Abstract
Purpose
Using small instead of large bites for laparotomy closure results in lower incidence of incisional hernia, but no consensus exists on which suture material to use. This study aimed to compare five different closure strategies in a standardized experimental setting.
Methods
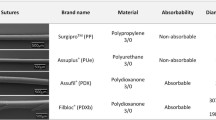
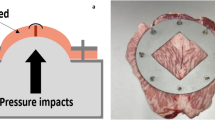
Fifty porcine abdominal walls were arranged into 5 groups: (A) running 2/0 polydioxanone; (B) interlocking 2/0 polydioxanone; (C) running size 0 barbed polydioxanone; (D) running size 0 barbed glycolic acid and trimethylene carbonate; (E) running size 0 suturable polypropylene mesh. The small-bites technique was used for linea alba closure in all. The abdominal walls were divided into a supra- and infra-umbilical half, resulting in 20 specimens per group that were pulled apart in a tensile testing machine. Maximum tensile force and types of suture failure were registered.
Results
The highest tensile force was measured when using barbed polydioxanone (334.8 N ± 157.0), but differences did not reach statistical significance. Infra-umbilical abdominal walls endured a significantly higher maximum tensile force compared to supra-umbilical (397 N vs 271 N, p < 0.001). Barbed glycolic acid and trimethylene carbonate failed significantly more often (25% vs 0%, p = 0.008).
Conclusion
Based on tensile force, both interlocking and running suture techniques using polydioxanone, and running sutures using barbed polydioxanone or suturable mesh, seem to be suitable for abdominal wall closure. Tensile strength was significantly higher in infra-umbilical abdominal walls compared to supra-umbilical. Barbed glycolic acid and trimethylene carbonate should probably be discouraged for fascial closure, because of increased risk of suture failure.



Similar content being viewed by others
Data availability statement
The data that support the findings of this study are available on request from the corresponding author.
References
Jairam AP, Timmermans L, Eker HH et al (2017) Prevention of incisional hernia with prophylactic onlay and sublay mesh reinforcement versus primary suture only in midline laparotomies (PRIMA): 2-year follow-up of a multicentre, double-blind, randomised controlled trial. The Lancet 390:567–576. https://doi.org/10.1016/S0140-6736(17)31332-6
Höer J, Lawong G, Klinge U, Schumpelick V (2002) Einflussfaktoren der narbenhernienentstehung retrospektive untersuchung an 2.983 laparotomierten Patienten über einen Zeitraum von 10 Jahren. Chirurg 73:474–480. https://doi.org/10.1007/s00104-002-0425-5
Alnassar S, Bawahab M, Abdoh A et al (2012) Incisional hernia postrepair of abdominal aortic occlusive and aneurysmal disease: five-year incidence. Vascular 20:273–277. https://doi.org/10.1258/vasc.2011.oa0332
Bosanquet DC, Ansell J, Abdelrahman T et al (2015) Systematic review and meta-regression of factors affecting midline incisional hernia rates: analysis of 14 618 patients. PLoS ONE 10:e0138745. https://doi.org/10.1371/journal.pone.0138745
van Ramshorst GH, Eker HH, Hop WCJ et al (2012) Impact of incisional hernia on health-related quality of life and body image: a prospective cohort study. The Am J Surg 204:144–150. https://doi.org/10.1016/j.amjsurg.2012.01.012
Gillion J-F, Sanders D, Miserez M, Muysoms F (2016) The economic burden of incisional ventral hernia repair: a multicentric cost analysis. Hernia 20:819–830. https://doi.org/10.1007/s10029-016-1480-z
Khorgami Z, Hui BY, Mushtaq N et al (2019) Predictors of mortality after elective ventral hernia repair: an analysis of national inpatient sample. Hernia 23:979–985. https://doi.org/10.1007/s10029-018-1841-x
Kudsi OY, Kaoukabani G, Bou-Ayash N et al (2023) A comparison of clinical outcomes and costs between robotic and open ventral hernia repair. The Am J Surg 226:87–92. https://doi.org/10.1016/j.amjsurg.2023.01.031
Deerenberg EB, Henriksen NA, Antoniou GA et al (2022) Updated guideline for closure of abdominal wall incisions from the European and American hernia societies. Br J Surg 109:1239–1250. https://doi.org/10.1093/bjs/znac302
Muysoms FE, Antoniou SA, Bury K et al (2015) European hernia society guidelines on the closure of abdominal wall incisions. Hernia 19:1–24. https://doi.org/10.1007/s10029-014-1342-5
Millbourn D (2009) Effect of stitch length on wound complications after closure of midline incisions. Arch Surg 144:1056. https://doi.org/10.1001/archsurg.2009.189
