Abstract
Purpose
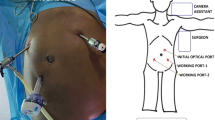
Risk of total extraperitoneal hernia repair (TEP) in patients with previous lower abdominal surgery (PLAS) is still debated. The present study was designed to assess the rate of conversion in TEP for inguinal hernia stratified by type of PLAS.
Methods
Variables on patients undergoing TEP inguinal hernia repair at our center were prospectively collected between July 2012 and May 2018. Patients with PLAS were compared to patients without PLAS. Furthermore, the most frequent subtypes of PLAS were defined and TEP conversion rate was stratified according to type of PLAS.
Results
A total of 1589 patients with TEP inguinal hernia repair were identified including 152 (9.6%) patients with PLAS. Operative time was increased in patients with PLAS (70 vs. 60 min, p < 0.001). Conversion from TEP to transabdominal preperitoneal patch plasty (TAPP) or Lichtenstein open inguinal hernia repair was eight-times more frequent after PLAS (8% vs. 1%, p < 0.001). Considering type of PLAS, open appendectomy was most frequently encountered, followed by multiple PLAS and surgery to the bladder and prostate (53%, 11% and 10%). After stratification for type of PLAS, conversions were most frequently found after previous surgery to the bladder or prostate and after multiple PLAS (conversion rate of 20% and 24%, p < 0.001). In contrast, conversion rate after open appendectomy was not increased.
Conclusion
PLAS to the bladder and prostate is associated with TEP conversion. Selected patients might profit from a different operative approach for inguinal hernia repair.
Similar content being viewed by others
Data availability
A data availability statement is not available.
References
The HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165. https://doi.org/10.1007/s10029-017-1668-x
Bittner R (2006) Laparoscopic surgery—15 years after clinical introduction. World J Surg 30:1190–1203. https://doi.org/10.1007/s00268-005-0644-2
Bittner R, Schwarz J (2012) Inguinal hernia repair: current surgical techniques. Langenbecks Arch Surg 397:271–282. https://doi.org/10.1007/s00423-011-0875-7
O’Reilly EA, Burke JP, O’Connell PR (2012) A meta-analysis of surgical morbidity and recurrence after laparoscopic and open repair of primary unilateral inguinal hernia. Ann Surg 255(5):846–853. https://doi.org/10.1097/SLA.0b013e31824e96cf
Aly O, Green A, Joy M, Wong CH, Al Kandari A, Cheng S (2011) Is laparoscopic inguinal hernia repair more effective than open repair? J College Physicians Surg Pak 21(5):291–296 (IMEMR | ID: emr-131103)
Kuhry E, van Veen RN, Langeveld HR et al (2007) Open or endoscopic total extraperitoneal inguinal hernia repair? A systematic review. Surg Endosc 21:161–166. https://doi.org/10.1007/s00464-006-0167-4
McCormack K, Wake B, Perez J et al (2005) Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation. Health Technol Assess (Winchester, England) 9(14):1–203. https://doi.org/10.3310/hta9140. (iii–iv)
Memon MA, Cooper NJ, Memon B, Memon MI, Abrams KR (2003) Meta-analysis of randomized clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg 90(12):1479–1492. https://doi.org/10.1002/bjs.4301
Andersson B et al (2003) Laparoscopic extraperitoneal inguinal hernia repair versus open mesh repair: a prospective randomized controlled trial. Surgery 133(5):464–472. https://doi.org/10.1067/msy.2003.98
Ramshaw BJ et al (1996) The effect of previous lower abdominal surgery on performing the total extraperitoneal approach to laparoscopic herniorrhaphy. Am Surg 62(4):292–294
Bringman S et al (2003) Tension-free inguinal hernia repair: TEP versus mesh-plug versus Lichtenstein: a prospective randomized controlled trial. Ann Surg 237(1):142. https://doi.org/10.1097/00000658-200301000-00020
Wright D, Paterson C, Scott N, Hair A, O’Dwyer PJ (2002) Five-year follow-up of patients undergoing laparoscopic or open groin hernia repair: a randomized controlled trial. Ann Surg 235(3):333–337
Stechemesser B, Jacob DA, Schug-Paß C et al (2012) Herniamed: an internet-based registry for outcome research in hernia surgery. Hernia 16:269–276. https://doi.org/10.1007/s10029-012-0908-3
Miserez M, Alexandre JH, Campanelli G et al (2007) The European hernia society groin hernia classication: simple and easy to remember. Hernia 11:113–116. https://doi.org/10.1007/s10029-007-0198-3
