Abstract
Background
Single-incision laparoscopic surgery has been developed with the objective to reduce surgical trauma, decrease associated surgical stress and to improve cosmetic outcome. However, concerns have been raised regarding the risk of trocar-site hernia following this approach. Previous meta-analyses have suggested a trend toward higher hernia rates, but have failed to demonstrate a significant difference between single-incision and conventional laparoscopic surgery.
Method
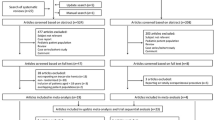
Medline, AMED, CINAHL and CENTRAL were searched up to May 2014. Randomized controlled trials comparing single-incision and conventional laparoscopic surgery were considered for inclusion. Studies with patients aged less than 18 years and those reporting on robotic surgery were disregarded. Pooled odds ratios with 95 % confidence intervals were calculated to measure the comparative risk of trocar-site hernia following single-incision and conventional laparoscopic surgery.
Results
Nineteen randomized trials encompassing 1705 patients were included. Trocar-site hernia occurred in 2.2 % of patients in the single-incision group and in 0.7 % of patients in the conventional laparoscopic surgery group (odds ratio 2.26, 95 % confidence interval 1.00–5.08, p = 0.05). Sensitivity analysis of quality randomized trials validated the outcome estimates of the primary analysis. There was no heterogeneity among studies (I 2 = 0 %) and no evidence of publication bias.
Conclusion
Single-incision laparoscopic surgery involving entry into the peritoneal cavity through the umbilicus is associated with a slightly higher risk of trocar-site hernia than conventional laparoscopy. Its effect on long-term morbidity and quality of life is a matter for further investigation.





Similar content being viewed by others
References
Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I (1997) One-wound laparoscopic cholecystectomy. Br J Surg 84:695
Antoniou SA, Pointner R, Granderath FA (2011) Single-incision laparoscopic cholecystectomy: a systematic review. Surg Endosc 25:367–377
Arezzo A, Scozzari G, Famiglietti F, Passera R, Morino M (2013) Is single incision laparoscopic cholecystectomy safe? Results of a systematic review and meta-analysis. Surg Endosc 27:2293–2304
Garg P, Thakur JD, Garg M, Menon GR (2012) Single incision laparoscopic cholecystectomy vs. conventional laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials. J Gastrointest Surg 16:1618–1628
Geng L, Sun C, Bai J (2013) Single incision versus conventional laparoscopic cholecystectomy outcomes: a meta-analysis of randomized controlled trials. PLoS One 8:e76530
Hao L, Liu M, Zhu H, Li Z (2012) Single-incision versus conventional laparoscopic cholecystectomy in patients with uncomplicated gallbladder disease: a meta-analysis. Surg Laparosc Endosc Percutan Tech 22:487–497
Markar SR, Karthikesalingam A, Thrumurthy S, Muirhead L, Kinross J, Paraskeva P (2012) Single incision laparoscopic surgery (SILS) vs. conventional multiport cholecystectomy: systematic review and meta-analysis. Surg Endosc 26:1205–1213
Pisanu A, Reccia I, Porceddu G, Uccheddu A (2012) Meta-analysis of prospective randomized studies comparing single incision laparoscopic cholecystectomy (SILC) and conventional multiport laparoscopic cholecystectomy (CMLC). J Gastrointest Surg 16:1790–1801
Qiu J, Yuan H, Chen S, He Z, Han P, Wu H (2013) Single-port versus conventional multiport laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials and nonrandomized studies. J Laparoendosc Adv Surg Tech A 23:815–831
Sajid MS, Ladwa N, Kalra L, Hutson KK, Singh KK, Sayegh M (2012) Single incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy: meta-analysis and systematic review of randomized controlled trials. World J Surg 36:2644–2653
Wang D, Wang Y, Ji ZL (2012) Laparoendoscopic single-site cholecystectomy versus conventional laparoscopic cholecystectomy: a systematic review of randomized controlled trials. ANZ J Surg 82:303–310
Wang Z, Huang X, Zheng Q (2012) Single incision versus conventional laparoscopic cholecystectomy: a meta-analysis. ANZ J Surg 82:885–889
