Abstract
In the wake of the Affordable Care Act, some US states expanded Medicaid eligibility to low-income, working-age adults while others did not. This study investigates whether this divergence induces migration across state borders to obtain Medicaid, especially in border regions of expansion states. It compares border with interior regions’ in-migration in the concerned subgroup before and after the Medicaid expansion in linear probability difference-in-difference and triple difference regression frameworks. Using individual-level data from the American Community Surveys over 2012–2017, this study finds only a statistically significant increase in in-migration to border regions after the expansion in Arkansas. The differing results across states could stem from statistical power issues of the employed regression analysis but might also result from state peculiarities. In Arkansas, the odds of having migrated increase by about 48% in its border regions after the Medicaid expansion compared to before and control regions. If all additional migrants take up Medicaid, the number of Medicaid beneficiaries in these regions increases by approximately 4%. Thus, even if the induced migration is statistically significant, it appears unlikely to impose meaningful fiscal externalities at the regional level.
Zusammenfassung
Im Zuge des Affordable Care Acts haben einige US-Bundesstaaten den Anspruch auf Medicaid auf einkommensschwache Erwachsene im arbeitsfähigen Alter ausgeweitet, während andere Bundesstaaten dies nicht taten. Diese Studie untersucht, ob diese Divergenz zu einer Migration über die Bundesstaatsgrenzen führt, um Medicaid zu erhalten, insbesondere in Grenzregionen von Reformbundesstaaten. Sie vergleicht die Zuwanderung in Grenzregionen mit der Zuwanderung in das Landesinnere in der betroffenen Gruppe vor und nach der Medicaid-Ausweitung in linearen Wahrscheinlichkeits-Differenz-in-Differenz- und Dreifach-Differenz-Regressionsanalysen. Unter Verwendung von Daten auf Individualebene aus den American Community Surveys der Jahre 2012–2017 findet diese Studie nur in Arkansas einen statistisch signifikanten Anstieg der Zuwanderung in die Grenzregionen nach der Ausweitung. Die unterschiedlichen Ergebnisse in den einzelnen Bundesstaaten könnten von Problemen mit der statistischen Aussagekraft der durchgeführten Regressionsanalyse herrühren. Sie könnten aber auch aus Besonderheiten der jeweiligen Bundesstaaten resultieren. Eine zufällig ausgewählte Person in den Grenzregionen von Arkansas hat nach der Medicaid-Ausweitung eine um 48 % erhöhte Wahrscheinlichkeit zugewandert zu sein im Vergleich zu vorher und den Kontrollregionen. Falls alle zusätzlichen Migranten Medicaid in Anspruch nehmen, steigt die Zahl der Medicaid-Empfänger in diesen Regionen um etwa 4 %. Es scheint somit unwahrscheinlich, dass die induzierte Migration zu bedeutenden fiskalischen Externalitäten auf regionaler Ebene führt, selbst wenn der Migrationseffekt statistisch signifikant ist.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
States with relatively high welfare benefits are long believed to attract low-income individuals from lower-benefit states, acting as “welfare magnets” (Armenter and Ortega 2010; Borjas 1999; Brown and Oates 1987). Similar reasoning might apply to the expansion of public health insurance programs such as Medicaid. Notably, the Patient Protection and Affordable Care Act (ACA) includes a Medicaid expansion from 2014 onward to low-income, non-disabled, working-age adults. However, not all states decided to implement it. Should expansion states then worry about an inflow of low-income individuals attracted by Medicaid?
Previous studies could not find any state-level migration effects induced by Medicaid expansions (Alm and Enami 2017; Goodman 2017; Schwartz and Sommers 2014). However, much of this migration would arise in regions at the state border (McKinnish 2005). This phenomenon can strain border regions considerably, even if the overall state-level migration effects are negligible.
Therefore, this paper aims at evaluating ACA Medicaid-induced border migration. It compares the in-migration of low-income, working-age individuals to border and interior regions of the same state before and after the ACA in difference-in-difference and triple difference frameworks based on individual-level American Community Survey (ACS) data (Ruggles et al. 2020).
This paper is not the first to study border migration induced by the ACA Medicaid expansion. Most notably, Goodman (2017) considers migration of individuals from border regions to border regions by restricting its sample accordingly. However, this substantially decreases the available number of observations and results in statistical power issues, making it impossible for Goodman (2017) to identify any border migration effects.
To overcome these issues, this paper uses the border-versus-interior-regions approach suggested by McKinnish (2005, 2007) and adapted to the 2006 Massachusetts Medicaid expansion by Alm and Enami (2017). This approach compares the evolution in migration rates to border regions to the ones of interior regions for the state enacting a reform. At a state border with a Medicaid coverage difference, the border regions on the expansion side should attract more in-migrants after the Medicaid expansion than before, and this increase should be larger than in interior regions. Using this approach, Alm and Enami (2017) could identify border migration effects for the Massachusetts Medicaid expansion.
The contribution of the present study to the literature is twofold. First, it is the first one that applies the border-versus-interior-regions approach to the ACA Medicaid expansion and evaluates Medicaid migration effects for five states at once (Arkansas, Illinois, Iowa, Maryland, and New Mexico). Second, the present study extends until 2017, adding three more years to Goodman’s (2017) observation period. This allows both to increase the number of observations and study slightly longer-term effects of the Medicaid expansion on migration.
This paper can only identify a statistically significant, positive Medicaid migration effect for Arkansas. The other states exhibit insignificant migration effects, which sometimes even turn negative, indicating that no Medicaid migration occurs. The differing results across states could stem from statistical power issues but might also result from state peculiarities.
For Arkansas, the odds of having migrated are about 48% higher post-ACA in concerned border regions compared to before the ACA and interior regions. However, the effect is small in the aggregate due to the baseline migration odds of about 0.05. If all additional migrants take up Medicaid, the number of Medicaid beneficiaries in these regions increases by less than 4.2%. This increase seems manageable, probably not imposing a meaningful fiscal externality on regional budgets.
The following section discusses the existing literature on public services migration in the US in more detail. Sect. 3 provides background on the ACA Medicaid expansion, the data, and study units, while Sect. 4 presents the empirical strategy and discusses the parallel trend test results. Sect. 5 presents the main results, while Sect. 6 discusses the reasons for the many insignificant results. Sect. 7 performs robustness checks, while Sect. 8 concludes.
2 Public services and internal migration
The basic economic migration model constitutes migration decisions as a cost-benefit analysis. In this framework, individuals weigh the costs and benefits of their location options and migrate when the benefits from relocation outweigh the costs (Molloy et al. 2011; Tiebout 1956). Three main reasons for migration emerge from the literature: economic opportunity, public goods/services provision, and natural amenities. Public health insurance, such as Medicaid, can be considered a special kind of public services.
Public services migration also includes welfare migration, which has been studied extensively. It is related to the welfare-magnet theory. States with relatively high welfare benefits should attract low-income individuals from low-benefit states while concurrently retaining those already living in the state (Kennan and Walker 2013). Thus, they act as “magnets” for low-income individuals. This could lead to a race to the bottom in setting benefit levels due to competition among states (Armenter and Ortega 2010; Bailey and Rom 2004; Saavedra 2000).
Welfare migration is more likely to occur to and from border regions. In this case, interstate migration costs are lower as physical relocation and information costs are lower, while networks are more likely to persist (Baker 2020; Greenwood 1997; McKinnish 2005). Welfare recipients have limited financial means, restraining their possibility of moving long distances (McKinnish 2005, 2007; Snarr and Burkey 2006). Concurrently, state public policies, such as welfare benefits and Medicaid coverage, change abruptly at the state border. This results in appreciable differences in benefit levels within a short-distance move (McKinnish 2005). In sum, border regions play a particular role in welfare migration as comparatively short-distance moves can already lead to significant changes in the policy environment while only small migration costs arise.
