Abstract
Purpose
Obesity and smoking are associated with postoperative wound complications following open hernia repair. However, with the advancements in minimally invasive surgical techniques, we hypothesized that obese and/or smoking patients undergoing minimally invasive repairs were not subjected to an increased risk of postoperative surgical complications. As opposed to nonobese and/or nonsmoking patients.
Methods
This was a retrospective cohort study including patients undergoing minimally invasive retromuscular repair at a single university hospital. Patients were divided into two groups according to exposure; obese vs. nonobese and smoking vs. nonsmoking. One month postoperatively, all patients underwent clinical follow-up. The main outcome was surgical site occurrence (SSO).
Results
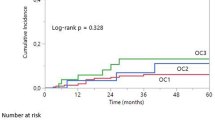
A total of 94 patients were included, undergoing both laparoscopic (n = 32) and robotic (n = 62) retromuscular repair. Of these, 7.7% of the obese patients had SSO when compared with 19.1% of the nonobese patients. A total of 17.2% of the nonsmokers had SSO compared with 13.3% of the active smokers. Of the nonsmokers, 12.5% developed seroma and 6.2% hematoma postoperatively, the corresponding numbers were 13.3% and 0% among the active smokers. After multivariable analysis, there was no significant risk factors for developing postoperative SSO.
Conclusion
There was no association between obesity or smoking and surgical complication in patients undergoing minimally invasive retromuscular repair. If the results of the current study are confirmed, patients who are unable to obtain weight loss or smoking cessation may be offered minimally invasive retromuscular ventral hernia repair without inducing an increased risk of short-term complications.

Similar content being viewed by others
References
Jensen KK, Emmertsen KJ, Laurberg S, Krarup PM (2020) Long-term impact of incisional hernia on quality of life after colonic cancer resection. Hernia 24(2):265–272. https://doi.org/10.1007/s10029-019-01978-w
Oma E, Jensen KK, Jorgensen LN (2016) Recurrent umbilical or epigastric hernia during and after pregnancy: a nationwide cohort study. Surg (United States) 159(6):1677–1683. https://doi.org/10.1016/j.surg.2015.12.025
Christoffersen MW, Westen M, Rosenberg J, Helgstrand F, Bisgaard T (2020) Closure of the fascial defect during laparoscopic umbilical hernia repair: a randomized clinical trial. Br J Surg 107(3):200–208. https://doi.org/10.1002/bjs.11490
Bui NH, Jørgensen LN, Jensen KK (2021) Laparoscopic intraperitoneal versus enhanced-view totally extraperitoneal retromuscular mesh repair for ventral hernia: a retrospective cohort study. Surg Endosc. https://doi.org/10.1007/s00464-021-08436-8
Belyansky I, Daes J, Radu VG et al (2018) A novel approach using the enhanced-view totally extraperitoneal (eTEP) technique for laparoscopic retromuscular hernia repair. Surg Endosc 32(3):1525–1532. https://doi.org/10.1007/s00464-017-5840-2
Muysoms F, Van Cleven S, Pletinckx P, Ballecer C, Ramaswamy A (2018) Robotic transabdominal retromuscular umbilical prosthetic hernia repair (TARUP): observational study on the operative time during the learning curve. Hernia 22(6):1101–1111. https://doi.org/10.1007/s10029-018-1825-x
Petro CC, Prabhu AS (2018) Preoperative planning and patient optimization. Surg Clin North Am 98(3):483–497. https://doi.org/10.1016/j.suc.2018.01.005
Lindström D, Azodi OS, Wladis A et al (2008) Effects of a perioperative smoking cessation intervention on postoperative complications: a randomized trial. Ann Surg 248(5):739–745. https://doi.org/10.1097/SLA.0b013e3181889d0d
Liang MK, Bernardi K, Holihan JL et al (2018) Modifying risks in ventral hernia patients with prehabilitation: a randomized controlled trial. Ann Surg 268(4):674–680. https://doi.org/10.1097/SLA.0000000000002961
Sauerland S, Korenkov M, Kleinen T, Arndt M, Paul A (2004) Obesity is a risk factor for recurrence after incisional hernia repair. Hernia 8(1):42–46. https://doi.org/10.1007/s10029-003-0161-x
Juvany M, Hoyuela C, Carvajal F, Trias M, Martrat A, Ardid J (2018) Long-term follow-up (at 5 years) of midline incisional hernia repairs using a primary closure and prosthetic onlay technique: recurrence and quality of life. Hernia 22(2):319–324. https://doi.org/10.1007/s10029-018-1730-3
Alkhatib H, Tastaldi L, Krpata DM et al (2019) Impact of modifiable comorbidities on 30-day wound morbidity after open incisional hernia repair. Surg (United States) 166(1):94–101. https://doi.org/10.1016/j.surg.2019.03.011