Wu XS, Shi LB, Gu J, Dong P, Lu JH, Li ML, Mu JS, Wu WG, Yang JH, Ding QC, Zhang L, Liu YB (2013) Single incision laparoscopic cholecystectomy versus multi-incision laparoscopic cholecystectomy: a meta-analysis of randomized clinical trials. J Laparoendosc Adv Surg Tech A 23:183–191
Milas M, Deveđija S, Trkulja V (2014) Single incision versus standard multiport laparoscopic cholecystectomy: up-dated systematic review and meta-analysis of randomized trials. Surgeon. doi:10.1016/j.surge.2014.01.009
Bingener J, Ghahfarokhi LS, Skaran P, Sloan J (2013) Responsiveness of quality of life instruments for the comparison of minimally invasive cholecystectomy procedures. Surg Endosc 27:2446–2453
Trastulli S, Cirocchi R, Desiderio J, Guarino S, Santoro A, Parisi A, Noya G, Boselli C (2013) Systematic review and meta-analysis of randomized clinical trials comparing single-incision versus conventional laparoscopic cholecystectomy. Br J Surg 100:191–208
Joseph M, Phillips MR, Farrell TM, Rupp CC (2012) Single incision laparoscopic cholecystectomy is associated with a higher bile duct injury rate: a review and a word of caution. Ann Surg 256:1–6
Muysoms FE, Antoniou SA, Bury K, Campanelli G, Conze J, Cuccurullo D, de Beaux AC, Deerenberg EB, East BE, Fortelny RH, Gillion JF, Henriksen NH, Israelsson L, Jairam A, Jänes A, Jeekel J, Lopez-Cano M, Miserez M, Morales-Conde S, Sanders D, Simons MP, Śmietański M, Venclauskas L, Berrevoet F (2014) European Hernia Society guidelines on the closure of abdominal wall incisions. Hernia. doi:10.1007/s10029-014-1342-5
Erdas E, Dazzi C, Secchi F, Aresu S, Pitzalis A, Barbarossa M, Garau A, Murgia A, Contu P, Licheri S, Pomata M, Farina G (2012) Incidence and risk factors for trocar site hernia following laparoscopic cholecystectomy: a long-term follow-up study. Hernia 16:431–437
Bunting DM (2010) Port-site hernia following laparoscopic cholecystectomy. JSLS 14:490–497
Helgstrand F, Rosenberg J, Bisgaard T (2011) Trocar site hernia after laparoscopic surgery: a qualitative systematic review. Hernia 15:113–121
University of York, Centre for Reviews and Dissemination. PROSPERO; International Prospective Register of systematic reviews. http://www.crd.york.ac.uk/PROSPERO/. Accessed April 2014
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. BMJ 339:b2700
SIGN Methodology Checklist 2: Controlled Trials. http://www.sign.ac.uk/methodology/checklists/20121206_Checklist_for_controlled_trials.doc. Accessed April 2014
Higgins JP, Altman DG (2009) Assessing risk of bias in included studies. In: Higgins JP, Green S (eds) Cochrane handbook for systematic reviews of interventions. Wiley, West Sussex, pp 187–235
Abd Ellatif ME, Askar WA, Abbas AE, Noaman N, Negm A, El-Morsy G, El Nakeeb A, Magdy A, Amin M (2013) Quality-of-life measures after single-access versus conventional laparoscopic cholecystectomy: a prospective randomized study. Surg Endosc 27:1896–1906
Zapf M, Yetasook A, Leung D, Salabat R, Denham W, Barrera E, Butt Z, Carbray J, Du H, Wang CE, Ujiki M (2013) Single-incision results in similar pain and quality of life scores compared with multi-incision laparoscopic cholecystectomy: a blinded prospective randomized trial of 100 patients. Surgery 154:662–670 Discussion 670–671
Carter JT, Kaplan JA, Nguyen JN, Lin MY, Rogers SJ, Harris HW (2014) A Prospective, randomized controlled trial of single-incision laparoscopic vs conventional 3-port laparoscopic appendectomy for treatment of acute appendicitis. J Am Coll Surg 218:950–959
Jørgensen LN, Rosenberg J, Al-Tayar H, Assaadzadeh S, Helgstrand F, Bisgaard T (2014) Randomized clinical trial of single-versus multi-incision laparoscopic cholecystectomy. Br J Surg 101:347–355
Villalobos Mori R, Escoll Rufino J, Herrerías González F, Mias Carballal MC, Escartin Arias A, Olsina Kissler JJ (2014) Prospective, randomized comparative study between single-port laparoscopic appendectomy and conventional laparoscopic appendectomy. Cir Esp. doi:10.1016/j.ciresp.2013.12.013 Article in English, Spanish, Epub ahead of print
Ma J, Cassera MA, Spaun GO, Hammill CW, Hansen PD, Aliabadi-Wahle S (2011) Randomized controlled trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. Ann Surg 254:22–27
