Abstract
Purpose
Antibiotic prophylaxis in inguinal hernia repair (IHR) is contentious in literature and practice. In low-risk patients, for whom evidence suggests antibiotic prophylaxis is unnecessary, many surgeons still advocate for its routine use. This study surveys prescription patterns of Department of Defense (DoD) general surgeons.
Methods
An anonymous survey was sent electronically to approximately 350 DoD general surgeons. The survey asked multiple-choice and free text answers about prescribing patterns and knowledge of current evidence for low-risk patients undergoing elective open inguinal hernia repair without mesh (OIHRWOM), open inguinal hernia repair with mesh (OIHRWM), or laparoscopic inguinal hernia repair (LIHR).
Results
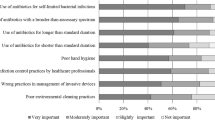
110 DoD general surgeons consented to participate. 58.6, 95 and 84.2% of surgeons always administer antibiotic prophylaxis in OIHRWOM, OIHRWM, and LIHR, respectively. 37.9, 70.9, and 63.2% of surgeons believe that it reduces rates of surgical site infection in OIHRWOM, OIHRWM, and LIHR, respectively. The most common reasons for empirically prescribing antibiotic prophylaxis include “I think the evidence supports it” (27 of 72 responses), “I would rather be conservative and safe” (15 of 72 responses), and “I am following my hospital/department guidelines” (9 of 72 responses).
11.8, 40.8, and 32.9% of surgeons believe current evidence supports antibiotic prophylaxis use in OIHRWM, OIHRWOM, and LIHR, respectively. 50, 18.4, and 22.4% of surgeons believe current evidence refutes antibiotic prophylaxis use in OIHRWM, OIHRWOM, and LIHR, respectively.
Conclusion
The survey results indicate that the majority of practicing DoD general surgeons still empirically prescribe surgical antibiotic prophylaxis in IHR despite more conflicting opinions that it has no meaningful effect or that current evidence does not supports its use.

Similar content being viewed by others
References
Aufenacker TJ, Koelemay MJW, Gouma DJ, Simons MP (2006) Systematic review and meta-analysis of the effectiveness of antibiotic prophylaxis in prevention of wound infection after mesh repair of abdominal wall hernia. Br J Surg 93:5–10. https://doi.org/10.1002/bjs.5186
Sanabria A, Domínguez LC, Valdivieso E, Gómez G (2007) Prophylactic antibiotics for mesh inguinal hernioplasty: a meta-analysis. Ann Surg 245:392–396. https://doi.org/10.1097/01.sla.0000250412.08210.8e
Simons MP, Aufenacker TJ, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, de Lange D, Fortelny RH, Heikkinen T, Kingsnorth A, Kukleta JF, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403. https://doi.org/10.1007/s10029-009-0529-7
Sanchez-Manuel FJ, Lozano-García J, Seco-Gil JL (2012) Antibiotic prophylaxis for hernia repair. Cochrane Database of Syst Rev. https://doi.org/10.1002/14651858.CD003769.pub4
Yin Y, Song T, Liao B, Luo Q, Zhou Z (2012) Antibiotic prophylaxis in patients undergoing open mesh repair of inguinal hernia: a meta-analysis. The Am Surg 78:359–365
Li J-F, Lai D-D, Zhang X-D, Zhang A-M, Sun K-X, Luo H-G, Yu Z (2012) Meta-analysis of the effectiveness of prophylactic antibiotics in the prevention of postoperative complications after tension-free hernioplasty. Can J Surg 55:27–32. https://doi.org/10.1503/cjs.018310
Mazaki T, Mado K, Masuda H, Shiono M (2013) Antibiotic Prophylaxis for the Prevention of Surgical Site Infection after Tension-Free Hernia Repair: A Bayesian and Frequentist Meta-Analysis. J Am Coll Surg 217:788–801.e4. https://doi.org/10.1016/j.jamcollsurg.2013.07.386
Miserez M, Peeters E, Aufenacker T, Bouillot JL, Campanelli G, Conze J, Fortelny R, Heikkinen T, Jorgensen LN, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Simons MP (2014) Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 18:151–163. https://doi.org/10.1007/s10029-014-1236-6
