Abstract
Purpose
Literature reviews outline minimally invasive approaches for abdominal diastasis in patients without skin excess. However, few surgeons are trained in endoscopic rectus sheath plication, and no simulated training programs exist for this method. This study aimed to develop and validate a synthetic simulation model for the training of skills in this approach under the Messick validity framework.
Methods
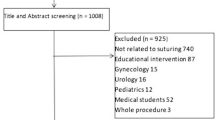
A cross-sectional study was carried out to assess the participants’ previous level of laparoscopic/endoscopic skills by a questionnaire. Participants performed an endoscopic plication on the model and their performance was evaluated by one blinded observer using the global rating scale OSATS and a procedure specific checklist (PSC) scale. A 5-level Likert survey was applied to 5 experts and 4 plastic surgeons to assess Face and Content validity.
Results
Fifteen non-experts and 5 experts in abdominal wall endoscopic surgery were recruited. A median OSATS score [25 (range 24–25) vs 14 (range 5–22); p < 0.05 of maximum 25 points] and a median PSC score [11 (range 10–11) vs 8 (range 3–10); p < 0.05 of maximum 11 points] was significantly higher for experts compared with nonexperts. All experts agreed or strongly agreed that the model simulates a real scenario of endoscopic plication of the rectus sheath.
Conclusion
Our simulation model met all validation criteria outlined in the Messick framework, demonstrating its ability to differentiate between experts and non-experts based on their baseline endoscopic surgical skills. This model stands as a valuable tool for evaluating skills in endoscopic rectus sheath plication.




Similar content being viewed by others
References
Boissonnault JS, Blaschak MJ (1988) Incidence of diastasis recti abdominis during the childbearing year. Phys Ther 68(7):1082–1086. https://doi.org/10.1093/ptj/68.7.1082
Chiarello CM, Falzone LA, McCaslin KE, Patel MN, Ulery KR (2005) The Effects of an Exercise Program on Diastasis Recti Abdominis in Pregnant Women. J Women’s Health Phys Ther 29(1):11–16. https://doi.org/10.1097/01274882-200529010-00003
Coldron Y, Stokes MJ, Newham DJ, Cook K (2008) Postpartum characteristics of rectus abdominis on ultrasound imaging. Man Ther 13(2):112–121. https://doi.org/10.1016/j.math.2006.10.001
Nahabedian MY (2018) Management Strategies for Diastasis Recti. Semin Plast Surg 32(3):147–154. https://doi.org/10.1055/s-0038-1661380
Bellido Luque J, Bellido Luque A, Valdivia J et al (2015) Totally endoscopic surgery on diastasis recti associated with midline hernias. The advantages of a minimally invasive approach. Prospective cohort study. Hernia 19(3):493–501. https://doi.org/10.1007/s10029-014-1300-2
Pitanguy I (1967) Abdominoplastias [Abdominal plastic surgery]. Hosp Rio Janeiro Brazil 71(6):1541–1556
Nahas FX (2001) An aesthetic classification of the abdomen based on the myoaponeurotic layer. Plast Reconstr Surg 108(6):1787–1797. https://doi.org/10.1097/00006534-200111000-00057
Sperstad JB, Tennfjord MK, Hilde G, Ellström-Engh M, Bø K (2016) Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med 50(17):1092–1096. https://doi.org/10.1136/bjsports-2016-096065
Ranney B (1990) Diastasis recti and umbilical hernia causes, recognition and repair. S D J Med 43(10):5–8
Lockwood T, Core GB (1998) Rectus Muscle Diastasis in Males: Primary Indication for Endoscopically Assisted Abdominoplasty. Plast and Reconstr Surg 101(6):1692–1694. https://doi.org/10.1097/00006534-199805000-00042
Faria Corrêa MA (1992) Videoendoscopic abdominoplasty (subcutaneoscopy). Rev Soc Bras Cir Plast Est Reconstr 7:32–34
Faria Corrêa MA (1995) Videoendoscopic Subcutaneous Techniques for Aesthetic and Reconstructive Plastic Surgery. Plast Reconstr Surg 96(2):446–453. https://doi.org/10.1097/00006534-199508000-00030
