Abstract
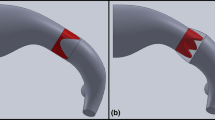
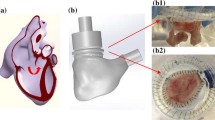
The purpose of this study was to examine the hemodynamic characteristics of expanded polytetrafluoroethylene (ePTFE) pulmonary valves with bulging sinuses quantitatively in a pediatric pulmonary mechanical circulatory system designed by us, in order to propose the optimal design for clinical applications. In this study, we developed a pediatric pulmonary mock circulation system, which consisted of a pneumatic right ventricular model, a pulmonary heart valve chamber, and a pulmonary elastic compliance tubing with resistive units. The hemodynamic characteristics of four different types of ePTFE valves and a monoleaflet mechanical heart valve were examined. Relationships between the leaflet movements and fluid characteristics were evaluated based on engineering analyses using echocardiography and a high-speed video camera under the pediatric circulatory conditions of the mock system. We successfully performed hemodynamic simulations in our pediatric pulmonary circulatory system that could be useful for quantitatively evaluating the pediatric heart valves. In the simulation study, the ePTFE valve with bulging sinuses exhibited a large eddy in the vicinity of the leaflets, whereas the straight tubing exhibited turbulent flow. The Reynolds number obtained in the valve with bulging sinuses was calculated to be 1667, which was smaller than that in the straight tubing (R e = 2454).
The hemodynamic characteristics of ePTFE pediatric pulmonary heart valves were examined in our mock circulatory system. The presence of the bulging sinuses in the pulmonary heart valve decreased the hydrodynamic energy loss and increased the systolic opening area. Based on an in vitro experiment, we were able to propose an optimal selection of pulmonary valve design parameters that could yield a more sophisticated pediatric ePTFE valve shape.










Similar content being viewed by others
References
Fiore AC, Peigh PS, Robison RJ, Glant MD, King H, Brown JW. Valved and nonvalved right ventricular–pulmonary arterial extracardiac conduits. An experimental comparison. J Thorac Cardiovasc Surg. 1983;86:490–7.
Ando M, Imai Y, Hoshino S, Ishihara K. Autologous reconstruction of pulmonary trunk at reoperation after extracardiac conduit repair. Ann Thorac Surg. 1995;59:621–5.
Ando M, Takahashi Y. Ten-year experience with handmade trileaflet polytetrafluoroethylene valved conduit used for pulmonary reconstruction. J Thorac Cardiovasc Surg 2009;137:124–131.
Brown JW, Ruzmetov MR, Rodefeld MD, Vijay P, Turrentine MW. Right ventricular outflow tract reconstruction with an allograft conduit in non-Ross patients: risk factors for allograft dysfunction and failure. Ann Thorac Surg. 2005;80:655–64.
Dur O, Yoshida M, Manor P, Mayfield A, Wearden PD, Morell VO, Pekkan K. In vitro evaluation of right ventricular outflow tract reconstruction with bicuspid valved polytetrafluoroethylene conduit. Artif Organs. 2010;34:1010–6.
Molina JE. Preliminary experience with GORE-TEX grafting for right ventricle–pulmonary artery conduits. Tex Heart Inst J. 1986;13:137–42.
Elkins RC. The Ross operation: a 12-year experience. Ann Thorac Surg. 1999;68:S14–8.
Bielefeld MR, Bishop DA, Campbell DN, Mitchell MB, Grover FL, Clarke DR. Reoperative homograft right ventricular outflow tract reconstruction. Ann Thorac Surg. 2001;71:482–8.
Oosterhof T, Meijboom FJ, Vliegen HW, Hazekamp MG, Zwinderman AH, Bouma BJ, van Dijk AP, Mulder BJ. Long-term follow-up of homograft function after pulmonary valve replacement in patients with tetralogy of Fallot. Eur Heart J. 2006;27:1478–84.
Iwai S, Torikai K, Coppin CM, Sawa Y. Minimally immunogenic decellularized porcine valve provides in situ recellularization as a stentless bioprosthetic valve. J Artif Organs. 2007;10:29–35.
Sekarski N, van Meir H, Rijlaarsdam MEB, Schoof PH, Koolbergen DR, Hruda J, von Segesser LK, Meijboom EJ, Hazekamp MG. Right ventricular outflow tract reconstruction with the bovine jugular vein graft: 5 years’ experience with 113 patients. Ann Thorac Surg. 2007;84:599–605.
Boethig D, Goerler H, Wasthoff-Bleck M, Ono M, Daiber A, Haverich A, Breymann T. Evaluation of 188 consecutive homografts implanted in pulmonary position after 20 years. Eur J Cardiothorac Surg. 2007;32:133–42.
Tokunaga S, Masuda M, Shiose A, Tomita Y, Morita S, Tominaga R. Isolated pulmonary valve replacement: analysis of 27 years of experience. J Artif Organs. 2008;11:130–3.
Brown JW, Ruzmetov MR, Estayeb O, Rodefeld MD, Turrentine MW. Performance of SynerGraft decellularized pulmonary homograft in patients undergoing a Ross procedure. Ann Thorac Surg. 2011;91:416–23.
Yamagishi M, Emoto T, Wada Y, Oka T. Pulmonary reconstruction in the Ross procedure. Combined autologous aortic and polytetrafluoroethylene valve. J Thorac Cardiovasc Surg. 1998;116:1076–7.
Miyazaki T, Yamagishi M, Maeda Y, Yamamoto Y, Taniguchi S, Sasaki Y, Yaku H. Expanded polytetrafluoroethylene conduits and patches with bulging sinuses and fan-shaped valves in right ventricular outflow tract reconstruction: multicenter study in Japan. J Thorac Cardiovasc Surg. 2011; [Epub ahead of print].
Peacock JA. An in vitro study of the onset of turbulence in the sinus of Valsalva. Circ Res. 1990;67:448–80.
Yamanami M, Yahata Y, Tajikawa T, Ohba K, Watanabe T, Kanda K, Yaku H, Nakayama Y. Preparation of in vivo tissue-engineered valved conduit with the sinus of Valsalva. J Artif Organs. 2010;13:106–12.
Cooke J, Hertzberg J, Boardman M, Shandas R. Characterizing vortex ring behavior during ventricular filling with Doppler echocardiography: an in vitro study. Ann Biomed Eng. 2004;32:245–56.
Tanaka M, Sakamoto T, Sugawara S, Nakajima H, Katahira Y, Ohtsuki S, Kanai H. Blood flow structure and dynamics, and ejection mechanism in the left ventricle: analysis using echo-cardiography. J Cardiol. 2008;52:86–101.
Yap CH, Dasi LP, Yoganathan AP. Dynamic hemodynamic energy loss in normal and stenosed aortic valves. J Biomech Eng. 2010;132:021005.
Yoganathan AP, He Z, Jones C. Fluid mechanics of heart valves. Ann Rev Biomed Eng. 2004;6:331–62.
Acknowledgments
This study was supported by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (no. 22689047).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Suzuki, I., Shiraishi, Y., Yabe, S. et al. Engineering analysis of the effects of bulging sinuses in a newly designed pediatric pulmonary heart valve on hemodynamic function. J Artif Organs 15, 49–56 (2012). https://doi.org/10.1007/s10047-011-0609-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-011-0609-1