Boonchan T, Wilasrusmee C, McEvoy M, Attia J, Thakkinstian A (2017) Network meta-analysis of antibiotic prophylaxis for prevention of surgical-site infection after groin hernia surgery. Br J Surg 104:e106–e117. https://doi.org/10.1002/bjs.10441
Simons MP, Smietanski M, Bonjer HJ, Bittner R, Miserez M, Aufenacker TJ, Chowbey PK, Tran HM, Sani R, Berrevoet F, Bingener J, Bisgaard T, Bury K, Campanelli G, Chen DC, Conze J, Cuccurullo D, de Beaux AC, Eker HH, Fortelny RH, Gillion JF, van Den Heuvel BJ, Hope WW, Jorgensen LN, Klinge U, Köckerling F, Kukleta JF, Konate I, Liem AL, Lomanto D, Loos MJ, Lopez-Cano M, Misra MC, Montgomery MA, Morales-Conde S, Muysoms FE, Niebuhr H, Nordin P, Pawlak M, van Ramshorst GH, Reinpold WM, Sanders DL, Schouten N, Smedberg S, Simmermacher RK, Tumtavitikul S, van Veenendaal N, Weyhe D, Wijsmuller AR, Jeekel J, Sharma A, Ramshaw B (2018) International guidelines for groin hernia management. Hernia 22:1–165. https://doi.org/10.1007/s10029-017-1668-x
Köckerling F, Bittner R, Jacob D, Schug-Pass C, Laurenz C, Adolf D, Keller T, Stechemesser B (2015) Do we need antibiotic prophylaxis in endoscopic inguinal hernia repair? Results of the Herniamed Registry. Surg Endosc and Other Int Tech 29:3741–3749. https://doi.org/10.1007/s00464-015-4149-2
Schwetling R, Bärlehner E (1998) Is there an indication for general perioperative antibiotic prophylaxis in laparoscopic plastic hernia repair with implantation of alloplastic tissue? Zentralbl Chir 123:193–195
Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ, Fortelny RH, Klinge U, Köckerling F, Kuhry E, Kukleta JF, Lomanto D, Misra MC, Montgomery MA, Morales-Conde S, Reinpold WM, Rosenberg J, Sauerland S, Schug-Paß C, Singh K, Timoney M, Weyhe D, Chowbey PK (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal Hernia [International Endohernia Society (IEHS)]. Surg Endosc and Other Int Tech 25:2773. https://doi.org/10.1007/s00464-011-1799-6
Pasquali S, Boal M, Griffiths EA, Alderson D, Vohra RS (2015) Meta-analysis of perioperative antibiotics in patients undergoing laparoscopic cholecystectomy , on behalf of the CholeS Study Group and the West Midlands Research Collaborative. The British journal of surgery 103:27–34; discussion 34–34; discussion 34. https://doi.org/10.1002/bjs.9904
Aiken AM, Haddow JB, Symons NRA, Kaptanis S, Katz-Summercorn AC, Debnath D, Dent H, Tayeh S, Kung V, Clark S, Gahir J, Dindyal S, Farag S, Lazaridis A, Bretherton CP, Williams S, Currie A, West H, Davies J, Arora S, Kheraj A, Stubbs BM, Yassin N, Mallappa S, Garrett G, Hislop S, Bhangu A, Abbey Y, Al-Shoek I, Ahmad U, Sharp G, Memarzadeh A, Patel A, Ali F, Kaderbhai H, Knowles CH (2013) Use of antibiotic prophylaxis in elective inguinal hernia repair in adults in London and south-east England: a cross-sectional survey. Hernia 17:657–664. https://doi.org/10.1007/s10029-013-1061-3
MacCormick AP, Akoh JA (2018) Survey of Surgeons Regarding Prophylactic Antibiotic Use in Inguinal Hernia Repair. Scand J of Surgery 107:208–211. https://doi.org/10.1177/1457496917748229
Rosenberger LH, Politano AD, Sawyer RG (2011) The surgical care improvement project and prevention of post-operative infection, including surgical site infection. Surg infect 12:163–168. https://doi.org/10.1089/sur.2010.083
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest or financial ties to disclose.
Ethical approval
For this type of study, ethical approval is not required.
Human and animal rights
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
All survey participants gave informed consent to participate in the survey and were allowed to withdraw at any point or withhold answers to questions as desired.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Russell, D., Cole, W., Yheulon, C. et al. USA Department of Defense audit of surgical antibiotic prophylaxis prescribing patterns in inguinal hernia repair. Hernia 25, 159–164 (2021). https://doi.org/10.1007/s10029-020-02145-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02145-2