Herrero Fonollosa E, Cugat Andorrà E, García Domingo MI, Camps Lasa J, Porta Castejón R, Carvajal López F, Rodríguez Campos A (2012) A randomised prospective comparative study between laparoscopic cholecystectomy and single port cholecystectomy in a major outpatient surgery unit. Cir Esp 90:641–646
Leung D, Yetasook AK, Carbray J, Butt Z, Hoeger Y, Denham W, Barrera E, Ujiki MB (2012) Single-incision surgery has higher cost with equivalent pain and quality-of-life scores compared with multiple-incision laparoscopic cholecystectomy: a prospective randomized blinded comparison. J Am Coll Surg 215:702–708
Noguera JF, Cuadrado A, Dolz C, Olea JM, García JC (2012) Prospective randomized clinical trial comparing laparoscopic cholecystectomy and hybrid natural orifice transluminal endoscopic surgery (NOTES) (NCT00835250). Surg Endosc 26:3435–3441
Zheng M, Qin M, Zhao H (2012) Laparoendoscopic single-site cholecystectomy: a randomized controlled study. Minim Invasive Ther Allied Technol 21:113–117
Khorgami Z, Shoar S, Anbara T, Soroush A, Nasiri S, Movafegh A, Aminian A (2014) A randomized clinical trial comparing 4-port, 3-port, and single-incision laparoscopic cholecystectomy. J Invest Surg 27:147–154
Marks JM, Phillips MS, Tacchino R, Roberts K, Onders R, DeNoto G, Gecelter G, Rubach E, Rivas H, Islam A, Soper N, Paraskeva P, Rosemurgy A, Ross S, Shah S (2013) Single-incision laparoscopic cholecystectomy is associated with improved cosmesis scoring at the cost of significantly higher hernia rates: 1-year results of a prospective randomized, multicenter, single-blinded trial of traditional multiport laparoscopic cholecystectomy vs single-incision laparoscopic cholecystectomy. J Am Coll Surg 216:1037–1047 Discussion 1047–1048
Noguera J, Tejada S, Tortajada C, Sánchez A, Muñoz J (2013) Prospective, randomized clinical trial comparing the use of a single-port device with that of a flexible endoscope with no other device for transumbilical cholecystectomy: LLATZER-FSIS pilot study. Surg Endosc 27:4284–4290
Saad S, Strassel V, Sauerland S (2013) Randomized clinical trial of single-port, minilaparoscopic and conventional laparoscopic cholecystectomy. Br J Surg 100:339–349
Bucher P, Pugin F, Buchs NC, Ostermann S, Morel P (2011) Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br J Surg 98:1695–1702
Sinan H, Demirbas S, Ozer MT, Sucullu I, Akyol M (2012) Single-incision laparoscopic cholecystectomy versus laparoscopic cholecystectomy: a prospective randomized study. Surg Laparosc Endosc Percutan Tech 22:12–16
Solomon D, Shariff AH, Silasi DA, Duffy AJ, Bell RL, Roberts KE (2012) Transvaginal cholecystectomy versus single-incision laparoscopic cholecystectomy versus four-port laparoscopic cholecystectomy: a prospective cohort study. Surg Endosc 26:2823–2827
Vilallonga R, Barbaros U, Sümer A, Demirel T, Fort JM, González O, Rodriguez N, Carrasco MA (2012) Single-port transumbilical laparoscopic cholecystectomy: a prospective randomised comparison of clinical results of 140 cases. J Minim Access Surg 8:74–78
Madureira FA, Manso JE, Madureira Fo D, Iglesias AC (2013) Randomized clinical study for assessment of incision characteristics and pain associated with LESS versus laparoscopic cholecystectomy. Surg Endosc 27:1009–1115
Beck C, Eakin J, Dettorre R, Renton D (2013) Analysis of perioperative factors and cost comparison of single-incision and traditional multi-incision laparoscopic cholecystectomy. Surg Endosc 27:104–108
Sherwinter DA (2010) Transitioning to single-incision laparoscopic inguinal herniorrhaphy. JSLS 14:353–357
Weiss HG, Brunner W, Biebl MO, Schirnhofer J, Pimpl K, Mittermair C, Obrist C, Brunner E, Hell T (2014) Wound complications in 1145 consecutive transumbilical single-incision laparoscopic procedures. Ann Surg 259:89–95
Nakajima K, Wasa M, Kawahara H, Hasegawa T, Soh H, Taniguchi E, Ohashi S, Okada A (1999) Revision laparoscopy for incarcerated hernia at a 5-mm trocar site following pediatric laparoscopic surgery. Surg Laparosc Endosc Percutan Tech 9:294–295
Backman T, Arnbjörnsson E, Kullendorff CM (2005) Omentum herniation at a 2-mm trocar site. J Laparoendosc Adv Surg Tech A 15:87–88