There exists a sizable empirical literature on welfare migration. Welfare benefit generosity appears to have a positive but moderate effect on migration (Bailey 2005; Brueckner 2000; De Jong et al. 2005; Gelbach 2004; Kennan and Walker 2010). This effect’s scale is typically not large enough to matter in the aggregate for states’ budgets (Gelbach 2004).
An innovative approach by McKinnish (2005, 2007) evaluates welfare migration by exploiting that welfare migration is more likely to occur in border regions. It compares welfare participation rates in state border counties to interior counties’ ones for both high- and low-benefit states. More welfare-generous states should have higher welfare participation rates in their border regions compared to both interior ones and the neighboring low-benefit states’ regions due to short-distance interstate border migration (McKinnish 2005). This hypothesis is tested by estimating a difference-in-difference model. This approach de facto underestimates the actual migration effect as some migrants might also move to or from interior regions. Another study extends this framework to individual-level microdata and adds a time dimension by using observations from the 1980 and 1990 Censuses (McKinnish 2007). The thereby obtained results are similar to other studies on welfare migration in finding significant but small welfare-migration effects (McKinnish 2005, 2007).
Medicaid might also induce migration. This migration is not necessarily identical to the welfare benefits one as the target group and eligibility rules differ (Goodman 2017). Potenzial and current Medicaid beneficiaries tend to move, ceteris paribus, to states with higher Medicaid benefits (Cebula and Clark 2013). The decision to expand Medicaid might hence induce in-migration to an expansion state.
There were already Medicaid expansions in selected US states before the ACA. Several studies have exploited these policy changes to analyze their effect on interstate migration. They do not find any state-level effect of Medicaid expansion on migration (Alm and Enami 2017; Schwartz and Sommers 2014). Global effects could neither be found for the ACA Medicaid expansion, except for particular subpopulations such as homeless individuals (Baker 2020; Goodman 2017; Kumar 2021). However, states are quite large and far apart, rendering migration mostly long-distance and hence costly.
Relevant border migration might nevertheless occur as it is less costly (Baker 2020). Border migration might be so locally concentrated that migration flows are insignificant at the state level. They might still distinctively impact border regions as the latter have to cope with the low-income migrant influx and its associated costs (for instance, for hospital infrastructure, roads, housing, utilities provision, and police, while local taxes do not increase proportionally). Border migration effects have been found for the 2006 Massachusetts Medicaid expansion in border cities (Alm and Enami 2017). These effects are identified by comparing the population growth of low-income individuals in border cities to its growth in Massachusetts’s interior cities before and after the reform in a difference-in-difference framework in the spirit of McKinnish (2005, 2007). If Medicaid-expansion-induced border migration occurs, this population growth should be ceteris paribus higher in border cities compared to interior ones and pre-expansion growth rates. Empirically, a relatively large migration effect appears for cities close to the border. However, it decreases rapidly with increasing distance to the border and disappears completely beyond 25 km from the border (Alm and Enami 2017). The results also hold when employing triple differences by additionally comparing to either population growth of higher-income individuals or the population growth pattern in neighboring, non-expansion states (Alm and Enami 2017).
In contrast, Goodman (2017) cannot isolate any border migration effects for the ACA Medicaid expansion in 2014. The study assesses border migration by restricting its sample to border regions only. It analyzes commuting zones that straddle expansion/non-expansion state borders, respectively, Public Use Microdata Areas (PUMAs) with a population-weighted centroid within a certain distance from these borders (75, 150, and 250 km). Potentially Medicaid-eligible individuals from these border regions are not significantly more likely to migrate from a non-expansion to an expansion state than before the reform (Goodman 2017). However, small border migration effects cannot be ruled out due to large confidence intervals (Goodman 2017).
Goodman’s (2017) approach appears the most intuitive one to study the particular effects of border migration. However, it substantially decreases the number of available observations, resulting in statistical power issues and rendering the identification of border migration effects difficult even though they might exist. Therefore, another approach is needed to identify potential migration effects of the Medicaid expansion. Using the border-versus-interior-regions approach, Alm and Enami (2017) were able to isolate a border migration effect for a Medicaid expansion by comparing border to interior regions.Footnote 1
Consequently, the present paper employs the approach of Alm and Enami (2017) and McKinnish (2005, 2007) and applies it to the ACA Medicaid expansion to gain a more precise picture of the latter’s border migration effects. The approach will be adapted to the present case by using individual-level migration data with a more precise identification of the affected subpopulation, employing PUMAs to delimit regions, and studying five expansion states at once. The present paper follows otherwise closely Goodman’s (2017) overall study set-up. This includes the data source (IPUMS USA ACS), individual-level data, subsample, and most control variables.
The present study also assesses whether the diverging results of Goodman (2017) and Alm and Enami (2017) are due to the considered states or the employed methodology. If the present study obtained statistically significant results, the technique used to study Medicaid border migration would matter. If the obtained results were not significant, there would be something special about the Massachusetts reform or about studying cities as opposed to PUMAs.
Furthermore, the present study extends until 2017, adding three more years to Goodman’s (2017) observation period. This allows pooling years, increasing the number of observations and smoothing yearly fluctuations in the migration rate. Besides, this permits studying slightly longer-term migration effects of the Medicaid expansion. Migration effects might not be visible until 2015 due to increasing public awareness about Medicaid differences across states (Baker 2020; Goodman 2017; Kumar 2021).
3 The Medicaid expansion of the ACA, data sources and study unit
The ACA is a health insurance reform passed in March 2010. Its Medicaid expansion was implemented for the first time on January 1, 2014. The ACA aims at increasing health insurance coverage as previously approximately one-fifth of the non-elderly population was uninsured (Duggan et al. 2019). It includes several provisions, including expanding the public health insurance program Medicaid to previously ineligible parts of the population. This concerns working-age, non-disabled adults with a gross income of their Health Insurance Unit (approximately a family) equal to or below 138% of the federal poverty (guide)line (FPL) (Leung and Mas 2016). The ACA’s further measures include health insurance subsidies to those with slightly higher income levels (between 100% and 400% of the FPL), private health insurance market reforms, and penalties on individuals without insurance (Duggan et al. 2019). Before the reform, working-age, non-disabled adults could either obtain health insurance through their employers (though not all offered it) or conclude insurance themselves (relatively expansive and given no severe pre-existing conditions) (Leung and Mas 2016). In Medicaid non-expansion states, adults below the FPL are not eligible for any health insurance aid, thus potentially without coverage. Those between 100 and 138% of the FPL can resort to subsidies, which are less advantageous for the individual than Medicaid (Goodman 2017; Leung and Mas 2016).
This paper focuses on the Medicaid expansion effects as this sub-program has an explicit cutoff and beneficiary group. It has been implemented uniformly across all states that chose to expand. The Medicaid expansion is a means-tested program and involves no cost-sharing for the beneficiary as the health insurance premiums are essentially equal to zero (Duggan et al. 2019). There is no blocking period for Medicaid. If one moves to another state, a new application is needed, but no minimum residency is required (Stringfellow 2017).
Initially, an expansion of Medicaid for all US states was intended. However, the Supreme Court ruled in 2012 that states may choose whether to expand Medicaid or not (Goodman 2017). A considerable number of states then decided not to expand Medicaid. Some states already had state-level provisions expanding Medicaid before the ACA, which were converted into the ACA Medicaid program. In the expansion states, the federal government fully finances the Medicaid expansion from 2014 until 2016. Afterward, federal funding gradually declines. From 2020 onward, the federal government covers 90% of the Medicaid expansion and the respective state the rest (Goodman 2017).
