Abstract
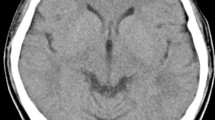
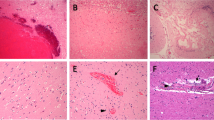
The clinical relevance of transcranial Doppler (TCD) detection of micro-embolic signals (MES) in patients with ventricular assist devices (VADs) has been described. However, all of the previous studies concerning TCD in patients with VADs were conducted in patients with old devices; the clinical relevance of TCD in patients with newer devices has not been fully elucidated. We recently encountered a patient with a continuous-flow VAD with hemolysis. TCD monitoring was useful for the direct evaluation of micro-emboli in this patient. A 50-year-old male who underwent HeartMate II® VAD (Thoratec Corporation; Pleasanton, CA) implantation with a diagnosis of ischemic cardiomyopathy 15 months prior was admitted to our institution because of findings suggestive of hemolysis, such as elevated lactate dehydrogenase (LDH) and total bilirubin. Unfractionated heparin was started after admission and hemolysis gradually improved. On admission, TCD detected 146 MES during 30 min of monitoring. During the hospital course, the MES count decreased to 20 signals on hospital day 4 and further decreased to 2 signals on hospital day 15 along with decreases in LDH and total bilirubin. Since hemolysis in VAD patients is thought to be associated with thromboembolic outcomes, MES detected by TCD indicate subclinical micro-emboli. TCD monitoring may be useful for assessing the risk of thromboembolic events in newer continuous-flow VAD patients through direct visualization of micro-emboli.


Similar content being viewed by others
References
Pagani FD, Miller LW, Russell SD, Aaronson KD, John R, Boyle AJ, Conte JV, Bogaev RC, MacGillivray TE, Naka Y, Mancini D, Massey HT, Chen L, Klodell CT, Aranda JM, Moazami N, Ewald GA, Farrar DJ, Frazier OH, HeartMate II Investigators. Extended mechanical circulatory support with a continuous-flow rotary left ventricular assist device. J Am Coll Cardiol. 2009;54:312–21.
Slaughter, Rogers LG, Milano CA, Russell SD, Conte JV, Feldman D, Sun B, Tatooles AJ, Delgado RM 3rd, Long JW, Wozniak TC, Ghumman W, Farrar DJ, Frazier OH, HeartMate II Investigators. Advanced heart failure treated with continuous-flow left ventricular assist device. N Eng J Med. 2009;361:2241–51.
John R, Kamdar F, Liao K, Colvin-Adams M, Miller L, Joyce L, Boyle A. Low thromboembolic risk for patients with the Heartmate II left ventricular assist device. J Thorac Cardiovasc Surg. 2008;136:1318–23.
Boyle AJ, Russel SD, Teuteberg JJ, Slaughter MS, Moazami N, Pagani FD, Frazier OH, Heatley G, Farrar DJ, John R. Low thromboembolism and pump thrombosis with the Heartmate II left ventricular assist device: analysis of outpatient anti-coagulation. J Heart Lung Transplant. 2009;28:881–7.
Whitson BA, Eckman P, Kamdar F, Lacey A, Shumway SJ, Liao KK, John R. Hemolysis, pump thrombus, and neurologic events in continuous-flow left ventricular assist device recipients. Ann Thorac Surg. 2014;97:2097–103.
Ravichandran AK, Parker J, Novak E, Joseph SM, Schilling JD, Ewald GA, Silvestry S. Hemolysis in left ventricular assist device: a retrospective analysis of outcomes. J Heart Lung Transplant. 2014;33:44–50.
Moazami N, Roberts K, Argenziano M, Catanese K, Mohr JP, Rose EA, Oz MC. Asymptomatic microembolism in patients with long-term ventricular assist support. ASAIO J. 1997;43:177–80.
Potapov EV, Nasseri BA, Loebe M, Kukucka M, Koster A, Kuppe H, Noon GP, DeBakey ME, Hetzer R. Transcranial detection of microembolic signals in patients with a novel nonpulsatile implantable LVAD. ASAIO J. 2001;47:249–53.
Nabavi DG, Stockmann J, Schmid C, Schneider M, Hammel D, Scheld HH, Ringelstein EB. Doppler microembolic load predicts risk of thromboembolic complications in Novacor patients. J Thorac Cardiovasc Surg. 2003;126:160–7.
Thoennissen NH, Allroggen A, Ritter M, Dittrich R, Schmid C, Schmid HH, Ringelstein EB, Nabavi DG. Influence of inflammation and pump dynamic on cerebral microembolization in patients with continuous-flow DeBakey LVAD. ASAIO J. 2006;52:243–7.
Uriel N, Morrison KA, Garan AR, Kato TS, Yuzefpolskaya M, Latif F, Restaino SW, Mancini DM, Flannery M, Takayama H, John R, Colombo PC, Naka Y, Jorde UP. Development of a novel echocardiography ramp test for speed optimization and diagnosis of device thrombosis in continuous-flow left ventricular assist devices: the Columbia ramp study. J Am Coll Cardiol. 2012;60:1764–75.
Austen WG, Howry DH. Ultrasound as a method to detect bubbles or particulate matter in the arterial line during cardiopulmonary bypass. J Surg Res. 1965;5:283–4.
Aaslid R, Markwalder TM, Nornes H. Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg. 1982;57:769–74.
Babikian VL, Hyde C, Pochay V, Winter MR. Clinical correlates of high-intensity transient signals detected on transcranial Doppler sonography in patients with cerebrovascular disease. Stroke. 1994;25:1570–3.
Tong DC, Albers GW. Transcranial Doppler-detected microemboli in patients with acute stroke. Stroke. 1995;26:1588–92.
Sliwka U, Job FP, Wissuwa D, Diehl RR, Flachskampf FA, Hanrath P, Noth J. Occurrence of transcranial Doppler high-intensity transient signals in patients with potential cardiac sources of emboli. Stroke. 1995;26:2067–70.
Schmid C, Weyand M, Nabavi DG, Hammel D, Deng MC, Ringelstein EB, Scheld HH. Cerebral and systemic embolization during left ventricular support with the Novacor N100 device. Ann Thorac Surg. 1998;65:1703–10.
Kaps M, Hansen J, Weiher M, Tiffert K, Kayser I, Droste DW. Clinically silent microemboli in patients with artificial prosthetic aortic valves are predominantly gaseous and not solid. Stroke. 1997;28:322–5.
Toda K, Sawa Y. Clinical management for complications related to implantable LVAD use. Gen Thorac Cardiovasc Surg. 2015;63:1–7.
Acknowledgments
We thank Hiroshi Nishioka, Akira Hatanaka, Megumi Komiyama, Rieko Sakai, Emiko Fujiwara, Chiyo Fujikawa, Eri Miyoshi, Ai Nagayo, Nobuaki Konishi, Shiho Tsuboi, and Yumiko Hori for their role in patient care.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seguchi, O., Saito, K., Fukuma, K. et al. Evaluation of micro-emboli in a patient with ventricular assist device support with hemolysis. J Artif Organs 18, 276–279 (2015). https://doi.org/10.1007/s10047-015-0832-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-015-0832-2