Yee DS, Duel BP (2006) Omental herniation through a 3-mm umbilical trocar site. J Endourol 20:133–134
Clark LH, Soliman PT, Odetto D, Munsell MF, Schmeler KM, Fleming N, Westin SN, Nick AM, Ramirez PT (2013) Incidence of trocar site herniation following robotic gynecologic surgery. Gynecol Oncol 131:400–403
Schmedt CG, Leibl BJ, Däubler P, Bittner R (2001) Access-related complications—an analysis of 6023 consecutive laparoscopic hernia repairs. Min Invas Ther Allied Technol 10:23–30
Chiu CC, Lee WJ, Wang W, Wei PL, Huang MT (2006) Prevention of trocar-wound hernia in laparoscopic bariatric operations. Obes Surg 16:913–918
Coda A, Bossotti M, Ferri F et al (2000) Incisional hernia and fascial defect following laparoscopic surgery. Surg Laparosc Endosc Percutan Tech 10:34–38
Nassar AH, Ashkar KA, Rashed AA, Abdulmoneum MG (1997) Laparoscopic cholecystectomy and the umbilicus. Br J Surg 84:630–633
Yamamoto M, Minikel L, Zaritsky E (2011) Laparoscopic 5-mm trocar site herniation and literature review. JSLS 15:122–126
Mayol J, Garcia-Aguilar J, Ortiz-Oshiro E, De-Diego Carmona JA, Fernandez-Represa JA (1997) Risks of the minimal access approach for laparoscopic surgery: multivariate analysis of morbidity related to umbilical trocar insertion. World J Surg 21:529–533
Acknowledgments
The authors wish to thank Dr. Alexandros Andreou for translation of articles from the Spanish language. The contribution of Ms. Angeliki Zachou, clinical librarian at the Papageorgiou University Hospital of Thessaloniki is greatly acknowledged.
Conflict of interest
SAA declares no conflict of interest. SMC declares no conflict of interest. GAA declares no conflicts of interest. FAA declares no conflict of interest. FB declares conflict of interest not directly related to the submitted work. FEM declares conflict of interest not directly related to the submitted work. ACB declares conflict of interest not directly related to the submitted work. KB declares no conflict of interest. MLC declares conflict of interest not directly related to the submitted work. DC declares conflict of interest not directly related to the submitted work. EBD declares conflict of interest not directly related to the submitted work. BEE declares no conflict of interest. RHF declares conflict of interest not directly related to the submitted work. JFG declares conflict of interest not directly related to the submitted work. NAH declares no conflict of interest. MM declares conflict of interest not directly related to the submitted work. DLS declares conflict of interest not directly related to the submitted work. MPS declares no conflict of interest. LV declares no conflict of interest.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Members of the Bonham Group are listed in “Appendix 1”.
Appendices
Appendix 1
“The Bonham Group” is the European Hernia Society Guidelines Development Group for Guidelines on the closure of abdominal wall incisions:
Andrew C. de Beaux
Kamil Bury
Manuel Lopez-Cano
Diego Cuccurullo
Eva B. Deerenberg
Barbora E. East
Rene H. Fortelny
Jean-Francois Gillion
Nadia A. Henriksen
Marc Miserez
David L. Sanders
Maarten P. Simons
Linas Venclauskas
Appendix 2: Search strategy
1. Hernia
2. Incisional hernia
3. Trocar-site hernia
4. Trocar site hernia
5. Port-site hernia
6. Port site hernia
7. Single-incision
8. Single incision
9. Single-port
10. Single port
11. Single-access
12. Single access
13. One-access
14. One access
15. One-port
16. One port
17. Single-site
18. Single site
19. Laparoscopy
20. Laparoscopic
21. 1 OR 2 OR 3 OR 4 OR 5 OR 6
22. 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18
23. 19 OR 20
Search terms combination: 21 AND 22 AND 23
Rights and permissions
About this article
Cite this article
Antoniou, S.A., Morales-Conde, S., Antoniou, G.A. et al. Single-incision laparoscopic surgery through the umbilicus is associated with a higher incidence of trocar-site hernia than conventional laparoscopy: a meta-analysis of randomized controlled trials. Hernia 20, 1–10 (2016). https://doi.org/10.1007/s10029-015-1371-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-015-1371-8