Abstract
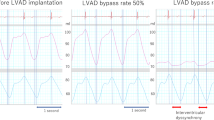
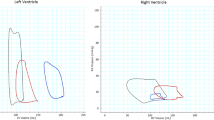
Aiming the ‘Bridge to Recovery’ course, we have developed a novel left ventricular assist device (LVAD) controlling system. It can change the rotational speed of the continuous flow LVAD, EVAHEART, synchronized with the cardiac beat. Employing this system, we have already demonstrated that myocardial oxygen consumption (MVO2), which is considered to be equivalent to native heart load, changes in the hearts of normal goats. Herein, we examined changes in goats with acute ischemic heart failure. We studied 14 goats (56.1 ± 6.9 kg) with acute ischemic heart failure due to coronary microsphere embolization. We installed the EVAHEART and drive in four modes: “circuit-clamp”, “continuous support”, “counter-pulse”, and “co-pulse”, with 50 and 100 % bypass. In comparison to the circuit-clamp mode, MVO2 was reduced to 70.4 ± 17.9 % in the counter-pulse mode and increased to 90.3 ± 14.5 % in the co-pulse mode, whereas it was 80.0 ± 14.5 % in the continuous mode, with 100 % bypass (p < 0.05). The same difference was confirmed with 50 % bypass. This means that we may have a chance to change the native heart load by controlling the LVAD rotation in synchrony with the cardiac rhythm, so we named our controller as the Native Heart Load Control System (NHLCS). Employing changeable MVO2 with NHLCS according to the patient’s condition may provide more opportunity for native heart recovery with LVAD, especially for patients with ischemic heart diseases.






Similar content being viewed by others
References
Frazier OH, Benedict CR, Radovancevic B, Bick RJ, Capek P, Springer WE, Macris MP, Delgado R, Buja LM. Improved left ventricular function after chronic left ventricular unloading. Ann Thorac Surg. 1996;62:675–81. discussion 681-672.
Birks EJ, Tansley PD, Hardy J, George RS, Bowles CT, Burke M, Banner NR, Khaghani A, Yacoub MH. Left ventricular assist device and drug therapy for the reversal of heart failure. N Engl J Med. 2006;355:1873–84.
Dandel M, Weng Y, Siniawski H, Potapov E, Lehmkuhl HB, Hetzer R. Long-term results in patients with idiopathic dilated cardiomyopathy after weaning from left ventricular assist devices. Circulation. 2005;112:I37–45.
Saito S, Nishinaka T, Yamazaki K. Long-term circulatory support with a left ventricular assist device therapy in Japan. Circ J. 2010;74:624–5.
Matsumiya G, Saitoh S, Sakata Y, Sawa Y. Myocardial recovery by mechanical unloading with left ventricular assist system. Circ J. 2009;73:1386–92.
Slaughter MS, Rogers JG, Milano CA, Russell SD, Conte JV, Feldman D, Sun B, Tatooles AJ, Delgado RM, Long JW, Wozniak TC, Ghumman W, Farrar DJ, Frazier OH, HeartMate II Investigators. Advanced heart failure treated with continuous-flow left ventricular assist device. N Engl J Med. 2009;361:2241–51.
Ji B, Ündar A. An evaluation of the benefits of pulsatile versus nonpulsatile perfusion during cardiopulmonary bypass procedures in pediatric and adult cardiac patients. ASAIO J. 2006;52:357–61.
Loebe M, Koster A, Sänger S, Potapov EV, Kuppe H, Noon GP, Hetzer R. Inflammatory response after implantation of a left ventricular assist device: comparison between the axial flow MicroMed DeBakey VAD and the pulsatile Novacor device. ASAIO J. 2001;47:272–4.
Nishinaka T, Tatsumi E, Taenaka Y, Takano H, Koyanagi H. Influence of pulsatile and nonpulsatile left heart bypass on the hormonal circadian rhythm. ASAIO J. 2000;46:582–6.