The expansion and non-expansion states are geographically dispersed (see Fig. 1). To give an overview of the Medicaid expansion status:
-
10 states (including the District of Columbia) had already expansions in place before 2014,
-
16 states expanded in January 2014,
-
7 states expanded later (2014–2016), and
-
18 states have not expanded until the end of 2017 (Black et al. 2019; The Henry J. Kaiser Family Foundation 2019) (see the online resource table I for a complete list of states).
Map of US States by Expansion Status. Expansion status is assigned after Black et al. (2019) and The Henry J. Kaiser Family Foundation (2019). The present paper can ultimately only analyze five expansion states: Arkansas, Illinois, Iowa, Maryland, and New Mexico. For der underlying reasons, see the main text
The present paper uses individual-level ACS data retrieved from IPUMS USA (Ruggles et al. 2020). The ACS is a survey of a 1% sample of the US population. It is representative of any place with a population larger than 65,000 (US Census Bureau 2018). This data source provides yearly data and information on migration over the previous year. It is not possible to track individuals across years due to confidentiality protection.
The ACS provides data on health insurance. This data includes whether the individual in question is below the Medicaid eligibility threshold, is covered by Medicaid, and whether she has any health insurance coverage. The ACS further supplies a wide range of socioeconomic variables such as age, sex, race, income, marital status, family size, and educational attainment.
The studied subsample includes only individuals potentially eligible for the Medicaid expansion: income below or equal to 138% FPL, and between 18 and 64 years of age. One eligible individual per Health Insurance Unit was selected randomly to reduce the design factor.
The smallest identifiable geographic unit in the data are PUMAs. A PUMA is a statistical entity consisting of one or more counties or census tracts combining a population of at least 100,000 (IPUMS-USA n.d.). If a county has less than 100,000 inhabitants, it is merged with another county to create a PUMA. If an area has more than 200,000 inhabitants, it is split (IPUMS-USA n.d.). No PUMA crosses state boundaries. Between 2011 and 2012, the PUMA delineations changed to ensure further compliance with the PUMA definition cited above (IPUMS-USA n.d.). This study uses only the newer PUMA delineation to ensure consistency and covers the period 2012–2017.
Medicaid-induced migration might have occurred in the studied subgroup before 2012 only due to single states passing state-level Medicaid expansion laws. The ACA Medicaid expansion was thought to cover all states uniformly before the Supreme Court ruling in June 2012. Thus, any anticipatory migration effects related to the ACA should only start in the second half of 2012 and ultimately in 2013. Data from 2013 might already have a partial treatment effect included (Goodman 2017). However, the mean and median ACS interviews are conducted in June of the considered year (Goodman 2017). Interviewees were always asked whether they moved within the last 12 months. Thus, 2014 interviews will pick up several moves that happened during 2013.
States are classified into non-expansion, expansion, late-expansion, and early- (pre-ACA- ) expansion states, as shown in Fig. 1. This study focuses on the migration effects in expansion states. A border region in this study is a PUMA whose population-weighted centroid is less than 40 km away from the state border. This threshold is based on the work on welfare migration by McKinnish (2005, 2007), which uses the same threshold.
The treatment PUMAs of interest are the border PUMAs in an expansion state that border a non-expansion state. PUMAs bordering a late- or an early-expansion state might have distinct migration effects.Footnote 2 Therefore, they are excluded from the analysis sample. It is also possible that a PUMA borders two different states with different expansion statuses. If this involves a late- or early-expansion state, the PUMA is excluded from the analysis sample to avoid diluting the estimated migration effect. PUMAs bordering another expansion state should not experience any change in migration due to no Medicaid-related incentives to migrate. They are part of the control group together with the interior PUMAs. In sum, the following classification scheme has been applied to the PUMAs:
-
bordering a late-expansion state: excluded from the analysis sample,
-
bordering an early-expansion state: excluded from the analysis sample,
-
bordering a non-expansion state, while not falling in the two categories above: treatment group (referred to hereafter as treated border regions),
-
bordering only another expansion state: control group (control regions), and
-
not bordering any state: control group (control regions).
Half of the sixteen expansion states do not have any treated border regions and are excluded ex-ante from the analysisFootnote 3. The retained eight expansion states at this stage are Arkansas, Illinois, Iowa, Kentucky, Maryland, New Mexico, Washington, and West Virginia. Maps in the online resource show treatment and control regions.
4 Empirical strategy
This paper investigates whether the treated border regions of expansion states attract more in-migrants after the ACA compared to both their pre-ACA migration rates and the migration evolution in these states’ interior regions. Empirically, this is studied in a difference-in-difference framework. The first difference in this framework is between pre-and post-ACA years. The second difference is between treatment and control regions in expansion states. The interaction of these two differences then captures the effect of the ACA Medicaid expansion on migration.Footnote 4
More precisely, the estimated model is the following:
where yirst is a dummy taking the value of one if an individual i residing in region r of state s at time t has migrated across any state border but within the US in the past 12 months before the interview in the considered year. Otherwise, the dummy takes the value of zero. Migrants from outside the US are dropped from the dataset. Thus, the dummy captures in-migration in the past year.Footnote 5postt is a dummy taking the value of one for post-reform (treatment) years (2014–2017) and zero otherwise (2012 and 2013). borderr is the treatment region dummy, taking the value of one if an individual resides in a treated border PUMA as defined above. Otherwise, the dummy takes the value of zero. The dummy is coded as a missing value for individuals residing in PUMAs bordering late- or early-expansion states. borderr * postt is the interaction term of the border and post dummies. Its coefficient δ captures the treatment effect of the ACA Medicaid expansion on migration. δ is expected to be positive.
Xit is a vector of individual-level control variables detailed below. µs are state fixed effects (FEs), which are included when pooling several states together. εirst is the error term.
The difference-in-difference framework already captures a lot of variation between entities, especially those due to specific years (for instance, federal reforms or national economic downturns) or locations (treatment versus control regions, urban versus rural). It also captures baseline migration levels, which occur due to various other reasons than the studied Medicaid expansion (job, education, natural amenities, family ties, other public services). The difference-in-difference framework captures migration due to higher wage or lower price levels in certain regions if the respective differences in wages and prices are constant over time.Footnote 6 Besides, the state FEs capture state-specific, time-invariant characteristics when several states are pooled together.
Control variables for age, sex, race, income, marital status, family size, and educational attainment have been added as these factors all influence migration decisions (Foster 2017; Molloy et al. 2011; Rosenbloom and Sundstrom 2004). Including control variables improves precision by avoiding omitted variable bias and mitigating any effects of changes in the sample composition over time (Goodman 2017).
This difference-in-difference framework can be expanded to a triple difference one by additionally comparing migration by higher-income individuals (between 200 and 400% FPL) to migration by Medicaid-eligible ones. As the Medicaid expansion is almost exclusively financed by the federal government, the Medicaid expansion should not affect middle- and high-income individuals via state taxes, hence not resulting in any migration incentive. The triple difference set-up additionally controls for state-specific migration shocks unrelated to the Medicaid expansion. It requires adding a dummy for Medicaid eligibility and further interaction terms. The triple interaction term of Medicaid eligibility, treatment region, and post-ACA period now captures the treatment effect.
The corresponding regression equation is:
Both frameworks require a linear probability model as the dependent variable in the regressions is binary. Both ordinary least squares (OLS) and logistic models are estimated. The calculated standard errors are robust and clustered at the state level when the regression includes several states.
