Abstract
Background
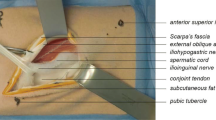
Transabdominal preperitoneal (TAPP) inguinal hernia repair requires the surgeon to have good manual skills in laparoscopic surgery, as well as an understanding of the laparoscopic features of the groin anatomy. This is why TAPP is considered a more difficult surgical procedure compared to open techniques. Realistic training model for TAPP inguinal hernia repair would enhance surgeons’ skills before they enter in the operation room. Our aim was to create a realistic, inexpensive, and easily reproducible model for laparoscopic TAPP inguinal hernia repair and to assess its effectiveness.
Methods
The applied TAPP inguinal hernia repair training simulator consists of a laparoscopic box and an inguinal region model placed in it. The model of the groin area is made of the porcine stomach and assembling materials. Uniaxial tensile and T-peel tests were performed to compare the mechanical properties of the porcine stomach and the human cadaver peritoneum. Thirty eight surgeons performed TAPP inguinal hernia repair using this model. Their opinions were scored on a five-point Likert scale.
Results
Close elastic modules of the porcine and human tissues (13.5 ± 4.2 kPa vs. 15.8 ± 6.7 kPa, p = 0.531) gave to trainees a realistic tissue feel and instrument usage. All participants strongly agreed that model was highly useful for TAPP inguinal hernia repair training. They also put the following points: the model as a whole 5 (3–5), simulation of anatomy 5 (3–5), simulation of dissection and mobilization 5 (3–5), and simulation of intracorporeal suture 5 (4–5).
Conclusions
We successfully created a model for TAPP inguinal hernia repair training. The model is made of inexpensive synthetic and biological materials similar to the human tissue. The model is easy to reproduce and can be used in the training programs of surgical residents.


Similar content being viewed by others
References
Andresen K, Friis-Andersen H, Rosenberg J (2016) Laparoscopic repair of primary inguinal hernia performed in public hospitals or low-volume centers have increased risk of reoperation for recurrence. Surg Innov 23:142–147
Trevisonno M, Kaneva P, Watanabe Y, Fried GM, Feldman LS, Andalib A, Vassiliou MC (2015) Current practices of laparoscopic inguinal hernia repair: a population-based analysis. Hernia 19:725–733
Vu JV, Gunaseelan V, Krapohl GL, Englesbe MJ, Campbell DA, Dimick JB, Telem DA (2018) Surgeon utilization of minimally invasive techniques for inguinal hernia repair: a population-based study. Surg Endosc. https://doi.org/10.1007/s00464-018-6322-x
Trevisonno M, Kaneva P, Watanabe Y, Fried GM, Feldman LS, Lebedeva E, Vassiliou MC (2015) A survey of general surgeons regarding laparoscopic inguinal hernia repair: practice patterns, barriers, and educational needs. Hernia 19:719–724
Suguita Fabio Yuji, Essu FF, Oliveira LT, Iuamoto LR, Kato JM, Torsani MB, Franco AS, Meyer A, Andraus W (2017) Learning curve takes 65 repetitions of totally extraperitoneal laparoscopy on inguinal hernias for reduction of operating time and complications. Surg Endosc 31:3939–3945
Leblanc F, Champagne BJ, Augestad KM, Neary PC, Senagore AJ, Ellis CN, Delaney CP (2010) A comparison of human cadaver and augmented reality simulator models for straight laparoscopic colorectal skills acquisition training. J Am Coll Surg 211:250–255
Nishihara Y, Isobe Y, Kitagawa Y (2017) Validation of newly developed physical laparoscopy simulator in transabdominal preperitoneal (TAPP) inguinal hernia repair. Surg Endosc 31:5429–5435
Sharma M, Horgan A (2012) Comparison of fresh-frozen cadaver and high-fidelity virtual reality simulator as methods of laparoscopic training. World J Surg 36:1732–1737
Yiasemidou M, Roberts D, Glassman D, Tomlinson J, Biyani S, Miskovic D (2017) A multispecialty evaluation of thiel cadavers for surgical training. World J Surg 41:1201–1207
The Herniasurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165
Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ, Fortelny RH, Klinge U, Kockerling F, Kuhry E, Kukleta J, Lomanto D, Misra MC, Montgomery A, Reinpold W, Rosenberg J, Sauerland S, Singh K, Timoney M, Weyhe D, Chowbey P (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc 25:2773–2843
Bittner R, Montgomery MA, Arregui E, Bansal V, Bingener J, Bisgaard T, Buhck H, Dudai M, Ferzli GS, Fitzgibbons RJ, Fortelny RH, Grimes KL, Klinge U, Koeckerling F, Kumar S, Kukleta J, Lomanto D, Misra MC, Morales-Conde S, Reinpold W, Rosenberg J, Singh K, Timoney M, Weyhe D, Chowbey P (2015) Update of guidelines on laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia (International Endohernia Society). Surg Endosc 29:289–321
Lorenz R, Stechemesser B, Reinpold W, Fortelny R, Mayer F, Schröder W, Köckerling F (2017) Development of a standardized curriculum concept for continuing training in hernia surgery: German Hernia School. Hernia 21(2):153–162
Kurashima Y, Feldman L, Al-Sabah S, Kaneva P, Fried G, Vassiliou M (2011) A novel low-cost simulator for laparoscopic inguinal hernia repair. Surg Innov 18:171–175
Hoops HE, Maynard E, Brasel KJ (2017) Training surgeons in the current US Healthcare System : a review of recent changes in resident education. Curr Surg Reports. https://doi.org/10.1007/s40137-017-0195-0
Kurashima Y, Feldman LS, Kaneva PA, Fried GM, Bergman S, Demyttenaere SV, Li C, Vassiliou MC (2014) Simulation-based training improves the operative performance of totally extraperitoneal (TEP) laparoscopic inguinal hernia repair: a prospective randomized controlled trial. Surg Endosc 28:783–788
Schlottmann F, Murty NS, Patti MG (2017) Simulation model for laparoscopic foregut surgery: the University of North Carolina foregut model. J Laparoendosc Adv Surg Tech 27:1–5
Kurashima Y, Feldman LS, Al-Sabah S, Kaneva PA, Fried GM, Vassiliou MC (2011) A tool for training and evaluation of laparoscopic inguinal hernia repair: the Global Operative Assessment of Laparoscopic Skills-Groin Hernia (GOALS-GH). Am J Surg 201:54–61
Lee JS, Hong TH (2015) In vivo porcine training model for laparoscopic Roux-en-Y choledochojejunostomy. Ann Surg Treat Res 88:306–310
Kim EY, Hong TH (2018) In vivo porcine training model of laparoscopic common bile duct repair with T-tube insertion under the situation of iatrogenic common bile duct injury. Ann Surg Treat Res 94:142–146
White EJ, Cunnane EM, Mcmahon M, Walsh MT, Coffey JC, Sullivan LO (2018) Mechanical characterisation of porcine non-intestinal colorectal tissues for innovation in surgical instrument design. J Eng Med 232:796–806
The HerniaSurg Group (2018) International guidelines for groin hernia management. Hernia 22:1–165. https://doi.org/10.1007/s10029-017-1668-x
Köckerling F (2018) What is the influence of simulation-based training courses, the learning curve, supervision, and surgeon volume on the outcome in hernia repair? A Systematic Review. Front Surg. 5:57. https://doi.org/10.3389/fsurg.2018.00057(Published online 25 Sep 2018)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Georgy Ivakhov, Alexey Kolygin, Svetlana Titkova, Michail Anurov, and Alexander Sazhin have no conflicts of interest or financial ties to disclose.
Ethical approval
The study was approved by the institutional Ethics Committee of Pirogov Russian National Research Medical University.
Human and animal rights
This article does not contain any studies with human participants. No procedures were performed on animals in this study.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary file1 (MOV 124223 kb)
Rights and permissions
About this article
Cite this article
Ivakhov, G., Kolygin, A., Titkova, S. et al. Development and evaluation of a novel simulation model for transabdominal preperitoneal (TAPP) inguinal hernia repair. Hernia 24, 159–166 (2020). https://doi.org/10.1007/s10029-019-02032-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-019-02032-5