Abstract
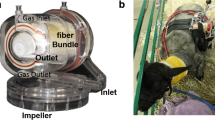
The lack of donor organs has led to the development of alternative “destination therapies”, such as a bio-artificial lung (BA) for end-stage lung disease. Ultimately aiming at a fully implantable BA, general capabilities and limitations of different oxygenators were tested based on the model of BA positioning at the right upper lobe. Three different-sized oxygenators (neonatal, paediatric, and adult) were tested in a mock circulation loop regarding oxygenation and decarboxylation capacities for three respiratory pathologies. Blood flows were imitated by a roller pump, and respiration was imitated by a mechanical ventilator with different FiO2 applications. Pressure drops across the oxygenators and the integrity of the gas-exchange hollow fibers were analyzed. The neonatal oxygenator proved to be insufficient regarding oxygenation and decarboxylation. Despite elevated pCO2 levels, the paediatric and adult oxygenators delivered comparable sufficient oxygen levels, but sufficient decarboxylation across the oxygenators was ensured only at flow rates of 0.5 L min. Only the adult oxygenator indicated no significant pressure drops. For all tested conditions, gas-exchange hollow fibers remained intact. This is the first study showing the general feasibility of delivering sufficient levels of gas exchange to an intracorporeal BA via patient’s breathing, without damaging gas-exchange hollow fiber membranes.






Similar content being viewed by others
References
Organization WHO. Global surveillance, prevention and control of chronic respiratory diseases: a comprehensive approach. Geneva: World Health Organization; 2013.
Koh Y. Update in acute respiratory distress syndrome. J Intensive Care. 2014;2:2.
Marasco SF, Lukas G, McDonald M, McMillan J, Ihle B. Review of ECMO (extra corporeal membrane oxygenation) support in critically ill adult patients. Heart Lung Circ. 2008;17:S41–47.
Yusen RD, Edwards LB, Kucheryavaya AY, et al. The registry of the International Society for Heart and Lung Transplantation: thirty-first adult lung and heart-lung transplant report—2014; focus theme: retransplantation. J Heart Lung Transplant. 2014;33:1009–24.
Kotloff RM, Thabut G. Lung transplantation. Am J Respir Crit Care Med. 2011;184:159–71.
Valapour M, Skeans MA, Heubner BM, et al. OPTN/SRTR 2012 annual data report: lung. Am J Transplant. 2014;14:139–65.
Warnecke G, Moradiellos J, Tudorache I, et al. Normothermic perfusion of donor lungs for preservation and assessment with the organ care system lung before bilateral transplantation: a pilot study of 12 patients. Lancet. 2012;380:1851–8.
Martin JT, Zwischenberger JB. Artificial lung and novel devices for respiratory support. Seminars in thoracic and cardiovascular surgery. Spring. 2013;25:70–5.
Ota K. Advances in artificial lungs. J Artif Organs. 2010;13:13–6.
Wiegmann B, Figueiredo C, Gras C, et al. Prevention of rejection of allogeneic endothelial cells in a biohybrid lung by silencing HLA-class I expression. Biomaterials. 2014;35:8123–33.
Hess C, Wiegmann B, Maurer AN, et al. Reduced thrombocyte adhesion to endothelialized poly 4-methyl-1-pentene gas exchange membranes-a first step toward bioartificial lung development. Tissue Eng Part A. 2010;16:3043–53.
Zwischenberger JB, Anderson CM, Cook KE, Lick SD, Mockros LF, Bartlett RH. Development of an implantable artificial lung: challenges and progress. ASAIO J. 2001;47:316 – 20.
Lick SD, Zwischenberger JB. Artificial lung: bench toward bedside. ASAIO J. 2004;50:2–5.
Nolan H, Wang D, Zwischenberger JB. Artificial lung basics: fundamental challenges, alternative designs and future innovations. Organogenesis. 2011;7:23–7. (Epub 2011 Jan 1).
Perlman CE, Mockros LF. Predicted oxygenation efficacy of a thoracic artificial lung. ASAIO J. 2012;58:247 – 54.
McGuigan AP, Sefton MV. The influence of biomaterials on endothelial cell thrombogenicity. Biomaterials. 2007;28:2547–71. (review).
Consigny PM. Endothelial cell seeding on prosthetic surfaces. J Long Term Eff Med Implants. 2000;10:79–95.
https://www.xenios-ag.com/medos-products/hilite-oxygenators/.
Borchardt R, Schlanstein P, Mager I, Arens J, Schmitz-Rode T, Steinseifer U. In vitro performance testing of a pediatric oxygenator with an integrated pulsatile pump. ASAIO J. 2012;58:420–5. doi:10.1097/MAT.0b013e318251dc70.
Stocks J, Quanjer PH. Reference values for residual volume, functional residual capacity and total lung capacity. ATS Workshop on Lung Volume Measurements. Official Statement of The European Respiratory Society. Eur Respir J. 1995;8:492–506. (review).
Wettstein RB, Shelledy DC, Peters JI. Delivered oxygen concentrations using low-flow and high-flow nasal cannulas. Respir Care. 2005;50:604–9.
Park M, Mendes PV, Hirota AS, Santos EV, Costa EL, Azevedo LC. Blood flow/pump rotation ratio as an artificial lung performance monitoring tool during extracorporeal respiratory support using centrifugal pumps. Rev Bras Ter Intensiva. 2015;27:178–84.
Mahajan AK, Doeing DC, Hogarth DK. Isolation of persistent air leaks and placement of intrabronchial valves. J Thorac Cardiovasc Surg. 2013;145:626–30. doi:10.1016/j.jtcvs.2012.12.003. (Epub 2013 Jan 9. Review).
Gogakos A, Barbetakis N, Lazaridis G, et al. Heimlich valve and pneumothorax. Ann Transl Med. 2015;3:54. doi:10.3978/j.issn.2305-5839.2015.03.25. (review).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Funding
This work was supported by a travelling award from the International Society of Heart and Lung Transplantation, by the Cluster of Excellence REBIRTH (Unit 4.1) and the German Center for Lung Research (DZL: 82DZL00201).
Rights and permissions
About this article
Cite this article
Schumer, E., Höffler, K., Kuehn, C. et al. In-vitro evaluation of limitations and possibilities for the future use of intracorporeal gas exchangers placed in the upper lobe position. J Artif Organs 21, 68–75 (2018). https://doi.org/10.1007/s10047-017-0987-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-017-0987-0