Some prerequisites need to be fulfilled to estimate a valid difference-in-difference model. For instance, no self-selection into the treatment group should occur that might influence the estimated migration effect. Living in a treated border region previous to the ACA reform can be considered reasonably exogenous to the individual.Footnote 7
Individuals might also self-select into eligibility for Medicaid by reducing their income to fall below the eligibility threshold. However, the literature can only identify tiny, if any, changes in labor supply after the ACA Medicaid expansion (Gangopadhyaya and Garrett 2020; Gruber and Sommers 2019; Kaestner et al. 2017). This renders it unlikely that a substantial number of individuals reduced their working hours, hence their income, to be eligible for Medicaid. However, a sample-selection effect due to income differences across regions is conceivable. An individual who lived in a high-income region 12 months before the ACS interview would be more likely to be in the selected sample if she migrated to a low-income region with fewer absolute earning opportunities. Conversely, an individual would forego her Medicaid eligibility if her income rises above the eligibility threshold after migrating to a higher-income destination. In the latter case, the Medicaid-related incentive to migrate would be reduced. Both channels result in an upward bias of the estimated migration flow to a low-income region. However, there is no correlation between being a treated border region and having a lower average income.
The parallel trend assumption has also to hold to estimate the ACA Medicaid expansion’s causal effect on migration. The in-migration rates to treated border and control regions should exhibit parallel trends before the expansion. There should neither be any third factor inducing differences between the treatment and control group concurrently with the reform. However, no major reform with a similar geographic distribution is happening simultaneously as the ACA.
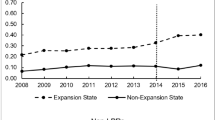
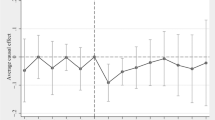
Parallel trend tests have been conducted using data for 2008–2011 and the old PUMA delineations.Footnote 8 Difference-in-difference and triple difference event study regressions have been estimated to this effect. The overall set-up is similar to the main regressions’ one, but now several year dummies and interaction terms are included: one for each year over 2008–2010, 2011 being the reference year. In the case of parallel trends, there should not be any time-varying differences in migration rates between the treatment and the control group relative to the 2011 difference in migration rates, conditional on the control variables. The treatment effect coefficients for all years are thus expected not to be statistically significant. This is almost always the case for the expansion states (see online resource table III for Arkansas and Maryland; results for the other states available upon request).
Tests of joint significance have been conducted for all treatment effect coefficients together. In the case of parallel trends, the tests should not reject the null hypothesis of the treatment effect coefficients being jointly equal to zero (respectively equal to one for the odds ratios of logistic regressions). The p-values should hence be high, at least > 0.5. If these tests favor parallel trends in migration over 2008–2011, this suggests parallel trends up until the ACA.
The obtained p-values vary considerably across states (Table 1), indicating differing parallelism strengths in pre-reform migration rate trends. In the difference-in-difference set-up, only Arkansas and Maryland have p-values above 0.5. In the triple difference regressions, this is the case again for Maryland as well as for Illinois, Iowa, and New Mexico.Footnote 9 Therefore, the present study only examines regressions results for these five states.
5 The Medicaid expansion migration effect
This paper hypothesizes that the Medicaid expansion increases in-migration rates of treated border regions compared to their pre-expansion levels and control regions’ migration rate evolution. Thus, the treatment effect coefficient is expected to be positive.
Tables 2 and 3 report the difference-in-difference (columns 1 and 2) and triple difference (columns 3–7) results for the expansion states with treated border regions and satisfactory parallel trend test results. The states are presented in decreasing order of their parallel trend tests’ p-values. Summary statistics for Arkansas and Maryland can be found in the online resource table IV.
In the difference-in-difference regressions, both Arkansas and Maryland have, as expected, a positive treatment effect coefficient of Medicaid-expansion-induced migration. However, it is only statistically significant at the 5% level for Arkansas. For the latter, the probability of having migrated to its treated border regions increases by 1.3 percentage points following the ACA compared to before and control regions according to the OLS regression. The baseline migration rate in these regions was 5.5% in 2012. According to the logistic regression, the odds of having migrated are 48% higher for individuals living in these regions after the ACA compared to before and control regions. The post coefficients are not statistically significant in these regressions, indicating that overall migration has not increased in the post-ACA years (2014–2017). The border coefficient is only statistically significant and positive for Arkansas, indicating that migration to Arkansas’ treated border regions has always been higher than to its interior ones. No such effect is discernable for Maryland.Footnote 10
A back-of-the-envelope calculation for Arkansas shows that the additional number of Medicaid beneficiaries due to induced migration is inconsequential from a regional-level perspective. In 2012, 14,499 low-income individuals migrated interstate to treated border regions in Arkansas, while 251,534 lived there already, resulting in a migration rate of 5.5%. The Medicaid-induced migration rate increase by 1.3 percentage points amounts to 3853 additional migrants. This increases the number of Medicaid-eligible working-age adults in treated border regions by 1.5%. The total number of “native” Medicaid beneficiaries in these regions in 2015 equals 92,658. If all additional migrants take up Medicaid, the number of Medicaid beneficiaries increases by less than 4.2%. The corresponding state-level shares are even smaller. Thus, the number of additional migrants due to the Medicaid expansion is statistically significant for Arkansas but is presumably not relevant size-wise for policymakers at the regional and state level.Footnote 11
The difference-in-difference framework can be turned into a triple difference one by adding observations for higher-income, non-Medicaid eligible individuals as comparison group. Columns 3–6 report the results by state. The treatment effect’s coefficient is now only statistically significant at the 10% level for Iowa in the OLS regression, while it is insignificant in all the other cases. The coefficient even turns negative for Maryland (OLS) and New Mexico (OLS and logistic).
Column 7 of each table presents results for grouping the four considered states (Maryland, New Mexico, Iowa, and Illinois) together. These regressions include state FEs to control for time-invariant state characteristics and cluster standard errors at the state level. Pooling several states together can improve statistical precision by increasing the number of observations available relative to the number of included regressors. It also smooths out the migration rate fluctuations, further increasing the estimations’ precision. The treatment effect coefficient is positive in the state group regressions. However, it is still not statistically significant at the 10% level despite the standard errors being smaller than in the single-state regressions.
The post coefficients are not statistically significant in all triple difference regressions, indicating that overall migration has not increased in the post-ACA years (2014–2017). The border coefficient is only statistically significant at the 10% level and positive for Iowa, indicating that migration to Iowa’s treated border regions has always been higher than to its interior ones. No such effect is discernable for the other states. The Medicaid dummy’s coefficients are always positive and, in most cases, statistically significant at the 5% level. This result indicates that Medicaid-eligible individuals are generally more likely to migrate ceteris paribus than slightly higher-income individuals. This fact might be due to this group also including students who have low incomes but migrate relatively frequently across states for and after college. Furthermore, this effect is offset by the negative coefficients for the interaction terms of Medicaid eligibility with respectively border and post. The coefficient of the interaction of border and post is not statistically significant in these regressions, except for New Mexico (positive).
Overall, the obtained results do not allow for a straightforward interpretation. Some states do not exhibit a Medicaid migration effect, while others have a statistically significant effect or a tendency towards it. The following section discusses more in detail possible reasons for these diverging results. However, even if a statistically significant migration effect occurs, the absolute number of additional migrants is so small in the aggregate that it seems manageable at the regional and state level. Thus, Medicaid migrants do not appear to impose a meaningful fiscal externality on these budgets. Excessively attracting low-income individuals due to the Medicaid expansion is unlikely.
