Abstract
Microparticles are produced by various cells due to a number of different stimuli in the circulatory system. Shear stress has been shown to injure red blood cells resulting in hemolysis or non-reversible sub-hemolytic damage. We hypothesized that, in the sub-hemolytic shear range, there exist sufficient mechanical stimuli for red blood cells to respond with production of microparticles. Red blood cells isolated from blood of healthy volunteers were exposed to high shear stress in a microfluidic channel to mimic mechanical trauma similar to that occurring in ventricular assist devices. Utilizing flow cytometry techniques, both an increase of shear rate and exposure time showed higher concentrations of red blood cell microparticles. Controlled shear rate exposure shows that red blood cell microparticle concentration may be indicative of sub-hemolytic damage to red blood cells. In addition, properties of these red blood cell microparticles produced by shear suggest that mechanical trauma may underlie some complications for cardiovascular patients.







Similar content being viewed by others
References
Mecozzi G, et al. Intravascular hemolysis in patients with new-generation prosthetic heart valves: a prospective study. J Thorac Cardiovasc Surg. 2002;123:550–6.
Mitlyng BL, et al. Use of breath carbon monoxide to measure the influence of prosthetic heart valves on erythrocyte survival. Am J Cardiol. 2006;97:1374–6.
Taimeh Z, et al. Erythrocyte aging as a mechanism of anemia and a biomarker of device thrombosis in continuous-flow left ventricular assist devices. J Heart Lung Transplant. 2017;36:625–32.
Olia SE, et al. Mechanical blood trauma in assisted circulation: sublethal RBC damage preceding hemolysis. Int J Artif Organs. 2016;39:150–9.
Barcellini W, Fattizzo B. Clinical applications of hemolytic markers in the differential diagnosis and management of hemolytic anemia. Dis Markers. 2015;2015:635670.
Dao KM, et al. Sensitivity of the erythrocyte membrane bilayer to subhemolytic mechanical trauma as detected by fluorescence anisotropy. Biorheology. 1994;31:69–76.
Kameneva MV, et al. Mechanisms of red blood cell trauma in assisted circulation. Rheologic similarities of red blood cell transformations due to natural aging and mechanical stress. Blood Trauma Assist Circ. 1995;41:457–60.
Kameneva MV, et al. Decrease in red blood cell deformability caused by hypothermia, hemodilution, and mechanical stress: factors related to cardiopulmonary bypass. ASAIO J. 1999;45:307–10.
Simmonds MJ, et al. Erythrocyte deformability responses to intermittent and continuous subhemolytic shear stress. Biorheology. 2014;51:171–85.
O’Rear EA, et al. Reduced erythrocyte deformability associated with calcium accumulation. Biochimica et Biophysica Acta. 1982;691:274–80.
Sutera SP. Flow-induced trauma to blood cells. Circul Res. 1977;41:2–8.
Shiga T, et al. Cell age-dependent changes in deformability and calcium accumulation of human erythrocytes. Biochimica et Biophysica Acta. 1985;814:289–99.
Sutera SP, et al. Age-related changes in deformability of human erythrocytes. Blood. 1985;65:275–82.
Buerck JP, et al. A flow induced autoimmune response and accelerated senescence of red blood cells in cardiovascular devices. Sci Rep. 2019;9:19443.
Sandza JG, et al. Subhemolytic trauma of erythrocytes: recognition and sequestration by the spleen as a function of shear. Trans Am Soc Artif Intern Organs. 1974;B20:457–62.
Alaarg A, et al. Red blood cell vesiculation in hereditary hemolytic anemia. Front Physiol. 2013;4:365.
Willekens FL, et al. Erythrocyte vesiculation: a self-protective mechanism? Br J Haematol. 2008;141:549–56.
Nascimbene A, et al. Association between cell-derived microparticles and adverse events in patients with nonpulsatile left ventricular assist devices. J Heart Lung Transplant. 2014;33:470–7.
Kay MMB, et al. Senescent cell antigen is immunologically related to band 3. Cell Biol. 1983;80:1631–5.
Low PS, et al. Contribution of the band 3-ankyrin interaction to erythrocyte membrane mechanical stability. Blood. 1991;77:1581–6.
Rubin O, et al. Red blood cell microparticles: clinical relevance. Transfus Med Hemother. 2012;39:342–7.
Burger P, et al. Potassium leakage primes stored erythrocytes for phosphatidylserine exposure and shedding of pro-coagulant vesicles. Br J Haematol. 2013;160:377–86.
Bevers EM, Comfurius P, Dekkers DW, Zwaal RF. Lipid translocation across the plasma membrane of mammalian cells. Biochimica et Biophysica Acta. 1999;1439:317–30.