Toda K, Tatsumi E, Taenaka Y, Masuzawa T, Miyazaki K, Wakisaka Y, Nakatani T, Baba Y, Eya K, Takano H. How does the sympathetic nervous system behave during non pulsatile circulation? ASAIO J. 1995;41:M465–8.
Tatsumi E, Toda K, Taenaka Y, Miyazaki K, Masuzawa T, Nakatani T, Baba Y, Yagura A, Eya K, Wakisaka Y. Acute phase responses of vasoactive hormones to non pulsatile systemic circulation. ASAIO J. 1995;41:M460–5.
Tatsumi E, Miyazaki K, Toda K, Taenaka Y, Nakatani T, Baba Y, Masuzawa T, Wakisaka Y, Eya K, Nishimura T, Takewa Y, Ohno T, Takano H. Influence of non pulsatile systemic circulation on tissue blood flow and oxygen metabolism. ASAIO J. 1996;42:M757–62.
Tatsumi E, Miyazaki K, Toda K, Taenaka Y, Nakatani T, Baba Y, Masuzawa T, Eya K, Wakisaka Y, Nishimura T, Takewa Y, Ohno T, Takano H. Altered oxygen metabolic conditions associated with increased norepinephrine levels in a nonpulsatile systemic circulation. ASAIO J. 1996;42:M854–7.
Undar A, Masai T, Frazier OH, Fraser CDJ. Pulsatile and nonpulsatile flows can be quantified in terms of energy equivalent pressure during cardiopulmonary bypass for direct comparisons. ASAIO J. 1999;45:610–4.
Vandenberghe S, Segers P, Antaki JF, Meyns B, Verdonck PR. Hemodynamic modes of ventricular assist with a rotary blood pump: continuous, pulsatile, and failure. ASAIO J. 2005;51:711–8.
Bartoli CR, Giridharan GAS, Litwak KNP, Sobieski M, Prabhu SD, Slaughter MS, Koenig SCS. Hemodynamic responses to continuous versus pulsatile mechanical unloading of the failing left ventricle. ASAIO J. 2010;56:410–6.
Orime Y, Shiono M, Nakata K, Hata M, Sezai A, Yamada H, Iida M, Kashiwazaki S, Nemoto M, Kinoshita J, Kojima T, Saito T, Sezai Y. The role of pulsatility in end-organ microcirculation after cardiogenic shock. ASAIO J. 1996;42:M724–8.
Jung JS, Son HS, Lim CH, Sun K. Pulsatile versus nonpulsatile flow to maintain the equivalent coronary blood flow in the fibrillating heart. ASAIO J. 2007;53:785–90.
Satoh H, Miyamoto Y, Shimazaki Y, Kadoba K, Masai T, Yagura A, Matsuda H. Comparison between pulsatile and nonpulsatile circulatory assist for the recovery of shock liver. ASAIO J. 1995;41:M596–600.
Anstadt MP, Tedder M, Hegde SS, Perez-Tamayo RA, Crain BJ, Khian Ha VL, Abdel-Aleem S, White WD, Lowe JE. Pulsatile versus nonpulsatile reperfusion improves cerebral blood flow after cardiac arrest. Ann Thorac Surg. 1993;56:453–61.
Henze T, Stephan H, Sonntag H. Cerebral dysfunction following extracorporeal circulation for aortocoronary bypass surgery: no differences in neuropsychological outcome after pulsatile versus nonpulsatile flow. Thorac Cardiovasc Surg. 1990;38:65–8.
Nishinaka T, Tatsumi E, Nishimura T, Taenaka Y, Imada K, Takano H, Koyanagi H. Effects of reduced pulse pressure to the cerebral metabolism during prolonged nonpulsatile left heart bypass. Artif Organs. 2000;24:676–9.
Wilson E, Mai Q, Sudhir K, Weiss RH, Ives HE. Mechanical strain induces growth of vascular smooth muscle cells via autocrine action of PDGF. J Cell Biol. 1993;123:741–7.