Core GB, Mizgala CL, Bowen JC et al (1995) Endoscopic abdominoplasty with repair of diastasis recti and abdominal wall hernia. Clin Plast Surg 22:707–722
Zukowski ML, Ash K, Spencer D, Malanoski M, Moore G (1998) Endoscopic intracorporal abdominoplasty: a review of 85 cases. Plast Reconstr Surg 102(2):516–527. https://doi.org/10.1097/00006534-199808000-00037
Iglesias M, Bravo L, Chavez-Muñoz C, Barajas-Olivas A (2006) Endoscopic abdominoplasty: an alternative approach. Ann Plast Surg 57(5):489–494. https://doi.org/10.1097/01.sap.0000229004.25059.87
Claus CMP, Malcher F, Cavazzola LT et al (2018) Subcutaneous onlay laparoscopic approach (scola) for ventral hernia and rectus abdominis diastasis repair: technical description and initial results. Arq Bras Cir Dig. https://doi.org/10.1590/0102-672020180001e1399
Muas Juarez DM (2019) Preaponeurotic endoscopic repair (REPA) of diastasis recti associated or not to midline hernias. Surg Endosc 33(6):1777–1782. https://doi.org/10.1007/s00464-018-6450-3
Varas J, Mejía R, Riquelme A, Maluenda F, Buckel E, Salinas J, Martínez J, Aggarwal R, Jarufe N, Boza C (2012) Significant transfer of surgical skills obtained with an advanced laparoscopic training program to a laparoscopic jejunojejunostomy in a live porcine model: feasibility of learning advanced laparoscopy in a general surgery residency. Surg Endosc 26(12):3486–3494. https://doi.org/10.1007/s00464-012-2391-4
Boza C, León F, Buckel E, Riquelme A, Crovari F, Martínez J, Aggarwal R, Grantcharov T, Jarufe N, Varas J (2016) Simulation-trained junior residents perform better than general surgeons on advanced laparoscopic cases. Surg Endosc 31(1):135–141. https://doi.org/10.1007/s00464-016-4942-6
Messick S (1994) Validity of Psychological Assessment: Validation of Inferences from Persons’ Responses and Performances as Scientific Inquiry into Score Meaning. ETS Research Report Series 1994(2):i–28. https://doi.org/10.1002/j.2333-8504.1994.tb01618.x
Goldenberg M, Lee JY (2018) Surgical Education, Simulation, and Simulators-Updating the Concept of Validity. Curr Urol Rep 19(7):52. https://doi.org/10.1007/s11934-018-0799-7
Martin JA, Reznick RK (1994) Reliability and validity of an instrument to evaluate operative skill in surgical residents. Can J Surg 37:342
Martin JA, Regehr G, Reznick R, MacRae H, Murnaghan J, Hutchison C, Brown M (1997) Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg 84(2):273–278. https://doi.org/10.1046/j.1365-2168.1997.02502.x
Ávila R, Tirado PA, Sufan RT et al (2017) Validación de modelo de entrenamiento basado en simulación para adquirir habilidades en trauma complejo cardiopulmonar. Investig Edu Med 6(22):130
Jarry C, Inzunza M, Bellolio F, Marino C, Achurra P, Varas J, Larach JT (2020) Desarrollo y evaluacion de modelo exvivo para entrenamiento de anastomosis intracorporea en hemicolectomia derecha laparoscopica. Rev Cir 72(3):209–216
Achurra P, Lagos A, Avila R et al (2017) Allowing New Opportunities in Advanced Laparoscopy Training Using a Full High-Definition Training Box. Surg Innov 24(1):66–71. https://doi.org/10.1177/1553350616672
Hollensteiner M, Malek M, Augat P, Fürst D, Schrödl F, Hunger S, Esterer B, Gabauer S, Schrempf A (2018) Validation of a simulator for cranial graft lift training: Face, content, and construct validity. J Craniomaxillofac Surg 46(8):1390–1394. https://doi.org/10.1016/j.jcms.2018.05.036
Messick S (1989) Validity. In: Linn RL (ed) Educational measurement, 3rd edn. Macmillan, New York, pp 13–103
Cronbach LJ (1971) Test validation. In: Thorndike RL (ed) Educational measurement, 2nd edn. American Council on Education, Washington, DC, pp 443–507
Cook DA, Beckman TJ (2006) Current concepts in validity and reliability for psychometric instruments: theory and application. Am J Med. https://doi.org/10.1016/j.amjmed.2005.10.036