Koshiar RL, et al. Erythrocyte-derived microparticles supporting activated protein C-mediated regulation of blood coagulation. PLoS ONE. 2014;9:e104200.
Greenwalt TJ, Byran DJ, Dumaswala UJ. Erythrocyte membrane vesiculation and changes in membrane composition during storage in citrate-phosphate-dextrose-adenine-1. Vox Sang. 1984;47:261–70.
Dumaswala UJ, T.J.G. Human erythrocytes shed exocytic vesicles in vivo. Transfusion. 1984;24:490–2.
Lutz HU, Liu S-C, Palek J. Release of spectrin-free vesicles from human erythrocytes during ATP depletion. J Cell Biol. 1977;73:548–60.
Badimon L, et al. Diet, microparticles and atherothrombosis. Front Biosci. 2018;23:432–57.
Suades R, et al. Growing thrombi release increased levels of CD235a(+) microparticles and decreased levels of activated platelet-derived microparticles. Validation in ST-elevation myocardial infarction patients. J Thromb Haemost. 2015;13:1776–86.
Chiva-Blanch G, et al. Microparticle shedding by erythrocytes, monocytes and vascular smooth muscular cells is reduced by aspirin in diabetic patients. Rev Esp Cardiol (Engl Ed). 2016;69:672–80.
Badimon L, et al. Microvesicles in atherosclerosis and angiogenesis: from bench to bedside and reverse. Front Cardiovasc Med. 2017;4:77.
Hugel BND, et al. Elevated levels of circulating procoagulant microparticles in patients with paroxysmal nocturnal hemoglobinuria and aplastic anemia. Hemostasis Thromb Vasc Biol. 1999;93:3451–6.
van Beers EJ, et al. Circulating erythrocyte-derived microparticles are associated with coagulation activation in sickle cell disease. Haematologica. 2009;94:1513–9.
Jeske WP, et al. Blood cell microparticles as biomarkers of hemostatic abnormalities in patients with implanted cardiac assist devices. Biomarkers Med. 2016;10:1095–104.
Burnier L, et al. Cell-derived microparticles in haemostasis and vascular medicine. Thromb Haemost. 2009;101:439–51.
Vion AC, et al. Shear stress regulates endothelial microparticle release. Circ Res. 2013;112:1323–33.
Westerman M, Porter JB. Red blood cell-derived Microparticles: an overview. Blood Cells Mol Dis. 2016;59:134–9.
O’Rear EA, et al. Increased intracellular calcium and decreased deformability of erythrocytes from prosthetic heart valve patients. Clin Hemorheol. 1984;4:461–71.
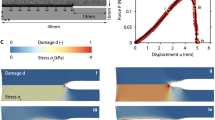
Alsmadi NZ, et al. Constricted microfluidic devices to study the effects of transient high shear exposure on platelets. Biomicrofluidics. 2017;11(6):064105.
Son Y. Determination of shear viscosity and shear rate from pressure drop and flow rate relationship in a rectangular channel. Polymer. 2007;48:632–7.
Lewis CS, et al. Effects of transient exposure to high shear on neutrophil rolling behavior. Cell Mol Bioeng. 2018;11:279–90.
Zhang T, et al. Study of flow-induced hemolysis using novel Couette-type blood-shearing devices. Artif Organs. 2011;35:1180–6.
Toninato R, Fadda G, Susin FM. A red blood cell model to estimate the hemolysis fingerprint of cardiovascular devices. Artif Organs. 2018;42:58–67.
Hochmuth RM, Evans EA, Colvard DF. Viscosity of human red cell membrane in plastic flow. Microvasc Res. 1976;11:155–9.
Distler JHW, et al. The release of microparticles by apoptotic cells and their effects on macrophages. Apoptosis. 2005;10:731–41.
Burger D, et al. Microparticles: biomarkers and beyond. Clin Sci (Lond). 2013;124:423–41.
Terrisse AD, et al. Internalization of microparticles by endothelial cells promotes platelet/endothelial cell interaction under flow. J Thromb Haemost. 2010;8:2810–9.
Willekens FL, et al. Liver Kupffer cells rapidly remove red blood cell-derived vesicles from the circulation by scavenger receptors. Blood. 2005;105:2141–5.
Litvack ML, Post M, Palaniyar N. IgM promotes the clearance of small particles and apoptotic microparticles by macrophages. PLoS ONE. 2011;6:e17223.
Shah P, et al. Lactate dehydrogenase is superior to serum free hemoglobin as a marker of pump thrombosis in left ventricular assist devices. J Heart Lung Transplant. 2013;32:S37.
