs. 29.3%; P < 0.05), atrial fibrillation (AF) (4.3% vs. 22%, P < 0.05), and respiratory failure (4.3% vs. 19.5%; P < 0.05). Multivariable logistic regressions revealed that VV-ECMO weaning after LTx was independently correlated with increased risk of developing PGD [odds ratio (OR), 5.97, 95% CI 1.16–30.74], AF (OR, 6.87, 95% CI 1.66–28.47) and respiratory failure (OR, 6.02, 95% CI 1.12–32.49) by comparison of delayed VV-ECMO weaning. Patients with delayed VV-ECMO weaning are associated with lower complications and short hospital length of stay, while it relates to longer mechanical ventilation. These findings suggest that delayed VV-ECMO after LTx can facilitate rehabilitation.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author (qcwucq@163.com). The data are not publicly available due to privacy or ethical restrictions.
References
Hartert M, Senbaklavacin O, Gohrbandt B, Fischer BM, Buhl R, Vahld CF. Lung transplantation: a treatment option in end-stage lung disease. Dtsch Arztebl Int. 2014;111:107–16.
Meyer KC. Recent advances in lung transplantation. F1000Res. 2018. https://doi.org/10.12688/f1000research.15393.1.
Ius F, Tudorache I, Warnecke G. Extracorporeal support, during and after lung transplantation: the history of an idea. J Thorac Dis. 2018;10:5131–48.
Machuca TN, Collaud S, Mercier O, Cheung M, Cunningham V, Kim SJ, et al. Outcomes of intraoperative extracorporeal membrane oxygenation versus cardiopulmonary bypass for lung transplantation. J Thorac Cardiovasc Surg. 2015;149:1152–7.
Biscotti M, Yang J, Sonett J, Bacchetta M. Comparison of extracorporeal membrane oxygenation versus cardiopulmonary bypass for lung transplantation. J Thorac Cardiovasc Surg. 2014;148:2410–5.
Ius F, Kuehn C, Tudorache I, Sommer W, Avsar M, Boethig D, et al. Lung transplantation on cardiopulmonary support: venoarterial extracorporeal membrane oxygenation outperformed cardiopulmonary bypass. J Thorac Cardiovasc Surg. 2012;144:1510–6.
Tonna JE, Abrams D, Brodie D, Greenwood JC, Rubio Mateo-Sidron JA, Usman A, et al. Management of adult patients supported with venovenous extracorporeal membrane oxygenation (VV ECMO): guideline from the extracorporeal life support organization (ELSO). ASAIO J. 2021;67:601–10.
Hashimoto K, Hoetzenecker K, Yeung JC, Jeagal L, Donahoe L, Pierre A, et al. Intraoperative extracorporeal support during lung transplantation in patients bridged with venovenous extracorporeal membrane oxygenation. J Heart Lung Transplant. 2018;37:1418–24.
Fang A, Studer S, Kawut SM, Ahya VN, Lee J, Wille K, et al. Elevated pulmonary artery pressure is a risk factor for primary graft dysfunction following lung transplantation for idiopathic pulmonary fibrosis. Chest. 2011;139:782–7.
Moser B, Jaksch P, Taghavi S, Muraközy G, Lang G, Hager H, et al. Lung transplantation for idiopathic pulmonary arterial hypertension on intraoperative and postoperatively prolonged extracorporeal membrane oxygenation provides optimally controlled reperfusion and excellent outcome. Eur J Cardiothorac Surg. 2018;53:178–85.
Hu CX, Chen WH, He JX, Jiang GN, Li XS, Wei D, et al. Lung transplantation in China between 2015 and 2018. Chin Med J (Engl). 2019;132:2783–9.
Banga A, Mohanka M, Mullins J, Bollineni S, Kaza V, Huffman L, et al. Incidence and variables associated with 30-day mortality after lung transplantation. Clin Transplant. 2019;33: e13468.
