Abstract
Purpose
Although many studies assessing enhanced recovery after surgery (ERAS) pathways in abdominal wall reconstruction (AWR) have recently demonstrated lower rates of postoperative morbidity and a decrease in postoperative length of stay compared to standard practice, the utility of ERAS in AWR remains largely unknown.
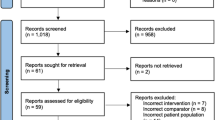
Methods
A systematic literature search for randomized and non-randomized studies comparing ERAS (ERAS +) pathways and standard protocols (Control) as an adopted practice for patients undergoing AWR was performed using MEDLINE, the Cochrane Central Register of Controlled Trials, Scopus, Web of Science, and EMBASE databases. A predefined search strategy was implemented. The included studies were reviewed for primary outcomes: overall postoperative morbidity, abdominal wall morbidity, surgical site infection (SSI), and length of hospital stay; and for secondary outcome: operative time, estimated blood loss, time to discontinuation of narcotics, time to urinary catheter removal, time to return to bowel function, time to return to regular diet, and readmission rate. Standardized mean difference (SMD) was calculated for continuous variables and Odds Ratio for dichotomous variables.
Results
Five non-randomized studies were included for qualitative and quantitative synthesis. 840 patients were allocated to either ERAS + (382) or Control (458). ERAS + and Control groups showed equivalent results with regard to the incidence of postoperative morbidity (OR 0.73, 95% CI 0.32–1.63; I2= 76%), SSI (OR 1.17, 95% CI 0.43–3.22; I2= 54%), time to return to bowel function (SMD − 2.57, 95% CI − 5.32 to 0.17; I2= 99%), time to discontinuation of narcotics (SMD − 0.61, 95% CI − 1.81 to 0.59; I2= 97%), time to urinary catheter removal (SMD − 2.77, 95% CI − 6.05 to 0.51; I2= 99%), time to return to regular diet (SMD − 0.77, 95% CI − 2.29 to 0.74; I2= 98%), and readmission rate (OR 0.82, 95% CI 0.52–1.27; I2= 49%). Length of hospital stay was significantly shorter in the ERAS + compared to the Control group (SMD − 0.93, 95% CI − 1.84 to − 0.02; I2= 97%).
Conclusions
The introduction of an ERAS pathway into the clinical practice for patients undergoing AWR may cause a decreased length of hospitalization. These results should be interpreted with caution, due to the low level of evidence and the high heterogeneity.



Similar content being viewed by others
References
Sauerland S, Walgenbach M, Habermalz B et al (2011) Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD007781.pub2
Hawn MT, Gray SH, Snyder CW et al (2011) Predictors of mesh explantation after incisional hernia repair. Am J Surg 202(1):28–33
Sanchez VM, Abi-Haidar YE, Itani KM (2011) Mesh infection in ventral incisional hernia repair: incidence, contributing factors, and treatment. Surg Infect (Larchmt) 12(3):205–210
Adamina M, Kehlet H, Tomlinson GA et al (2011) Enhanced recovery pathways optimize health outcomes and resource utilization: a meta-analysis of randomized controlled trials in colorectal surgery. Surgery 149(6):830–840
Spanjersberg WR, Reurings J, Keus F et al (2011) Fast track surgery versus conventional recovery strategies for colorectal surgery. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD007635.pub2
Nicholson A, Lowe MC, Parker J et al (2014) Systematic review and meta-analysis of enhanced recovery programmes in surgical patients. Br J Surg 101(3):172–188
Fayezizadeh M, Petro CC, Rosen MJ et al (2014) Enhanced recovery after surgery pathway for abdominal wall reconstruction: pilot study and preliminary outcomes. Plast Reconstr Surg 134(4 Suppl 2):151S–159S
Majumder A, Fayezizadeh M, Neupane R et al (2016) Benefits of multimodal enhanced recovery pathway in patients undergoing open ventral hernia repair. J Am Coll Surg 222(6):1106–1115
Warren JA, Stoddard C, Hunter AL et al (2017) Effect of multimodal analgesia on opioid use after open ventral hernia repair. J Gastrointest Surg 21(10):1692–1699
Colvin J, Rosen M, Prabhu A et al (2019) Enhanced recovery after surgery pathway for patients undergoing abdominal wall reconstruction. Surgery 166(5):849–853
Scott MJ, Miller TE (2015) Pathophysiology of major surgery and the role of enhanced recovery pathways and the anesthesiologist to improve outcomes. Anesthesiol Clin 33(1):79–91
Fischer JP, Wes AM, Wink JD et al (2014) Analysis of perioperative factors associated with increased cost following abdominal wall reconstruction (AWR). Hernia 18(5):617–624
Jensen KK, Brondum TL, Harling H et al (2016) Enhanced recovery after giant ventral hernia repair. Hernia 20(2):249–256
Macedo FIB, Mittal VK (2017) Does enhanced recovery pathways affect outcomes in open ventral hernia repair? Hernia 21(5):817–818