Bartoli CR, et al. Clinical and in vitro evidence that subclinical hemolysis contributes to LVAD thrombosis. Ann Thorac Surg. 2018;105:807–14.
O’Rear EA, et al. Use of a rheological technique to evaluate erythrocyte membrane alterations. J Rheol. 1979;23:721–33.
Guo Q, et al. Microfluidic analysis of red blood cell deformability. J Biomech. 2014;47:1767–76.
Shiga T, Maeda N, Kon K. Erythrocyte Rheology. Crit Rev Oncol/Hematol. 1990;10:9–48.
Zubairova LD, et al. Circulating microparticles alter formation, structure, and properties of fibrin clots. Sci Rep. 2015;5:17611.
Waugh RE, et al. Rheologic properties of senescent erythrocytes: loss of surface area and volume with red blood cell age. Blood. 1992;79:1351–8.
Nomura S, Shimizu M. Clinical significance of procoagulant microparticles. J Intensive Care. 2015;3:2.
Berckmans R, Nieuwland R, Boing AN, Romijn FPHTM, Hack CE, Sturk A. Cell-derived microparticles circulate in healthy humans and support low grade thrombin generation. Thromb Haemost. 2001;85:639–46.
Ziad Mallat M et al (1999) Shed membrane microparticles with procoagulant potential in human atherosclerotic plaques: a role for apoptosis in plaque thrombogenicity. Circulation. 99:348–53.
Biró E, et al. Human cell-derived microparticles promote thrombus formation in vivo in a tissue factor-dependent manner. J Thromb Haemost. 2003;12:2561–8.
Sinauridze EI, et al. Platelet microparticle membranes have 50- to 100-fold higher specific procoagulant activity than activated platelets. Thromb Haemost. 2007;97:425–34.
Lipets E, et al. Circulating contact-pathway-activating microparticles together with factors IXa and XIa induce spontaneous clotting in plasma of hematology and cardiologic patients. PLoS ONE. 2014;9:e87692.
Van Der Meijden PE, et al. Platelet- and erythrocyte-derived microparticles trigger thrombin generation via factor XIIa. J Thromb Haemost. 2012;10:1355–62.
Jy W, et al. Red cell-derived microparticles (RMP) as haemostatic agent. Thromb Haemost. 2013;110:751–60.
Nauta AJ, et al. Direct binding of C1q to apoptotic cells and cells blebs induces complement activation. Eur J Immunol. 2002;32:1726–36.
Kay MMB. Mechanism of removal of-senescent cells by human macrophages in situ. Proc Nat Acad Sci. 1975;72:3521–5.
Kay M. Immunoregulation of cellular life span. Ann NY Acad Sci. 2005;1057:85–111.
Turrini F, et al. Clustering of integral membrane proteins of the human erythrocyte membrane stimulates autologous IgG binding, complement deposition, and phogocytosis. J Biol Chem. 1991;266:23611–7.
Lutz HU, Bogdanova A. Mechanisms tagging senescent red blood cells for clearance in healthy humans. Front Physiol. 2013;4:387.
Czerwinski M, et al. Degradation of the human erythrocyte membrane band 3 studied with the monoclonal antibody directed against an epitope on the cytoplasmic fragment of band 3. Eur J Biochem. 1988;174:647–54.
Grisendi G, et al. Detection of microparticles from human red blood cells by multiparametric flow cytometry. Blood Transfus. 2015;13:274–80.
Chandler WL. Measurement of microvesicle levels in human blood using flow cytometry. Cytometry B Clin Cytom. 2016;90:326–36.
Orozco AF, Lewis DE. Flow cytometric analysis of circulating microparticles in plasma. Cytometry A. 2010;77:502–14.
Acknowledgements
Research in this publication was supported by the National Institutes of Health Small Business Innovation Research program under Award Number R44HL114246 as a subcontract to the University of Oklahoma from VADovations and NIH Grant R21HL132286 to DWS and TAS. The content of the paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
JPB conducted experiments, analyzed data and wrote the paper; DKB ran experiments and analyzed data; EAO conceived of the project, contributed to analysis of results and writing to the paper; DWS aided in design and implementation of experiments and editing of the manuscript; TAS contributed to data analysis and review of the manuscript; DVP contributed to experimental analysis and manuscript revision.
Corresponding author
Ethics declarations
Conflict of interest
T.A.S. is currently employed with a company developing ventricular assist devices. All other authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Buerck, J.P., Burke, D.K., Schmidtke, D.W. et al. Production of erythrocyte microparticles in a sub-hemolytic environment. J Artif Organs 24, 135–145 (2021). https://doi.org/10.1007/s10047-020-01231-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-020-01231-7