Deerenberg EB, Harlaar JJ, Steyerberg EW et al (2015) Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicentre, randomised controlled trial. The Lancet 386:1254–1260. https://doi.org/10.1016/S0140-6736(15)60459-7
Harlaar JJ, van Ramshorst GH, Nieuwenhuizen J et al (2009) Small stitches with small suture distances increase laparotomy closure strength. The Am J Surg 198:392–395. https://doi.org/10.1016/j.amjsurg.2008.10.018
Jenkins TPN (2005) The burst abdominal wound: A mechanical approach. Br J Surg 63:873–876. https://doi.org/10.1002/bjs.1800631110
Henriksen NA, Deerenberg EB, Venclauskas L et al (2018) Meta-analysis on materials and techniques for laparotomy closure: the match review. World J Surg 42:1666–1678. https://doi.org/10.1007/s00268-017-4393-9
Bloemen A, De Kleijn RJCMF, Van Steensel S et al (2019) Laparotomy closure techniques: do surgeons follow the latest guidelines? Results of a questionnaire. Int J Surg 71:110–116. https://doi.org/10.1016/j.ijsu.2019.09.024
Ruiz-Tovar J, Llavero C, Jimenez-Fuertes M et al (2020) Incisional surgical site infection after abdominal fascial closure with triclosan-coated barbed suture vs triclosan-coated polydioxanone loop suture vs polydioxanone loop suture in emergent abdominal surgery: a randomized clinical trial. J Am Coll Surg 230:766–774. https://doi.org/10.1016/j.jamcollsurg.2020.02.031
Deeken CR, Lake SP (2017) Mechanical properties of the abdominal wall and biomaterials utilized for hernia repair. J Mech Behav Biomed Mater 74:411–427. https://doi.org/10.1016/j.jmbbm.2017.05.008
Levillain A, Orhant M, Turquier F, Hoc T (2016) Contribution of collagen and elastin fibers to the mechanical behavior of an abdominal connective tissue. J Mech Behav Biomed Mater 61:308–317. https://doi.org/10.1016/j.jmbbm.2016.04.006
Irfan A, Cochrun S, He K et al (2023) Towards identifying a learning curve for robotic abdominal wall reconstruction: a cumulative sum analysis. Hernia 27:671–676. https://doi.org/10.1007/s10029-023-02794-z
Templeton MM, Krebs AI, Kraus KH, Hedlund CS (2015) Ex vivo biomechanical comparison of V-Loc 180® absorbable wound closure device and standard polyglyconate suture for diaphragmatic herniorrhaphy in a canine model. Vet Surg 44:65–69. https://doi.org/10.1111/j.1532-950X.2014.12201.x
Oni G, Brown SA, Kenkel JM (2012) A Comparison between barbed and nonbarbed absorbable suture for fascial closure in a porcine model. Plast Reconstr Surg 130:535e–540e. https://doi.org/10.1097/PRS.0b013e318262f0f6
Shimizu N, Tarlton J, Friend E et al (2017) Tensile comparison of polydioxanone, polyglyconate, and barbed glycolide-trimethylene carbonate suture in canine cadaveric tensor fascia lata. Vet Surg 46:89–94. https://doi.org/10.1111/vsu.12580
Scheiber CJ, Kurapaty SS, Goldman SM et al (2020) Suturable mesh better resists early laparotomy failure in a cyclic ball-burst model. Hernia 24:559–565. https://doi.org/10.1007/s10029-020-02133-6
Souza JM, Dumanian ZP, Gurjala AN, Dumanian GA (2015) In Vivo evaluation of a novel mesh suture design for abdominal wall closure. Plast Reconstr Surg 135:322e–330e. https://doi.org/10.1097/PRS.0000000000000910
Xing L, Culbertson EJ, Wen Y, Franz MG (2013) Early laparotomy wound failure as the mechanism for incisional hernia formation. J Surg Res 182:e35–e42. https://doi.org/10.1016/j.jss.2012.09.009
Yurtkap Y, den Hartog FPJ, van Weteringen W et al (2020) Evaluation of a new suture material (Duramesh™) by measuring suture tension in small and large bites techniques for laparotomy closure in a porcine model. Hernia 24:1317–1324. https://doi.org/10.1007/s10029-020-02140-7
Fortelny RH, Andrade D, Schirren M et al (2022) Effects of the short stitch technique for midline abdominal closure on incisional hernia (ESTOIH): randomized clinical trial. Br J Surg 109:839–845. https://doi.org/10.1093/bjs/znac194
Funding
This study received no financial support from extramural sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Neither human nor live animal subjects were used in this study. As such, per local institutional guidelines, no ethical approval was needed.
Conflict of interest
The authors have no competing conficts of interest to disclose.
Human and animal rights
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Allaeys, M., Visscher, L., den Hartog, F.P.J. et al. Strength of small-bites abdominal wall closure using different suturing methods and materials in an experimental animal model. Hernia 28, 527–535 (2024). https://doi.org/10.1007/s10029-023-02945-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-023-02945-2