The obtained results mostly correspond to Goodman’s (2017) insignificant and imprecise ones. The positive, but small in aggregate size, migration effect for Arkansas aligns with Alm and Enami (2017) and the empirical welfare migration literature (Gelbach 2004). However, its border migration effect is not as clear-cut as in McKinnish (2005, 2007) and Alm and Enami (2017).
6 Discussion
Statistical power issues might be partly responsible for the mostly statistically insignificant results, visible in the large standard errors. These issues might be due to several reasons.
First, the number of migrant observations for a single state is relatively small in the considered low-income sample. Arkansas has the most migrant observations in treated border regions of any analyzed state. Still, it has only about 150 migrant observations in treated border regions per year, although almost half of Arkansas’ regions are treated border ones (online resource table V). Note that this number is not proportional to the total number of migrants in these regions due to the applied weights in the ACS (duly considered in the regressions). Furthermore, this number includes all interstate migrants, also those migrating for other reasons than Medicaid. At the extreme, Maryland has only 48 migrant observations in treated border regions across the whole study period. This number still fulfills the rule of thumb of a minimum of 10 cases for a regression analysis but is far from ideal, potentially leading to Maryland’s statistically insignificant treatment effect and border dummy coefficients.
Second, the relatively small number of migrants also leads to random fluctuations in the annual migration rates, which are only incompletely smoothed by pooling the years together. Thus, the migration rate is volatile in these regions as individual decisions matter more for the observed migration rate in small samples. This volatility increases the noise in the regressions. The very low R2 and Pseudo‑R2 of the regressions (at the most 0.04 and 0.14 respectively) illustrate the difficulties of explaining migration decisions even with control variables included. Why one individual migrates and another not remains to a high degree unpredictable as many unobservables influence this decision. Again, this effect would be particularly strong for Maryland with its few migrant observations.
Third, logistic regressions might be particularly prone to small sample bias as they are based on the Maximum Likelihood approach. OLS regressions have their own issues in the linear probability case, especially when the mean of the dependent variable is close to 0 or 1, as in the present case with a migration probability below 6%. These shortcomings aggravate the discussed identification issues.
Fourth, it is more difficult to identify a treatment effect in difference-in-difference regressions if the considered groups are very different in size. The larger the difference in the respective group sizes, the stronger the treatment effect must be to be detectable. For instance, Maryland has only one treated border PUMA, constituting 10% of all included observations. In contrast, the ratio is almost 50:50 for Arkansas, hence much more well-balanced. The absolute number of observations in all subgroups is also higher in Arkansas. Thus, it is easier to identify a treatment effect for Arkansas than for Maryland, given that one exists. The Maryland case appears also underpowered according to the standard formula for the minimum detectable effect. Furthermore, the border-versus-interior-regions approach underestimates the migration effect by ignoring migration to interior regions, exacerbating this issue.
Statistical power issues are not the only explanation for statistically insignificant results. It might also be that simply no migration effect exists in Maryland. Maryland’s estimated treatment effect coefficients are smaller than the Arkansas ones. Furthermore, New Mexico and Illinois also exhibit insignificant treatment effect coefficients while they are only once marginally significant for Iowa. An inexistent Medicaid migration response would not necessarily imply that the concerned individuals do not value Medicaid. The involved migration costs might be too high and the obtained benefits too uncertain for the considered low-income group (Finkelstein et al. 2019; Goodman 2017). Information deficits about the program and one’s eligibility in another state, as well as hopes for future expansions in one’s state of residence, might also play a role (Baker 2020; Goodman 2017).
Arkansas’ Medicaid migration effect might constitute a peculiarity, maybe due to unobserved regional conditions, or be spurious. Differences across states in advertising the Medicaid expansion might lead to differing migration effects (Baker 2020). Third factors, such as the presence of children, youth, Medicaid insurance status, immigration, commuting, or the PUMA-level unemployment rate, cannot explain the differing results across states. Their inclusion into the regression does not affect the estimated migration effects (cf. robustness check subsection 7.2).
Having said that, Arkansas’s migration effect is strong and robust, rendering it impossible to neglect it and rule out any migration effects altogether. Although statistically insignificant, Iowa and Illinois also exhibit positive migration effects of comparable size or even larger. However, even for Arkansas with its strong migration effect, the aggregate absolute number of additional migrants remains small and appears manageable at the regional level.
7 Robustness checks
This section presents the results of several robustness checks. The first subsection considers different border cutoffs than 40 km, while the second discusses regression results for different subsamples. The third subsection examines pseudo-regressions for intrastate migration, while the fourth considers regressions over the whole 2008–2017 period for selected states.
7.1 Different border cutoffs
A border region in this study is a PUMA whose population-weighted centroid is less than 40 km away from the state border. This threshold is based on McKinnish’s (2005, 2007) work on welfare migration. However, Alm and Enami (2017) do not find any migration effect for the Massachusetts Medicaid reform after 25 km. The advantage of a more restrictive border definition is its increased likelihood of picking up border migration, which typically declines with distance. Its disadvantage is the reduced number of observations in treatment regions. Therefore, the main regressions have been repeated with mutually exclusive 10 km border intervals up to 40 km. The results can be found in the online resource tables VI and VII. Only Arkansas has observations for all the four considered distance intervals.
In the difference-in-difference regressions, the treatment effects are always positive. However, they are only statistically significant at the 10% level for Arkansas’ [10, 20] and [20, 30] km intervals. The treatment effect sizes are similar throughout, while the [30, 40] km one is smaller than the others. This pattern indicates a relatively stable migration response up to 30 km from the border, which then might decline. Maryland has only one treated border PUMA, which is in the [30, 40] km range. Its migration effect is hence not statistically significant as in the main regressions.
In the triple difference regressions, only the treatment effect for the [30, 40] km interval is sometimes statistically significant at the 10% level for New Mexico, Iowa, and Illinois. It is positive for the latter two, while negative for New Mexico. This unexpected negative effect might be due to the low number of observations per interval, resulting in PUMA-level migration peculiarities shining through. Maryland has only one treated border PUMA, resulting in a not statistically significant migration effect as in the main regressions.
These oddities disappear when increasing the number of observations per distance interval by pooling all the four states together. Only the [10, 20] km interval’s treatment effect is statistically significant at the 5% level and positive. Thus, the Medicaid migration effect tends to be stronger closer to the border if it occurs. All the remaining treatment effects are positive, albeit not statistically significant, with varying sizes. The migration effect does not linearly decline with distance. However, this might be due to the low number of migrant observations per distance category.Footnote 12
The present study sometimes finds migration effects beyond Alm and Enami’s (2017) 25 km cutoff, but at the latest, the effect seems to disappear after McKinnish’s (2005, 2007) 40 km threshold. The cutoff distance is distinctively smaller than the 75, 150, and 250 km thresholds used in Goodman (2017). However, the gradually declining border migration effect found for Massachusetts by Alm and Enami (2017) could not be confirmed. This effect might be either a specificity of Massachusetts or due to them studying cities, which are area-wise more concentrated than PUMAs. Identifying individuals living close to a treatment border remains imprecise as the PUMAs are pretty large in area, especially in rural areas. Furthermore, the here-obtained results need to be considered with caution due to the low number of migrant observations available. Thus, they do not allow an ultimate answer to the here considered question.
7.2 Subsamples
This subsection presents the results of several regressions, where the sample changes: urban/rural distinction, childless subsample, youth subsample, border regions to late- and early-expansion states, and non-expansion states.
The migration response to the Medicaid expansion might differ in urban and rural areas, which the difference-in-difference framework would not capture. Notably, it might be that if individuals decide to move for Medicaid, they rather move to urban areas than rural ones. For instance, Kumar (2021) could only identify an ACA migration effect for homeless individuals for metropolitan border counties but not for rural ones. Therefore, this robustness check includes a dummy variable and interaction terms for urban status. Restricting the sample to urban areas is not viable. It reduces the number of treated border regions considerably, further aggravating the issues discussed in the previous section.