Kudsi OY, Gokcal F (2021) Lateral approach totally extraperitoneal (TEP) robotic retromuscular ventral hernia repair. Hernia 25(1):211–222. https://doi.org/10.1007/s10029-019-02082-9
DeBord J, Novitsky Y, Fitzgibbons R, Miserez M, Montgomery A (2018) SSI, SSO, SSE, SSOPI: the elusive language of complications in hernia surgery. Hernia 22(5):737–738. https://doi.org/10.1007/s10029-018-1813-1
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 147(8):573–577. https://doi.org/10.7326/0003-4819-147-8-200710160-00010
Jensen KK, East B, Jisova B et al (2022) The European hernia society prehabilitation project: a systematic review of patient prehabilitation prior to ventral hernia surgery. Hernia. https://doi.org/10.1007/S10029-022-02573-2
Juul N, Henriksen NA, Jensen KK (2021) Increased risk of postoperative complications with retromuscular mesh placement in emergency incisional hernia repair: a nationwide register-based cohort study. Scand J Surg 110(2):193–198. https://doi.org/10.1177/1457496920966237
Henriksen NA, Jensen KK, Muysoms F (2019) Robot-assisted abdominal wall surgery: a systematic review of the literature and meta-analysis. Hernia 23(1):17–27. https://doi.org/10.1007/S10029-018-1872-3
Morrell ALG, Morrell AC, Cavazzola LT et al (2021) Robotic assisted eTEP ventral hernia repair: Brazilian early experience. Hernia 25(3):765–774. https://doi.org/10.1007/S10029-020-02233-3
Petro CC, Zolin S, Krpata D et al (2021) Patient-reported outcomes of robotic vs laparoscopic ventral hernia repair with intraperitoneal mesh: the PROVE-IT randomized clinical trial. JAMA Surg 156(1):22–29. https://doi.org/10.1001/JAMASURG.2020.4569
Olavarria OA, Bernardi K, Shah SK et al (2020) Robotic versus laparoscopic ventral hernia repair: multicenter, blinded randomized controlled trial. BMJ. https://doi.org/10.1136/bmj.m2457
Jensen KK (2020) Laparoscopic versus robot assisted repair of ventral hernia. BMJ. https://doi.org/10.1136/bmj.m2480
Jain M, Krishna A, Prakash O et al (2022) Comparison of extended totally extra peritoneal (eTEP) vs intra peritoneal onlay mesh (IPOM) repair for management of primary and incisional hernia in terms of early outcomes and cost effectiveness-a randomized controlled trial. Surg Endosc. https://doi.org/10.1007/S00464-022-09180-3
Carbonell AM, Criss CN, Cobb WS, Novitsky YW, Rosen MJ (2013) Outcomes of synthetic mesh in contaminated ventral hernia repairs. J Am Coll Surg 217(6):991–998. https://doi.org/10.1016/j.jamcollsurg.2013.07.382
Henriksen NA, Friis-Andersen H, Jorgensen LN, Helgstrand F (2021) Open versus laparoscopic incisional hernia repair: nationwide database study. BJS Open. https://doi.org/10.1093/BJSOPEN/ZRAA010
Oma E, Jensen KK, Jorgensen LN, Bisgaard T (2020) Incisional hernia repair in women of childbearing age: a nationwide propensity-score matched study. Scand J Surg 109(4):295–300. https://doi.org/10.1177/1457496919874482
Jensen KK, Backer V, Jorgensen LN (2017) Abdominal wall reconstruction for large incisional hernia restores expiratory lung function. Surg (United States) 161(2):517–524. https://doi.org/10.1016/j.surg.2016.08.015
Jensen KK, Munim K, Kjaer M, Jorgensen LN (2017) Abdominal wall reconstruction for incisional hernia optimizes truncal function and quality of life: a prospective controlled study. Ann Surg 265(6):1235–1240. https://doi.org/10.1097/SLA.0000000000001827
Jensen KK, Henriksen NA, Harling H (2014) Standardized measurement of quality of life after incisional hernia repair: a systematic review. Am J Surg 208(3):485–493. https://doi.org/10.1016/j.amjsurg.2014.04.004
Wolf LL, Ejiofor JI, Wang Y et al (2019) Management of reducible ventral hernias: clinical outcomes and cost-effectiveness of repair at diagnosis versus watchful waiting. Ann Surg 269(2):358–366. https://doi.org/10.1097/SLA.0000000000002507
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author J. R. Ekmann and M. W. Christoffersen declare that they have no conflict of interest. K. K. Jensen is a speaker for Intuitive.
Human and animal rights and Informed consent
This study was approved by the Danish Data Protection Agency. All patients gave informed consent to chart review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ekmann, J.R., Christoffersen, M.W. & Jensen, K.K. Short-term complications after minimally invasive retromuscular ventral hernia repair: no need for preoperative weight loss or smoking cessation?. Hernia 26, 1315–1323 (2022). https://doi.org/10.1007/s10029-022-02663-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-022-02663-1