Zárate Gómez J, Álvarez De Sierra Hernández P, Bernal Marco B, Fernández Luengas D, Conde Someso S, Supelano Eslait G, Peinado Iríbar B, Merello Godino J, OC-044 (2022) Total extraperitoneal endoscopic inguinal hernioplasty (TEP) in patients with previous lower abdominal surgery. Is it a worrisome indication? Br J Surg 109(Supplement_7):znac308.056. https://doi.org/10.1093/bjs/znac308.056
Prassas D et al (2019) Effect of previous lower abdominal surgery on outcomes following totally extraperitoneal (TEP) inguinal hernia repair. Surg Laparosc Endosc Percutan Tech 29(4):267–270. https://doi.org/10.1097/SLE.0000000000000633
Trawa M, Albrecht HC, Köckerling F, Riediger H, Adolf D, Gretschel S (2022) Outcome of inguinal hernia repair after previous radical prostatectomy: a registry-based analysis with 12,465 patients. Hernia 26(4):1143–1152. https://doi.org/10.1007/s10029-022-02635-5
Le Page P, Smialkowski A, Morton J et al (2013) Totally extraperitoneal inguinal hernia repair in patients previously having prostatectomy is feasible, safe, and effective. Surg Endosc 27:4485–4490. https://doi.org/10.1007/s00464-013-3094-1
Özata H, Sucu S, Karahan SN, Kılıçoğlu BK, Kalender M, Camcı F, Balık E (2023) Feasibility of totally extraperitoneal inguinal hernia repair in patients with previous prostatectomy. Turk J Surg 39(3):258. https://doi.org/10.47717/turkjsurg.2023.6198
La Regina D, Gaffuri P, Ceppi M, Saporito A, Ferrari M, Di Giuseppe M, Mongelli F (2019) Safety, feasibility and clinical outcome of minimally invasive inguinal hernia repair in patients with previous radical prostatectomy: a systematic review of the literature. J Minim Access Surg 15(4):281. https://doi.org/10.4103/jmas.JMAS_218_18
Dulucq JL, Wintringer P, Mahajna A (2006) Totally extraperitoneal (TEP) hernia repair after radical prostatectomy or previous lower abdominal surgery. Surg Endosc 20:473–476. https://doi.org/10.1007/s00464-006-3027-3
Hyae PJ, Choi YY, Hur KY (2010) The feasibility of laparoscopic total extraperitoneal (TEP) herniorrhaphy after previous lower abdominal surgery. J Korean Surg Soc 78(6):405–409. https://doi.org/10.4174/jkss.2010.78.6.405
Zuiki T, Ohki J, Ochi M et al (2018) Laparoscopic totally extraperitoneal (TEP) inguinal hernia repair in patients with previous lower abdominal surgery. Surg Endosc 32:4757–4762. https://doi.org/10.1007/s00464-018-6223-z
Elshof JWM, Keus F, Burgmans JPJ et al (2009) Feasibility of right-sided total extraperitoneal procedure for inguinal hernia repair after appendectomy: a prospective cohort study. Surg Endosc 23:1754–1758. https://doi.org/10.1007/s00464-008-0187-3
Al-Sahaf O et al (2008) Totally extraperitoneal laparoscopic inguinal hernia repair is a safe option in patients with previous lower abdominal surgery. J Laparoendosc Adv Surg Tech 18(3):353–356. https://doi.org/10.1089/lap.2007.0071
Chung SD, Huang CY, Chueh SC et al (2011) Feasibility and safety of total extraperitoneal inguinal hernia repair after previous lower abdominal surgery: a case–control study. Surg Endosc 25:3353–3356. https://doi.org/10.1007/s00464-011-1724-z
Wakasugi M, Suzuki Y, Tei M et al (2017) The feasibility and safety of single-incision totally extraperitoneal inguinal hernia repair after previous lower abdominal surgery: 350 procedures at a single center. Surg Today 47:307–312. https://doi.org/10.1007/s00595-016-1376-7
Schouten N, Simmermacher RKJ, van Dalen T et al (2013) Is there an end of the “learning curve” of endoscopic totally extraperitoneal (TEP) hernia repair? Surg Endosc 27:789–794. https://doi.org/10.1007/s00464-012-2512-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there are no financial or non-financial interests that are directly or indirectly related to the work submitted for publication.
Ethical approval
The study was approved by the ethics committee of northwest- and central Switzerland EKNZ (Project-ID 2019-02074).
Human and animal rights
Not applicable.
Informed consent
For this type of study, formal consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Merker, H., Slieker, J., Frey, M. et al. Risk of conversion after intended total extraperitoneal hernia repair for inguinal hernia depends on type of previous abdominal surgery. Hernia (2024). https://doi.org/10.1007/s10029-024-02997-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10029-024-02997-y