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. https://doi.org/10.1371/journal.pmed.1000100
Stroup DF, Berlin JA, Morton SC et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283(15):2008–2012
Higgins JPT, Green S (eds). Cochrane handbook for systematic reviews of interventions version 5.3.5. The Cochrane collaboration, 2019. www.handbook.cochrane.org. Accessed April 2020
Sterne JA, Hernán MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. https://doi.org/10.1136/bmj.i4919
Balshem H, Helfand M, Schünemann HJ et al (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64(4):401–406
GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University, 2015 (developed by Evidence Prime, Inc.). Available from gradepro.org
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13. https://doi.org/10.1186/1471-2288-5-13
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Stearns E, Plymale MA, Davenport DL et al (2018) Early outcomes of an enhanced recovery protocol for open repair of ventral hernia. Surg Endosc 32(6):2914–2922
Ueland W, Walsh-Blackmore S, Nisiewicz M et al (2019) The contribution of specific enhanced recovery after surgery (ERAS) protocol elements to reduced length of hospital stay after ventral hernia repair. Surg Endosc. https://doi.org/10.1007/s00464-019-07233-8
Warren JA, Carbonell AM, Jones LK et al (2019) Length of stay and opioid dose requirement with transversus abdominis plane block vs epidural analgesia for ventral hernia repair. J Am Coll Surg 228(4):680–686
Senagore AJ, Champagne BJ, Dosokey E et al (2017) Pharmacogenetics-guided analgesics in major abdominal surgery: further benefits within an enhanced recovery protocol. Am J Surg 213(3):467–472
Jensen KK, Dressler J, Baastrup NN et al (2019) Enhanced recovery after abdominal wall reconstruction reduces length of postoperative stay: an observational cohort study. Surgery. 165(2):393–397
Harryman C, Plymale MA, Stearns E et al (2019) Enhanced value with implementation of an ERAS protocol for ventral hernia repair. Surg Endosc. https://doi.org/10.1007/s00464-019-07166-2
Surgical Site Infection (SSI) Event: Center for Disease Control (2012). https://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf. Accessed April 3, 2020
Collaborative EuroSurg (2020) Safety of hospital discharge before return of bowel function after elective colorectal surgery. Br J Surg 107(5):552–559
Delaney CP, Brady K, Woconish D et al (2012) Towards optimizing perioperative colorectal care: outcomes for 1,000 consecutive laparoscopic colon procedures using enhanced recovery pathways. Am J Surg 203(3):353–356
Liang MK, Holihan JL, Itani K et al (2017) Ventral hernia management: expert consensus guided by systematic review. Ann Surg 265(1):80–89
Wick EC, Grant MC, Wu CL (2017) Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg 152(7):691–697
Prabhu AS, Krpata DM, Perez A et al (2018) Is it time to reconsider postoperative epidural analgesia in patients undergoing elective ventral hernia repair?: an AHSQC analysis. Ann Surg 267(5):971–976
Torgeson M, Kileny J, Pfeifer C et al (2018) Conventional epidural vs transversus abdominis plane block with liposomal bupivacaine: a randomized trial in colorectal surgery. J Am Coll Surg 227(1):78–83
Doble JA, Winder JS, Witte SR et al (2018) Direct visualization transversus abdominis plane blocks offer superior pain control compared to ultrasound guided blocks following open posterior component separation hernia repairs. Hernia 22(4):627–635
Slim K, Standaert D (2020) Enhanced recovery after surgical repair of incisional hernias. Hernia 24(1):3–8
Acknowledgements
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Alberto Sartori, Emanuele Botteri, Ferdinando Agresta, Chiara Gerardi, Nereo Vettoretto, Alberto Arezzo, Adolfo Pisanu, Giampiero Campanelli, Salomone Di Saverio, and Mauro Podda have no conflicts of interest or financial ties to disclose.
Ethical approval
No ethical approval was required for this article. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Research involving human participants and/or animals
This study does not include human or animal participants.
Informed consent
Informed consent was not required for this review study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sartori, A., Botteri, E., Agresta, F. et al. Should enhanced recovery after surgery (ERAS) pathways be preferred over standard practice for patients undergoing abdominal wall reconstruction? A systematic review and meta-analysis. Hernia 25, 501–521 (2021). https://doi.org/10.1007/s10029-020-02262-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02262-y