Shah RJ, Diamond JM. Primary graft dysfunction (PGD) following lung transplantation. Semin Respir Crit Care Med. 2018;39:148–54.
Kao CC, Parulekar AD. Postoperative management of lung transplant recipients. J Thorac Dis. 2019;11:S1782–8.
Faccioli E, Terzi S, Pangoni A, Lomangino I, Rossi S, Lloret A, et al. Extracorporeal membrane oxygenation in lung transplantation: indications, techniques and results. World J Transplant. 2021;11:290–302.
Bateman RM, Sharpe MD, Jagger JE, Ellis CG, Solé-Violán J, López-Rodríguez M, et al. 36th international symposium on intensive care and emergency medicine : Brussels, Belgium. 15–18 March 2016. Crit Care. 2016;20:94.
Hoetzenecker K, Benazzo A, Stork T, Sinn K, Schwarz S, Schweiger T, et al. Bilateral lung transplantation on intraoperative extracorporeal membrane oxygenator: an observational study. J Thorac Cardiovasc Surg. 2020;160:320-327.e1.
Hoetzenecker K, Schwarz S, Muckenhuber M, Benazzo A, Frommlet F, Schweiger T, et al. Intraoperative extracorporeal membrane oxygenation and the possibility of postoperative prolongation improve survival in bilateral lung transplantation. J Thorac Cardiovasc Surg. 2018;155:2193-2206.e3.
Fuehner T, Kuehn C, Welte T, Gottlieb J. ICU care before and after lung transplantation. Chest. 2016;150:442–50.
Harano T, Ryan JP, Morrell MR, Luketich JD, Sanchez PG. Extracorporeal membrane oxygenation for primary graft dysfunction after lung transplantation. ASAIO J. 2021. https://doi.org/10.1097/MAT.0000000000001350.
Saad M, Elgendy IY, Mentias A, Abdelaziz HK, Barakat AF, Abuzaid A, et al. Incidence, predictors, and outcomes of early atrial arrhythmias after lung transplant: a systematic review and meta-analysis. JACC Clin Electrophysiol. 2017;3:718–26.
Orrego CM, Cordero-Reyes AM, Estep JD, Seethamraju H, Scheinin S, Loebe M, et al. Atrial arrhythmias after lung transplant: underlying mechanisms, risk factors, and prognosis. J Heart Lung Transplant. 2014;33:734–40.
Jesel L, Barraud J, Lim HS, Marzak H, Messas N, Hirschi S, et al. Early and late atrial arrhythmias after lung transplantation- incidence, predictive factors and impact on mortality. Circ J. 2017;81:660–7.
Roukoz H, Benditt DG. Atrial arrhythmias after lung transplantation. Trends Cardiovasc Med. 2018;28:53–61.
Raghavan D, Gao A, Ahn C, Torres F, Mohanka M, Bollineni S, et al. Contemporary analysis of incidence of post-operative atrial fibrillation, its predictors, and association with clinical outcomes in lung transplantation. J Heart Lung Transplant. 2015;34:563–70.
Barnes H, Gurry G, McGiffin D, Westall G, Levin K, Paraskeva M, et al. Atrial flutter and fibrillation following lung transplantation: incidence, associations and a suggested therapeutic algorithm. Heart Lung Circ. 2020;29:1484–92.
Author information
Authors and Affiliations
Contributions
Conception and design: L-JL and H-YX. Administrative support: Q-CW and J-YC. Provision of study materials or patients: KJ, H-YX. Collection and assembly of data: L-JL, CZ and H-YX. Data analysis and interpretation: L-JL, X-WW, MD and H-YX. Manuscript writing: All authors. Final approval of manuscript: All authors.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, LJ., Xu, HY., Wang, XW. et al. Impact of delayed veno-venous extracorporeal membrane oxygenation weaning on postoperative rehabilitation of lung transplantation: a single-center comparative study. J Artif Organs 26, 303–308 (2023). https://doi.org/10.1007/s10047-022-01376-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-022-01376-7