Abstract
Aim
Enhanced recovery programmes (ERPs) were developed to improve the patient’s post-operative comfort and reduce post-operative morbidity after several types of major surgery including the incisional hernia repair. The aim of this review was to describe the features of ERPs in the setting for incisional hernia repair.
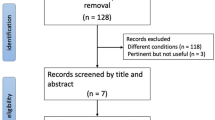
Methods
The literature review was conducted until March 2019, but retrieved very few papers (n = 4) on this topic. All studies were retrospective.
Results
Setting and comorbidities of incisional hernia patients are of such importance in many cases that prehabilitation (including tobacco use cessation, management of obesity, diabetes or malnutrition) should play a greater role compared with other specialties. The other peri-operative measures are similar to other specialties but their implementation was very heterogeneous in the published studies.
Conclusions
Like in other surgeries, ERPs were feasible and probably efficient to improve the post-operative course of incisional hernia patients. But the level of evidence remains low.
Similar content being viewed by others
References
Scott MJ, Baldini G, Fearon KC, Feldheiser A, Feldman LS, Gan TJ, Ljungqvist O, Lobo DN, Rockall TA, Schricker T, Carli F (2005) Enhanced recovery after surgery (ERP) for gastrointestinal surgery, part 1: pathophysiological considerations. Acta Anaesthesiol Scand 59:1212–1231
Ljungqvist O, Scott M, Fearon KC (2017) Enhanced recovery after surgery: a review. JAMA Surg 152:292–298
Fayezizadeh M, Petro CC, Rosen MJ, Novitsky YW (2014) Enhanced recovery after surgery pathway for abdominal wall reconstruction: pilot study and preliminary outcomes. Plast Reconstr Surg 34(4 Suppl 2):S151-9S
Slim K (2016) The benefits of enhanced recovery after surgery. J Visc Surg 153(6S):S41-4
Holihan JL, Alawadi ZM, Harris JW, Harvin J, Shah SK, Goodenough CJ, Kao LS, Liang MK, Roth JS, Walker PA, Ko TC (2016) Ventral hernia: Patient selection, treatment, and management. Curr Probl Surg 53:307–354
Liang MK, Holihan JL, Itani K, Alawadi ZM, Gonzalez JR, Askenasy EP, Ballecer C, Chong HS, Goldblatt MI, Greenberg JA, Harvin JA, Keith JN, Martindale RG, Orenstein S, Richmond B, Roth JS, Szotek P, Towfigh S, Tsuda S, Vaziri K, Berger DH (2017) Ventral hernia management: expert consensus guided by systematic review. Ann Surg 265:80–89
Petro CC, Prabhu AS (2018) Preoperative planning and patient optimization. Surg Clin North Am 98:483–497
Majumder A, Fayezizadeh M, Neupane R, Elliott HL, Novitsky YW (2016) Benefits of multimodal enhanced recovery pathway in patients undergoing open ventral hernia repair. J Am Coll Surg 222:1106–1115
Stearns E, Plymale MA, Davenport DL, Totten C, Carmichael SP, Tancula CS, Roth JS (2018) Early outcomes of an enhanced recovery protocol for open repair of ventral hernia. Surg Endosc 32:2914–2922
Jensen KK, Dressler J, Baastrup NN, Kehlet H, Jørgensen LN (2018) Enhanced recovery after abdominal wall reconstruction reduces length of postoperative stay: An observational cohort study. Surgery. https://doi.org/10.1016/j.surg.2018.07.035
Macedo FIB, Mittal VK (2017) Does enhanced recovery pathways affect outcomes in open ventral hernia repair? Hernia 21:817–818
Le Roy B, Selvy M, Slim K (2016) The concept of prehabilitation: what the surgeon needs to know. J Visc Surg 153:109–112
Liang MK, Bernardi K, Holihan JL, Cherla DV, Escamilla R, Lew DF, Berger DH, Ko TC, Kao LS (2018) Modifying risks in ventral hernia patients with prehabilitation: a randomized controlled trial. Ann Surg 268:674–680
Lovecchio F, Farmer R, Souza J, Khavanin N, Dumanian GA, Kim JY (2014) Risk factors for 30-day readmission in patients undergoing ventral hernia repair. Surgery 155:702–710
Kubasiak JC, Landin M, Schimpke S, Poirier J, Myers JA, Millikan KW, Luu MB (2017) The effect of tobacco use on outcomes of laparoscopic and open ventral hernia repairs: a review of the NSQIP dataset. Surg Endosc 31:2661–2666
Fischer JP, Wink JD, Tuggle CT, Nelson JA, Kovach SJ (2015) Wound risk assessment in ventral hernia repair: generation and internal validation of a risk stratification system using the ACS-NSQIP. Hernia 19:103–111
Dronge AS, Perkal MF, Kancir S, Concato J, Aslan M, Rosenthal RA (2006) Long-term glycemic control and postoperative infectious complications. Arch Surg 141:375–380
Kudsk KA, Tolley EA, DeWitt RC, Janu PG, Blackwell AP, Yeary S, King BK (2003) Preoperative albumin and surgical site identify surgical risk for major postoperative complications. JPEN J Parenter Enteral Nutr 27:1–9