Nishimura T, Tatsumi E, Takaichi S, Taenaka Y, Wakisaka Y, Nakatani T, Masuzawa T, Takewa Y, Nakamura M, Endo S, Nakata M, Takano H. Prolonged nonpulsatile left heart bypass with reduced systemic pulse pressure causes morphological changes in the aortic wall. Artif Organs. 1998;22:405–10.
Nishimura T, Tatsumi E, Nishinaka T, Taenaka Y, Nakata M, Takano H. Prolonged nonpulsatile left heart bypass diminishes vascular contractility. Int J Artif Organs. 1999;22:492–8.
Nishimura T, Tatsumi E, Taenaka Y, Nishinaka T, Nakatani T, Masuzawa T, Nakata M, Nakamura M, Endo S, Takano H. Effects of long-term nonpulsatile left heart bypass on the mechanical properties of the aortic wall. ASAIO J. 1999;45:455–9.
Nishimura T, Tatsumi E, Takaichi S, Taenaka Y, Wakisaka Y, Nakatani T, Masuzawa T, Takewa Y, Nakamura M, Endo S, Sohn YS, Takano H. Morphologic changes of the aortic wall due to reduced systemic pulse pressure in prolonged non pulsatile left heart bypass. ASAIO J. 1997;43:M691–5.
Yamazaki K, Kihara S, Akimoto T, Tagusari O, Kawai A, Umezu M, Tomioka J, Kormos RL, Griffith BP, Kurosawa H. EVAHEART: an implantable centrifugal blood pump for long-term circulatory support. Jpn J Thorac Cardiovasc Surg. 2002;50:461–5.
Yamazaki K, Saito S, Kihara S, Tagusari O, Kurosawa H. Completely pulsatile high flow circulatory support with a constant-speed centrifugal blood pump: mechanisms and early clinical observations. Gen Thorac Cardiovasc Surg. 2007;55:158–62.
Ando M, Takewa Y, Nishimura T, Yamazaki K, Kyo S, Ono M, Tsukiya T, Mizuno T, Taenaka Y, Tatsumi E. A novel counterpulsation mode of rotary left ventricular assist devices can enhance myocardial perfusion. J Artif Organs. 2011;14:185–91.
Ando M, Takewa Y, Nishimura T, Yamazaki K, Kyo S, Ono M, Tsukiya T, Mizuno T, Taenaka Y, Tatsumi E. Coronary vascular resistance increases under full bypass support of centrifugal pumps-relation between myocardial perfusion and ventricular workload during pump support. Artif Organs. 2012;36(1):105–10.
Ando M, Nishimura T, Takewa Y, Yamazaki K, Kyo S, Ono M, Tsukiya T, Mizuno T, Taenaka Y, Tatsumi E. Electrocardiogram-synchronized rotational speed change mode in rotary pumps could improve pulsatility. Artif Organs. 2011;35:941–7.
Ando M, Nishimura T, Takewa Y, Kyo S, Ono M, Taenaka Y, Tatsumi E. Creating an ideal “off-test mode” for rotary left ventricular assist devices: establishing a safe and appropriate weaning protocol after myocardial recovery. J Thorac Cardiovasc Surg. 2012;143(5):1176–82.
Ando M, Nishimura T, Takewa Y, Ogawa D, Yamazaki K, Kashiwa K, Kyo S, Ono M, Taenaka Y, Tatsumi E. A novel counterpulse drive mode of continuous-flow left ventricular assist devices can minimize intracircuit backward flow during pump weaning. J Artif Organs. 2011;14:74–9.
Ando M, Nishimura T, Takewa Y, Ogawa D, Yamazaki K, Kashiwa K, Kyo S, Ono M, Taenaka Y, Tatsumi E. What is the ideal off-test trial for continuous-flow ventricular-assist-device explantation? Intracircuit back-flow analysis in a mock circulation model. J Artif Organs. 2011;14:70–3.
Umeki A, Nishimura T, Ando M, Takewa Y, Yamazaki K, Kyo S, Ono M, Tsukiya T, Mizuno T, Taenaka Y, Tatsumi E. Alteration of LV end-diastolic volume by controlling the power of the continuous-flow LVAD, so it is synchronized with cardiac beat: development of a native heart load control system (NHLCS). J Artif Organs. 2012;15(2):128–33.
