Abstract
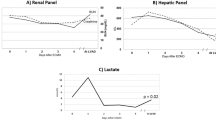
Implantation of left ventricular assist device (LVAD) as a bridge to recovery or transplantation is a widely accepted treatment modality. Preexisting organ dysfunction is thought to unfavorably affect patient survival after implantation of a ventricular assist device (VAD). We present our experience using extracorporeal membrane oxygenation (ECMO) in patients with cardiogenic shock to stabilized organ function prior to LVAD implantation. Between September 2006 and March 2008, five patients in cardiogenic shock with preexisting organ dysfunction (impaired liver and kidney function) were supported with ECMO before LVAD implantation. ECMO-LVAD interval was 8 ± 4 days. All patients were transferred to a LVAD. At the LVAD implantation time, glutamic-oxaloacetic transaminase (GOT) decreased from 206.25 ± 106.93 Ul −1 to 70.6 ± 32.9 U l−1, glutamic-pyruvic transaminase (GPT) decreased from 333.5 ± 207.3 U l−1 to 77.8 ± 39.7 U l−1, and creatinine decreased from 2.2 ± 0.9 mg dl−1 to 1.2 ± 0.2 mg dl−1. One patient died while on LVAD support due to not device related sepsis. One patient received successful heart transplantation. Overall survival was 80%. In all patients, we removed the ECMO 3 days after LVAD implantation. After removal of the ECMO there was no right heart failure. ECMO support can immediately stabilize circulation and provide organ perfusion in patients with cardiogenic shock. After improvement of organ function, LVAD implantation can be performed successfully in this patient collective. To avoid right ventricular failure, the ECMO should not be removed at the time of LVAD implantation, and used as a right ventricular support for the immediate postoperative period.
Similar content being viewed by others
References
McCarthy PM, Portner PM, Tobler HG, Starnes VA, Ramasamy N, Oyer PE. Clinical experience with the Novacor ventricular assist system. Bridge to transplantation and the transistion to permanent application. J Thorac Cardiovasc Surg 1991;102:578–586
Kasirajan V, McCarthy PM, Hoercher KJ, Starling RC, Young JB, Banbury MK, Smedira NG. Clinical experience with long term use of implantable left ventricular assist devices: indications, implantation, and outcomes. Semin Thorac Cardiovasc Surg 2000;12:229–237
Farrar DJ, Thoratec Ventricular Assist Device Principal Investigators. Preoperative predictors of survival in patients with Thoratec ventricular assist devices as a bridge to transplantation. J Heart Lung Transplant 1994;13:93–101
Frazier OH, Rose EA, Macmanus Q, Burton NA, Lefrak EA, Poirier VL, Dasse KA. Multicenter clinical evaluation of the HeartMate 1000 IP left ventricular assist device. Ann Thorac Surg 1992;53:1080–90
Reinhartz O, Farrar DJ, Hershon JH, Avery GJ, Haeusslein EA, Hill JD. Importance of preoperative liver function as a predictor of survival in patients supported with thoratec ventricular assist devices as a bridge to transplantation. J Thorac Cardiovasc Surg 1998;116:633–640
Doll N, Kiaii B, Borger M, Bucerius J, Krämer K, Schmitt DV, Walther T, Mohr FW. Five-year results of 219 consecutive patients treated with extracorporeal membrane oxygenation for refractory postoperative cardiogenic shock. Ann Thorac Surg 2004;77:151–157
Chen YS, Ko WJ, Lin FY, Huang SC, Chou TF, Chou NK, Hsu RB, Wang SS, Chu SH. Preliminary result of an algorithm to select proper ventricular assist devices for high risk patients with extracorporeal membrane oxygenation support. J Heart Lung Transplant 2001;20:850–857
Levi D, Marelli D, Plunkett M, Alejos J, Bresson J, Tran J, Eisenring C, Sadeghi A, Galindo A, Fazio D, George B, Laks H. Use of assist devices and ECMO to bridge pediatric patients with cardiomyopathy to transplantation. J Heart Lung Transplant 2002;21:760–770
Kihara S, Kawai A, Endo M, Koyanagi H, Kurosawa H. Extracorporeal membrane oxygenation and left ventricular assist device: a case of double mechanical bridge. Heart Vessels 2002;16:164–166
Murashita T, Eya K, Miyatake T, Kamikubo Y, Shiiya N, Yasuda K, Sasaki S. Outcome of the perioperative use of percutaneous cardiopulmonary support for adult cardiac surgery: factors affecting hospital mortality. Artif Organs 2004;28:189–195
Hoefer D, Ruttmann E, Poelzl G, Kilo J, Hoermann C, Margreiter R, Laufer G, Antretter H. Outcome evaluation of the bridge to bridge concept in patients with cardiogenic shock. Ann Thorac Surg 2006;82:28–34
Dunn GP, Hayes P, Breen KJ, Schenker S. The liver in congestive heart failure: a review. Am J Med Sci 1973;265:174–189
Editorial. Ischemic hepatitis. Lancet 1985;1:1019–1020
Gitlin N, Serio KM. Ischemic hepatitis: widening horizons. Am J Gastroenterol 1992;87:831–836
McCarthy PM, Smedira NO, Vargo RL, Goormastic M, Hobbs RE, Starling RC, Young JB. One hundred patients with the Heart-Mate left ventricular assist device: evolving concepts and technology. J Thorac Cardiovasc Surg 1998;115:904–912
Magliato KE, Kleisli T, Soukiasian HJ, Tabrizi R, Coleman B, Hickey A, Czer LS, Blanche C, Cheng W, Fontana GP, Kass RM, Raissi SS, Trento A. Biventricular support in patients with profound cardiogenic shock: a single center experience. ASAIO J 2003;49:475–479
Pagani FD, Lynch W, Swaniker F, Dyke DB, Bartlett R, Koelling T, Moscucci M, Deeb GM, Bolling S, Monaghan H, Aaronson KD. Extracorporeal life support to left ventricular assist device bridge to heart transplant: a strategy to optimize survival and resource utilization. Circulation 1999;100:II206–210
Pennington DG, Reedy Je, Swartz MT, McBride LR, Seacord LM, Naunheim KS, Miller LW. Univentricular versus biventricular assist device support. J Heart Lung Transplant 1991;10:258–263
Bakhtiary F, Keller H, Dogan S, Dzemali O, Oezaslan F, Meininger D, Ackermann H, Zwissler B, Kleine P, Moritz A. Venoarterial extracorporeal membrane oxygenation for treatment of cardiogenic shock: clinical experiences in 45 adult patients. J Thorac Cardiovasc Surg 2008;135:382–388
Jacobson J. Nitric oxide platelet protectant properties during cardiopulmonary bypass/ECMO. J Extra Corpor Technol 2002;34:144–147
Steinlechner B, Dworschak M, Birkenberg B, Duris M, Zeidler P, Fischer H, Milosevic L, Wieselthaler G, Wolner E, Quehenberger P, Jilma B. Platelet dysfunction in outpatients with left ventricular assist devices. Ann Thorac Surg 2009;87:131–137
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Scherer, M., Moritz, A. & Martens, S. The use of extracorporeal membrane oxygenation in patients with therapy refractory cardiogenic shock as a bridge to implantable left ventricular assist device and perioperative right heart support. J Artif Organs 12, 160–165 (2009). https://doi.org/10.1007/s10047-009-0464-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-009-0464-5