Heard RSM, Ramsay G, Hildebrand DR (2017) Sarcopaenia in surgical populations: a review. Surgeon 15:366–371
Chambrier C, Sztark F (2012) French clinical guidelines on perioperative nutrition: Update of the 1994 consensus conference on perioperative artificial nutrition for elective surgery in adults. J Visc Surg 149:e325-36
Maurice-Szamburski A, Auquier P, Viarre-Oreal V, Cuvillon P, Carles M, Ripart J, Honore S, Triglia T, Loundou A, Leone M, Bruder N, PremedX Study Investigators (2015) Effect of sedative premedication on patient experience after general anesthesia: a randomized clinical trial. JAMA 313:916–925
Venclauskas L, Llau JV, Jenny JY, Kjaersgaard-Andersen P, Jans Ø, ESA VTE Guidelines Task Force (2018) European guidelines on perioperative venous thromboembolism prophylaxis: day surgery and fast-track surgery. Eur J Anaesthesiol 35:134–138
Venclauskas L, Maleckas A, Arcelus JI (2017) European guidelines on perioperative venous thromboembolism prophylaxis: surgery in the obese patient. Eur J Anaesthesiol 35:147–153
Sarin A, Chen LL, Wick EC (2017) Enhanced recovery after surgery-Preoperative fasting and glucose loading—a review. J Surg Oncol 116:578–582
Kleppe KL, Greenberg JA (2018) Enhanced recovery after surgery protocols: rationale and components. Surg Clin North Am 98:499–509
Jensen KK (2018) Epidural analgesia in patients undergoing elective ventral hernia repair? Ann Surg 1:1. https://doi.org/10.1097/SLA.0000000000002906
Fischer JP, Nelson JA, Wes AM, Wink JD, Yan C, Braslow BM, Chen L, Kovach SJ (2014) The use of epidurals in abdominal wall reconstruction: an analysis of outcomes and cost. Plast Reconstr Surg 133:687–699
Karamanos E, Dream S, Falvo A, Schmoekel N, Siddiqui A (2017) Use of epidural analgesia as an adjunct in elective abdominal wall reconstruction: a review of 4983 cases. Perm J. https://doi.org/10.7812/TPP/16-115
Prabhu AS, Krpata DM, Perez A, Phillips S, Huang LC, Haskins IN, Rosenblatt S, Poulose BK, Rosen MJ (2018) Is it time to reconsider postoperative epidural analgesia in patients undergoing elective ventral hernia repair? An AHSQC analysis. Ann Surg 267:971–976
Helander EM, Billeaud CB, Kline RJ, Emelife PI, Harmon CM, Prabhakar A, Urman RD, Kaye AD (2017) Multimodal approaches to analgesia in enhanced recovery after surgery pathways. Int Anesthesiol Clin 55:51–69
Warren JA, Carbonell AM, Jones LK, Mcguire A, Hand WR, Cancellaro VA, Ewing JA, Cobb WS (2019) Length of stay and opioid dose requirement with transversus abdominis plane block vs epidural analgesia for ventral hernia repair. J Am Coll Surg 228:680–686
Warren JA, Stoddard C, Hunter AL, Horton AJ, Atwood C, Ewing JA, Pusker S, Cancellaro VA, Walker KB, Cobb WS, Carbonell AM, Morgan RR (2017) Effect of multimodal analgesia on opioid use after open ventral hernia repair. J Gastrointest Surg 21:1692–1699
Sebranek JJ, Lugli AK, Coursin DB (2013) Glycaemic control in the perioperative period. Br J Anaesth 111(Suppl 1):i18-34
Biedrzycka A, Lango R (2016) Tissue oximetry in anaesthesia and intensive care. Anaesthesiol Intensive Ther 48:41–48
Ireland CJ, Chapman TM, Mathew SF, Herbison GP, Zacharias M (2014) Continuous positive airway pressure (CPAP) during the postoperative period for prevention of postoperative morbidity and mortality following major abdominal surgery. Cochrane Database Syst Rev. 8:CD008930
Rothman JP, Gunnarsson U, Bisgaard T (2014) Abdominal binders may reduce pain and improve physical function after major abdominal surgery—a systematic review. Dan Med J 61:A4941
Christoffersen MW, Olsen BH, Rosenberg J, Bisgaard T (2015) Randomized clinical trial on the postoperative use of an abdominal binder after laparoscopic umbilical and epigastric hernia repair. Hernia 19:147–153
Slim K, Theissen A, Raucoules-Aimé M, Fédération de chirurgie viscérale et digestive (FCVD), French-speaking Group for Improved Rehabilitation after Surgery (GRACE) (2016) Risk management in ambulatory and short-stay gastrointestinal surgery. J Visc Surg 153:55-60
Funding
There is no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KS and DS declare no conflict of interest related to this paper.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Slim, K., Standaert, D. Enhanced recovery after surgical repair of incisional hernias. Hernia 24, 3–8 (2020). https://doi.org/10.1007/s10029-019-01992-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-019-01992-y