Suga H, Goto Y, Futaki S, Kawaguchi O, Yaku H, Hata K, Takasago T. Systolic pressure-volume area (PVA) as the energy of contraction in Starling’s law of the heart. Heart Vessels. 1991;6:65–70.
Suga H, Yasumura Y, Nozawa T, Futaki S, Tanaka N, Uenishi M. Ventricular systolic pressure-volume area (PVA) and contractile state (Emax) determine myocardial oxygen demand. Adv Exp Med Biol. 1988;222:421–30.
Suga H, Igarashi Y, Yamada O, Goto Y. Cardiac oxygen consumption and systolic pressure volume area. Basic Res Cardiol. 1986;81:39–50.
Suga H. Total mechanical energy of a ventricle model and cardiac oxygen consumption. Am J Physiol. 1979;236:H498–505.
Suga H. Ventricular energetics. Physiol Rev. 1990;70:247–77.
Tuzun E, Eya K, Chee HK, Conger JL, Bruno NK, Frazier OH, Kadipasaoglu KA. Myocardial hemodynamics, physiology, and perfusion with an axial flow left ventricular assist device in the calf. ASAIO J. 2004;50:47–53.
Goldstein AH, Monreal G, Kambara A, Spiwak AJ, Schlossberg ML, Abrishamchian AR, Gerhardt MA. Partial support with a centrifugal left ventricular assist device reduces myocardial oxygen consumption in chronic, ischemic heart failure. J Card Fail. 2005;11:142–51.
Voitl P, Vollkron M, Bergmeister H, Wieselthaler G, Schima H. Coronary hemodynamics and myocardial oxygen consumption during support with rotary blood pumps. Artif Organs. 2009;33:77–80.
Kawaguchi O, Pae WE, Daily WB, Sapirstein JS, Pierce WS. Left ventricular mechanoenergetics during asynchronous left atrial-to-aortic bypass. Effects of pumping rate on cardiac workload and myocardial oxygen consumption. J Thorac Cardiovasc Surg. 1995;110:793–9.
Pantalos GM, Marks JD, Riebman JB, Everett SD, Burns GL, Burton NA, DePaulis R. Left ventricular oxygen consumption and organ blood flow distribution during pulsatile ventricular assist. ASAIO Trans. 1988;34:356–60.
Klocke R, Tian W, Kuhlmann MT, Nikol S. Surgical animal models of heart failure related to coronary heart disease. Cardiovasc Res. 2007;74:29–38.
Dixon JA, Spinale FG. Large animal models of heart failure: a critical link in the translation of basic science to clinical practice. Circ Heart Fail. 2009;2:262–71.
Gill RM, Jones BD, Corbly AK, Wang J, Braz JC, Sandusky GE, Shen W. Cardiac diastolic dysfunction in conscious dogs with heart failure induced by chronic coronary microembolization. Am J Physiol Heart Circ Physiol. 2006;291:H3154–8.
Hayashi Y, Hamada M, Hiwada K. Characterization of left ventricular opacification using sonicated serum albumin in patients with dilated cardiomyopathy and myocardial infarction. Jpn Circ J. 1998;62:91–6.
Tuzun E, Narin C, Gregoric ID, Cohn WE, Frazier OH. Ventricular assist device outflow-graft site: effect on myocardial blood flow. J Surg Res. 2011;171:71–5.
May-Newman K, Hillen B, Dembitsky W. Effect of left ventricular assist device outflow conduit anastomosis location on flow patterns in the native aorta. ASAIO J. 2006;52:132–9.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Umeki, A., Nishimura, T., Takewa, Y. et al. Change in myocardial oxygen consumption employing continuous-flow LVAD with cardiac beat synchronizing system, in acute ischemic heart failure models. J Artif Organs 16, 119–128 (2013). https://doi.org/10.1007/s10047-012-0682-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-012-0682-0