Beckman TJ, Cook DA, Mandrekar JN (2005) What is the validity evidence for assessments of clinical teaching? J Gen Intern Med 20:1159–1164
Hatala R, Cook DA, Brydges R, Hawkins R (2015) Constructing a validity argument for the objective structured assessment of technical skills (OSATS): a systematic review of validity evidence. Adv Health Sci Educ Theory Pract 20:1149–1175. https://doi.org/10.1007/s10459-015-9593-1
Chang OH, King LP, Modest AM, Hur HC (2016) Developing an objective structured assessment of technical skills for laparoscopic suturing and intracorporeal knot tying. J Surg Educ 73(2):258–263. https://doi.org/10.1016/j.jsurg.2015.10.006
Steigerwald SN, Park J, Hardy KM, Gillman L, Vergis AS (2016) Establishing the concurrent validity of general and technique-specific skills assessments in surgical education. Am J Surg 211:268–273. https://doi.org/10.1016/j.amjsurg.2015.04.024
Vergis A, Steigerwald S (2017) A Preliminary Investigation of General and Technique-specific Assessments for the Evaluation of Laparoscopic Technical Skills. Cureus 9(10):e1757. https://doi.org/10.7759/cureus.1757
Azevedo MA, Santos HMG, Oliveira GBT, Favaro ML, Cavazolla LT (2021) Training model in abdominal wall endoscopic surgery for ventral hernias Extended totally extra-peritoneal approach (e-tep). Acta Cir Bras. https://doi.org/10.1590/ACB360808
Slater GH, Jourdan I, Fölscher DJ, Snook AL, Cooper M, D’Allessandro P, Rangeley C, Bailey ME (2001) The Guildford MATTU TEP hernia model. Surg Endosc 15:493–496. https://doi.org/10.1007/s004640000361
Kurashima Y, Feldman LS, Al-Sabah S, Kaneva PA, Fried GM, Vassiliou MC (2011) A novel low-cost simulator for laparoscopic inguinal hernia repair. Surg Innov 18:171–175. https://doi.org/10.1177/1553350610395949
Dawe SR, Pena GN, Windsor JA, Broeders JA, Cregan PC, Hewett PJ, Maddern GJ (2014) Systematic review of skills transfer after surgical simulation-based training. Br J Surg 101(9):1063–1076. https://doi.org/10.1002/bjs.9482
de Montbrun SL, MacRae H (2012) Simulation in Surgical Education. Clin Colon Rectal Surg 25(03):156–165. https://doi.org/10.1055/s-0032-1322553
Ujiki M, Zhao JC (2011) Simulation Training in Surgery. Dis Mon 57(12):789–801. https://doi.org/10.1016/j.disamonth.2011.08.018
Zevin B, Dedy NJ, Bonrath EM, Grantcharov TP (2017) Comprehensive simulation-enhanced training curriculum for an advanced minimally invasive procedure: a randomized controlled trial. Surg Obes Relat Dis 13(5):815–824. https://doi.org/10.1016/j.soard.2016.11.019
Funding
This study was financed by own funds and by funds of the Experimental Surgery and Simulation Center of the Pontificia Universidad Católica de Chile.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were carried out by María Fernanda Rojas and Javier Torres. The first draft of the manuscript was written by María Fernanda Rojas and all authors provided feedback on subsequent versions. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Pontificia Universidad Católica de Chile Ethics Committee.
Human and animal rights
The study included human participants and was performed in accordance with the ethical standards of the Declaration of Helsinki and its later amendments.
Informed consent
All participants provided informed consent after receiving a general explanation of the surgical procedure, the simulator, and the study design.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (AVI 225031 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rojas, M.F., Torres, J., Figueroa, Ú. et al. Validation of a synthetic simulation model of endoscopic rectus sheath plication. Hernia (2024). https://doi.org/10.1007/s10029-024-03059-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10029-024-03059-z