The regressions include a dummy variable taking the value of one if an individual currently lives in a PUMA located at least partly in a central city of a metropolitan statistical area as defined by the US Census Bureau. Some regressions also include the respective interaction terms of this dummy. The results can be found in the online resource table VIII for Arkansas (difference-in-difference) and in table IX for the four states pooled together (triple difference; remaining results upon request). The urban dummy’s coefficient is only statistically significant at the 5% level in the triple difference regressions, then being positive. In this case, more individuals migrate to urban areas than rural ones. However, the coefficients of its interaction term with the treated border region dummy and the treatment effect are never statistically significant. Thus, no difference between urban and rural areas regarding Medicaid migration can be identified. Most importantly, the inclusion of the urban dummy and its interaction terms does not affect the estimated migration effect. It remains positive and of almost identical size for Arkansas, albeit the significance level drops to 10%. For the four triple difference states, the treatment effect also remains positive and of comparable size as in the main regressions. It is now statistically significant at the 5% level in the logistic regression while remaining insignificant in the OLS one.Footnote 13
Individuals living in a household with an underage child might be less likely to migrate ceteris paribus. Children do not gain additional coverage with the ACA Medicaid expansion, but they increase one’s migration costs (Goodman 2017). Therefore, a stronger migration effect is expected for childless individuals. On the other hand, the family size control variable might already capture some of this effect. Running the regressions on a restricted subsample of childless individuals does not seem advisable as the sample size is reduced considerably by at least 25%. Therefore, a childless dummy and its interaction terms are included into the regressions: either for being childless altogether or for not having a child under age 18. Regardless of its definition, the childless dummy’s and its interaction terms’ coefficients are never statistically significant at the 10% level. Thus, the estimated migration effect remains as previously (results available upon request).
Young people (aged 19–25) might have benefitted disproportionally from the ACA Medicaid expansion as they historically had the highest uninsurance rates among all age groups (Gangopadhyaya and Johnston 2021). Furthermore, they are generally more likely to migrate, as shown by the age control variables’ statistically significant, negative coefficient. Thus, they might be disproportionally inclined to migrate for Medicaid. Therefore, a youth dummy (below 26 respectively 31 years) and its interaction terms are included into the regressions. Running regressions on a youth subsample is again not viable as the sample size would be more than halved.
In the difference-in-difference regressions, the youth Medicaid migration effect is always positive but never statistically significant at the 5% level, while the main migration effect turns not statistically significant for both considered states. A complex picture emerges in the triple difference regressions. Significance levels and signs vary between OLS and logistic regressions as well as depending on the considered age threshold. However, the main migration effect is never statistically significant, similar to the main regressions. Overall, this hints at the Medicaid migration response possibly being particularly strong among the youth. However, this cannot be evaluated conclusively due to the small size of the youth subsample. (Results are available upon request.).
The main analysis excludes any border regions to late- and early-expansion states. Thus, it also excludes border regions that border at the same time non-expansion and late- or early-expansion states. This exclusion might lead to an incomplete picture of the occurring Medicaid-induced migration. Furthermore, the number of border regions and hence their observations decreases substantially in some states (for instance, by about 70% for Maryland).Footnote 14 Therefore, dummies and interaction terms for border regions neighboring late- and early-expansion states have been added into the regressions. The obtained results mirror the main ones. The estimated migration effects are not statistically significant but mostly positive. Thus, this approach does not change the insignificant results either. (Results are available upon request.).
The ACA Medicaid expansion should as well affect the non-expansion states. In these states, the Medicaid expansion should lead a priori to a decrease in in-migration rates of treated border regions compared to their pre-expansion levels and interior regions’ migration evolution. Thus, the treatment effect coefficient is expected to be negative. No statistically significant treatment effects emerge in difference-in-difference and triple difference regressions (results available upon request). Thus, no ACA Medicaid expansion effect on interstate migration is discernable for non-expansion states, in accordance with Baker (2020).
7.3 Pseudo-regressions for intrastate migration
This subsection presents results of pseudo-regressions with intra-state migration instead of inter-state migration. The intrastate migration should not have been affected by the ACA Medicaid expansion. The pseudo-treatment effect coefficient (post-ACA* border) should not statistically significantly differ from zero.
The dependent variable is replaced in these regressions. The migration dummy now equals one if an individual has migrated across PUMAs but within the state. It is zero if the individual has not migrated or only within the PUMA. The dummy is set to a missing value if the individual has migrated across states or from abroad. Thus, the sample size is slightly reduced (by approximately 3%) compared to the main regressions, while the migration rate is higher (approximately 7.5 vs. 4.7%). The regression set-up remains otherwise the same.
These regressions should fulfill the parallel trend test requirements to infer from them regarding the pseudo-treatment over the 2012–2017 period. Therefore, parallel trend tests over 2008–2011 have been run. However, very few states exhibit parallel trend tests with a p-value > 0.5. For the states considered in the main analysis, this is only the case for New Mexico (triple difference). Furthermore, Kentucky (both regression models) and West Virginia (difference-in-difference) have this kind of parallel trend test result. Therefore, the pseudo-regressions have been run for the mentioned states (online resource table X presents the results for New Mexico; remaining results available upon request).
The pseudo-treatment coefficient is never significant at the 10% level. The t‑test p-values of the pseudo-treatment effect coefficients are often above 0.7. Thus, one can be confident that the observed interstate migration effect originates from the ACA Medicaid expansion if the state exhibits good parallelism in pre-existing trends.
7.4 Regressions over 2008–2017
The PUMA delineation changes between 2011 and 2012 render it impossible to use the 2008–2011 data for the main analysis. However, in Arkansas, Kentucky, New Mexico, and Washington, the PUMA delineations did not change or only in such a way as not to affect the borders of the overall treatment and control regions, which might consist of several PUMAs. It is hence possible for these four states to combine the 2008–2011 with the 2012–2017 data.
First, the parallel trend tests have been repeated over the whole pre-period 2008–2013. The obtained results are very similar to the 2008–2011 ones. The p-values of the F‑ respectively X2- tests of joint significance of all the treatment effect coefficients of the event study regression are again only convincing for Arkansas in the difference-in-difference setting (> 0.7, triple difference < 0.4) and for New Mexico in the triple difference one (> 0.5, difference-in-difference < 0.2). Kentucky (< 0.3 respectively < 0.1) and Washington (< 0.2) continue to exhibit unsatisfactory parallel trend test results. These results confirm the 2008–2011 ones, indicating that they are a good proxy test for parallel trends in migration before the ACA.
Second, the longer pre-period renders it possible to run pseudo-regressions mirroring the set-up of the main ones: two pre- and four treatment years. 2008 and 2009 are now the pseudo-pre-treatment, while 2010–2013 are the pseudo-treatment years. As no reform occurred, the coefficient of the pseudo-treatment effect should not be statistically significant. This is the case for all four states. Thus, the statistically significant results obtained in the main regressions for Arkansas have not been there before but are particular to the post-ACA years.
Third, it is now possible to estimate regressions with a six-year pre-treatment period (2008–2013) for Arkansas and New Mexico (online resource table XI). The results resemble the main ones for both states. Arkansas again exhibits a statistically significant and positive migration effect, while New Mexico’s is not statistically significantly negative.
8 Conclusion
This paper studies the 2014 ACA Medicaid expansion’s migration effects, especially for border regions in expansion states bordering a non-expansion state. It compares these border with interior regions’ in-migration before and after the ACA in difference-in-difference and triple difference frameworks to assess the border migration effects. Treated border regions of expansion states are expected to attract more migrants after the ACA compared to both their pre-ACA migration rates and the migration evolution in these states’ interior regions.
The present paper’s contribution is the combination of Goodman’s (2017) analysis of the ACA Medicaid expansion with the border-versus-interior-regions approach by Alm and Enami (2017) to evaluate migration induced by a Medicaid expansion. Additionally, the present study extends up until 2017. This allows for both pooling years and studying slightly longer-term effects of the ACA Medicaid expansion on migration.
The paper could not identify border migration effects for most considered states, but Arkansas exhibits a statistically significant effect. Even for Arkansas, however, the aggregate number of additional migrants is so small that it seems manageable at the regional and state level. Thus, Medicaid migrants do not appear to impose a meaningful fiscal externality on these budgets. Excessively attracting low-income individuals due to the Medicaid expansion is unlikely even if the migration effect is statistically significant for the considered state.
Employing the border-versus-interior-regions approach and pooling several years can help identify border migration effects that otherwise could not be isolated. However, this approach is not enough when a state has few treated border regions and a low number of migrant observations. In these cases, the statistical power issues of previous studies resurface, rendering the identification of a Medicaid migration effect impossible. Therefore, the latter’s existence, precise size, and differences across states remain an unsolved puzzle requiring further research.
Notes
Alm and Enami (2017) can probably identify a border migration effect because of the larger amount of usable data per state with the border-versus-interior-regions approach. Even though the size of the treatment group remains the same, this approach allows for a more precise estimation of the control variables’ effect on the probability of migrating, leading to a better isolation of the Medicaid migration effect.
Expansion-state PUMAs bordering a late-expansion state should experience some Medicaid-induced in-migration in the early years until it became clear that the neighboring state will also expand. PUMAs bordering an early-expansion state might experience some in-migration by individuals, who migrated to the neighboring state to obtain Medicaid and now return back. However, this migration effect should be smaller than the original Medicaid-expansion one as migration is costly and many individuals probably do not return.
New Jersey, Ohio, and Rhode Island do not border any non-expansion states. The population-weighted centroids of PUMAs bordering non-expansion states in Arizona, Colorado, Nevada, North Dakota, and Oregon are more than 40 km away from the border. The PUMAs there are very rural and hence very large.
The present study hypothesizes that the migration induced by the Medicaid expansion is predominantly a border regions’ one. Almost no state-level migration effects can be identified for Medicaid-expansion migration between expansion and non-expansion states for the present analysis sample (see online resource table II). This is in line with former studies (Alm and Enami 2017; Goodman 2017; Schwartz and Sommers 2014). Thus, the migration flows to interior regions appear to be negligible and are hence neglected in the present setup in favor of estimating a differential effect.
If only migrants from neighboring non-expansion states are considered, the number of migrants drops so low for single states that no meaningful regression analysis can be run. Thus, this analysis retorts to the broader migration definition presented above. Even if the migrants’ origin is not controlled for, they are still more likely to migrate to border regions ceteris paribus as all the other differences in potential pull-factors are controlled for by the difference-in-difference nature of the framework. This would not be the case if Medicaid migrants more than proportionally favored cities compared to other migrants. However, no evidence can be found for this (see robustness check subsection 7.2). Instead, a slight advantage of border regions still remains due to being close for migrants originating from the other side’s border regions.
Regional business cycle fluctuations might result in time-varying differences in income opportunities, which would pose a threat to identification. However, no effect of PUMA-level employment rates on migration and the obtained results can be identified (results available upon request).
The Medicaid expansion of the neighboring state as well as the non-expansion of one’s own state of residence might be unsurprising given the respective states’ track record on public programs. Thus, residents of a state with a poor track record are less likely to out-migrate to obtain Medicaid as they have chosen to reside in a non-generous state in the first place. This kind of self-selection would lead to an underestimation of the Medicaid-induced migration flow. Any obtained estimate can be considered a lower bound in this sense. Nevertheless, no evidence can be found that surprising (non-) expansion states experience larger in-(out-) migration after the ACA.
Data on compliance with the Medicaid eligibility threshold is available from 2008 onward only. One cannot use the main data from 2012 and 2013 for the parallel trend tests as the PUMA delineations change between 2011 and 2012. Only four of the eight expansion states with treated border regions exhibit PUMA delineations that did not change or only in such a way as to not overly affect the borders of the treatment and control regions (Arkansas, Kentucky, New Mexico, Washington). For these four states, parallel trend tests over 2008–2013 have also been run. Their results are very similar to the here presented ones (see robustness check subsection 7.4 and the online resource maps).
Adding further control variables such as PUMA-level employment rates or time trends does not improve the parallel trend test results. Implementing more advanced econometric techniques such as synthetic control groups or state-level pre-treatment trends (Willage 2020) is not possible due to the regional definitions and limited data. Thus, the proposed regression framework appears the best possible given the available data and the research question at hand.
This insignificant effect might be due to Maryland only having one treated border PUMA, potentially leading to its insignificant border and treatment effects at the same time (discussed more in detail in section 6). However, one cannot conclude per se that an (in)significant border coefficient implies an (in)significant treatment effect as the dummy’s task is to control for pre-existing differences in migration trends across the regions so that they do not interfere with the treatment effect.
If the migrants are sicker than the average “native” Medicaid-eligible population this would result in disproportionate costs for their future Medicaid coverage and other social assistance. However, no evidence for sicker individuals (i.e. self-reported disabled or older) being more likely to migrate can be found: neither in general nor following the ACA Medicaid expansion. To the contrary, sicker individuals are significantly less likely to migrate for Medicaid than healthy individuals. This is in line with Goodman’s (2017) results and probably due to migrating being more costly and cumbersome, if not impossible, if you are sicker. Furthermore, some disabled individuals were already covered by Medicaid previous to the ACA.
The main regressions have been repeated with respectively a 10 and 20 km threshold. In these cases, no statistically significant migration effect can be identified. When instead all other border regions up until a threshold of 40 km are excluded, the 10 and 20 km regions exhibit sometimes a statistically significant positive migration effect. This is in line with the interval results and probably due to some migration effect remaining between 20 and 40 km. If one does not exclude these regions, they are part of the control group and meddle the migration effect. (Results are available upon request.).
If using other urban definitions such as the OECD threshold of inhabitants per square km or being in a metropolitan statistical area at all, the urban dummies and their interaction terms never exhibit statistically significant coefficients. Consequently, the estimated migration effect remains unaffected.
In contrast, this effect is irrelevant for Arkansas. Arkansas has no border PUMAs to late- or early-expansion states.
References
Alm J, Enami A (2017) Do government subsidies to low-income individuals affect interstate migration? Evidence from the Massachusetts Health Care Reform. Reg Sci Urban Econ 66:119–131. https://doi.org/10.1016/j.regsciurbeco.2017.06.005
Armenter R, Ortega F (2010) Credible redistributive policies and migration across U.S. states. Rev Econ Dyn 13(2):403–423. https://doi.org/10.1016/j.red.2010.02.001
Bailey MA (2005) Welfare and the multifaceted decision to move. Am Polit Sci Rev 99(1):125–135. https://doi.org/10.1017/S0003055405051531
Bailey MA, Rom MC (2004) A wider race? Interstate competition across health and welfare programs. J Polit 66(2):326–347. https://doi.org/10.1111/j.1468-2508.2004.00154.x
Baker MC (2020) Three essays in health economics. Dissertation, George Mason University
Black B, Hollingsworth A, Nunes L, Simon K (2019) The effect of health insurance on mortality: Power analysis and what we can learn from the Affordable Care Act coverage expansions. Working Paper, vol 25568. National Bureau of Economic Research, https://doi.org/10.3386/w25568
Borjas GJ (1999) Immigration and welfare magnets. J Labor Econ 17(4):607–637. https://doi.org/10.1086/209933
Brown CC, Oates WE (1987) Assistance to the poor in a federal system. J Public Econ 32(3):307–330. https://doi.org/10.1016/0047-2727(87)90035-1
Brueckner JK (2000) Welfare reform and the race to the bottom: Theory and evidence. South Econ J 66(3):505–525. https://doi.org/10.2307/1061423
Cebula RJ, Clark JR (2013) An extension of the Tiebout hypothesis of voting with one’s feet: The Medicaid magnet hypothesis. Appl Econ 45(32):4575–4583. https://doi.org/10.1080/00036846.2013.795278
De Jong GF, Graefe DR, Pierre StT (2005) Welfare reform and interstate migration of poor families. Demography 42(3):469–496. https://doi.org/10.1007/BF03214592
Duggan M, Goda GS, Jackson E (2019) The effects of the Affordable Care Act on health insurance coverage and labor market outcomes. Natl Tax J 72(2):261–322. https://doi.org/10.17310/ntj.2019.2.01
Finkelstein A, Hendren N, Luttmer EFP (2019) The value of Medicaid: Interpreting results from the Oregon health insurance experiment. J Polit Econ 127(6):2836–2874. https://doi.org/10.1086/702238
Foster TB (2017) Decomposing American immobility: Compositional and rate components of interstate, intrastate, and intracounty migration and mobility decline. DemRes 37:1515–1548. https://doi.org/10.4054/DemRes.2017.37.47
Gangopadhyaya A, Garrett B (2020) How workers fared under the ACA. J Health Polit Policy Law 45(5):863–887. https://doi.org/10.1215/03616878-8543322
Gangopadhyaya A, Johnston EM (2021) Impacts of the ACA’s Medicaid expansion on health insurance coverage and health care access among young adults [Research Report]. Urban Institute. https://www.urban.org/sites/default/files/publication/103673/impacts-of-the-acas-medicaid-expansion-on-health-insurance-coverage-and-health-care-access-among-young-adults_0.pdf. Accessed 13 Dec 2021
Gelbach JB (2004) Migration, the life cycle, and State benefits: How low is the bottom? J Polit Econ 112(5):1091–1130. https://doi.org/10.1086/422560
Goodman L (2017) The effect of the Affordable Care Act Medicaid expansion on migration. J Policy Analysis Manag 36(1):211–238. https://doi.org/10.1002/pam.21952
Greenwood MJ (1997) Internal migration in developed countries. In: Rosenzweig MR, Stark O (eds) Handbook of population and family economics, vol 1. Elsevier, Amsterdam, pp 647–720 https://doi.org/10.1016/S1574-003X(97)80004-9
Gruber J, Sommers BD (2019) The affordable care act’s effects on patients, providers, and the economy: what we’ve learned so far. J Policy Anal Manage 38(4):1028–1052. https://doi.org/10.1002/pam.22158
IPUMS-USA (n. d.) IPUMS-USA: descr: PUMA. https://usa.ipums.org/usa-action/variables/PUMA#description_section. Accessed 13 Dec 2021
Kaestner R, Garrett B, Chen J, Gangopadhyaya A, Fleming C (2017) Effects of ACA Medicaid expansions on health insurance coverage and labor supply. J Policy Anal Manage 36(3):608–642. https://doi.org/10.1002/pam.21993
Kennan J, Walker JR (2010) Wages, welfare benefits and migration. J Econom 156(1):229–238. https://doi.org/10.1016/j.jeconom.2009.09.019
Kennan J, Walker JR (2013) Modeling individual migration decisions. In: Constant AF, Zimmermann KF (eds) International handbook on the economics of migration. Edward Elgar, Cheltenham, pp 39–54 https://doi.org/10.4337/9781782546078
Kumar A (2021) Moving to better healthcare? Estimating the causal impact of Medicaid expansion on homeless individuals. School of Economic Sciences Washington State University,
Leung P, Mas A (2016) Employment effects of the ACA Medicaid expansions. Working Paper, vol w22540. National Bureau of Economic Research, https://doi.org/10.3386/w22540
McKinnish T (2005) Importing the poor: Welfare magnetism and cross-border welfare migration. J Hum Resour XL(1):57–76. https://doi.org/10.3368/jhr.XL.1.57
McKinnish T (2007) Welfare-induced migration at state borders: New evidence from micro-data. J Public Econ 91(3):437–450. https://doi.org/10.1016/j.jpubeco.2006.09.002
Molloy R, Smith CL, Wozniak A (2011) Internal migration in the United States. J Econ Perspect 25(3):173–196. https://doi.org/10.1257/jep.25.3.173
Rosenbloom JL, Sundstrom WA (2004) The decline and rise of interstate migration in the United States: Evidence from the IPUMS, 1850–1990. Res Econ Hist 22:289–325. https://doi.org/10.1016/S0363-3268(04)22006-7
Ruggles S, Flood S, Goeken R, Grover J, Meyer E, Pacas J, Sobek M (2020) IPUMS USA: Version 10.0 [dataset]. IPUMS, Minneapolis https://doi.org/10.18128/D010.V10.0
Saavedra LA (2000) A model of welfare competition with evidence from AFDC. J Urban Econ 47(2):248–279. https://doi.org/10.1006/juec.1999.2141
Schwartz AL, Sommers BD (2014) Moving for Medicaid? Recent eligibility expansions did not induce migration from other States. Health Aff 33(1):88–94. https://doi.org/10.1377/hlthaff.2013.0910
Snarr HW, Burkey ML (2006) A preliminary investigation of welfare migration induced by time limits. J Reg Anal Policy 36(2):124–139
Stringfellow A (2017) What are Medicaid State to State transfer rules? Understanding how State-to-State transfers work and how to transfer your Medicaid benefits. https://blog.caregiverhomes.com/what-are-medicaid-state-to-state-transfer-rules-understanding-how-state-to-state-transfers-work-and-how-to-transfer-your-medicaid-benefits. Accessed 13 Dec 2021
The Henry J. Kaiser Family Foundation (2019) Status of State action on the Medicaid expansion decision. The Henry J. Kaiser Family Foundation. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/. Accessed 13 Dec 2021
Tiebout CM (1956) A pure theory of local expenditures. J Polit Econ 64(5):416–424. https://doi.org/10.1086/257839
US Census Bureau (2018) Survey data collection and methodology considerations. https://www.census.gov/topics/income-poverty/poverty/guidance/survey-data-collection.html. Accessed 13 Dec 2021
Willage B (2020) Unintended consequences of health insurance: Affordable Care Act’s free contraception mandate and risky sex. Health Econ 29(1):30–45. https://doi.org/10.1002/hec.3967
Funding
A doctoral scholarship by the Dresden Leibniz Graduate School, Dresden, Germany, partly supported this research.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
F. Seifert declares that she has no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Data accessibility statement
The base data is downloadable free of charge after registration from the IPUMS USA website https://usa.ipums.org (Ruggles et al. 2020). The compiled panel datasets are available from the author upon reasonable request.
Code availability
The empirical analyses were performed using STATA. The codes are available from the author upon reasonable request.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seifert, F. The Affordable Care Act Medicaid expansion and interstate migration in border regions of US States. Rev Reg Res 42, 49–74 (2022). https://doi.org/10.1007/s10037-022-00165-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10037-022-00165-2